Heart attacks, a sobering reality in the U.S., occur every 40 seconds, with approximately 805,000 incidents annually. This stark statistic underscores the critical importance of understanding chest pain, a symptom that can often be alarming and ambiguous. Distinguishing between a life-threatening cardiac event and other less severe conditions presents a significant diagnostic challenge for both individuals and medical professionals alike. The body’s signals are multifaceted, and interpreting them accurately is paramount for timely intervention and appropriate care.
While the immediate fear often centers on the heart, the reality is that pain in the chest, shoulder, or neck can arise from an extensive array of sources, some benign, others equally serious but non-cardiac. The human anatomy is intricately linked, meaning discomfort originating in one area can frequently manifest in another, creating a complex web of symptoms that demand careful, informed evaluation. This article aims to disentangle some of these complexities, offering a detailed guide to understanding various pain presentations across these critical regions.
Drawing upon expert medical insights, we will delve into the nuances of these physical sensations, highlighting key differentiators that can help illuminate the underlying causes. From the insidious onset of a heart attack to the more localized strains of musculoskeletal injury, and the referred pains from distant organs, a comprehensive understanding is crucial. Our exploration begins with the most urgent concerns: identifying the characteristics of heart attack pain and separating it from other common forms of chest discomfort.
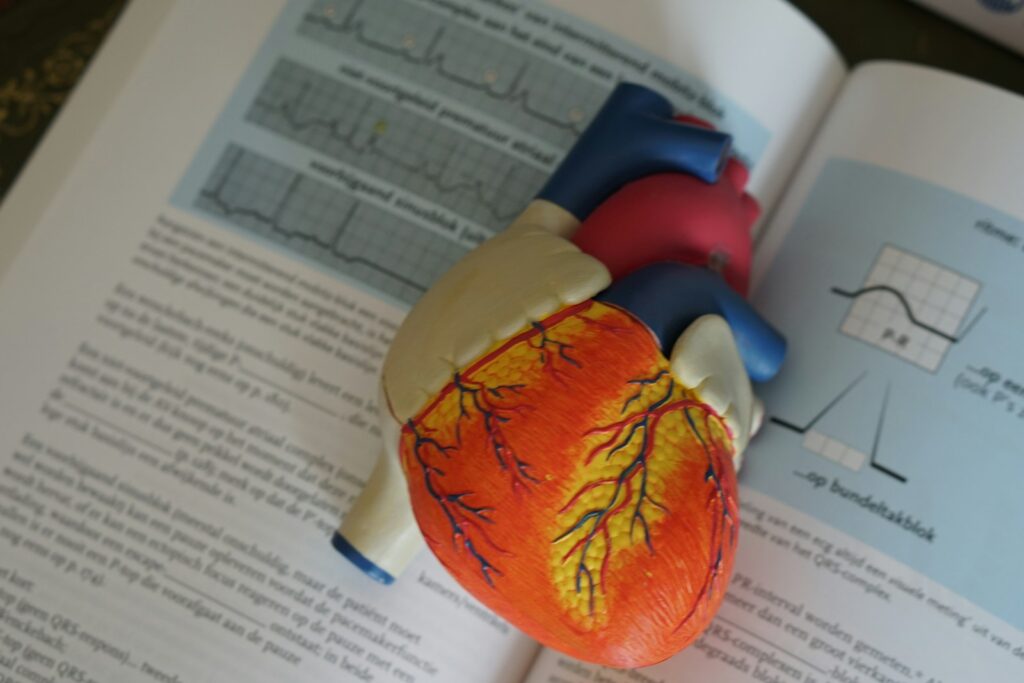
1. **Recognizing Heart Attack Symptoms: Sudden, Persistent Chest Pain and Referred Pain**Heart attacks are frequent, demanding vigilance regarding chest pain. Cardiologist Curtis Rimmerman, MD, describes cardiac pain as “sudden, persistent and not pinpointed to one location,” distinct from localized discomfort. He urges immediate medical attention for any chest pain, particularly for high-risk individuals, stressing, “When in doubt, err on the side of caution and visit a doctor or emergency room immediately.”
Dr. Rimmerman states that “location is overrated” for pinpoint chest pain, warning that delay can cause “loss of functioning heart muscle.” While some experience “silent heart attacks,” pain often covers an area “roughly the size of their fist or larger.” Referred pain may extend to the neck, throat, shoulders, upper back, jaw, and arms, confirming “location is only one factor.”
Serious heart attack pain is sudden, unrelenting, and often accompanied by shortness of breath, fatigue, dizziness, racing heart, cold sweat, or loss of consciousness. Described as “almost as if there is a balloon inside your chest that is expanding,” it builds in a “crescendo pattern” of “unrelenting intense pressure or heaviness.” Symptoms lasting over a few minutes necessitate a 911 call, especially with risk factors like smoking, diabetes, or family history of heart disease.
2. **Differentiating Non-Cardiac Chest Pain: When It’s Not a Heart Attack**Contrary to common fears, most ER chest pain is not cardiac; a study found less than 6% were life-threatening heart issues. This provides crucial context for low-risk individuals to differentiate non-cardiac discomfort. Key indicators distinguish these cases, guiding appropriate responses to various forms of chest pain.
Pain is unlikely cardiac if it is “momentary,” “isolated to one small area,” or changes with body repositioning. These characteristics are significant diagnostic clues. The ability to alleviate or worsen pain through movement strongly suggests a non-cardiac origin, directing assessment towards musculoskeletal or other localized issues.
Sudden, sharp, momentary chest discomfort lasting under two minutes often stems from musculoskeletal causes. Examples include broken ribs, a pulled chest muscle, or inflammation of rib cartilage (costochondritis). Other causes like fibromyalgia or shingles can also trigger sharp chest wall pain before a rash appears. While not heart attacks, such persistent symptoms warrant medical review.

3. **Chest Pain from Lung-Related Issues: Beyond the Heart**Piercing chest pain intensified by movement or deep breaths often signals lung-related problems, not cardiac events. This specific pain exacerbation with respiration serves as a critical diagnostic clue. Such discomfort indicates issues within the respiratory system, demanding prompt medical assessment for accurate identification and treatment.
Lung conditions causing this pain include pneumonia or infections, creating inflammation and sharp discomfort. Pleurisy, inflammation of the lung lining, produces distinct sharp pain worsening with breathing. More serious issues like a pulmonary embolism (blood clot) cause sudden, sharp chest pain with shortness of breath, requiring emergency care.
An asthma attack can also induce chest tightness and piercing pain. Crucially, these lung issues, though not heart attacks, are equally concerning. Ignoring persistent or worsening symptoms can lead to severe health implications. Therefore, seeking immediate medical attention from a healthcare provider or emergency room is strongly advised if symptoms persist or intensify.
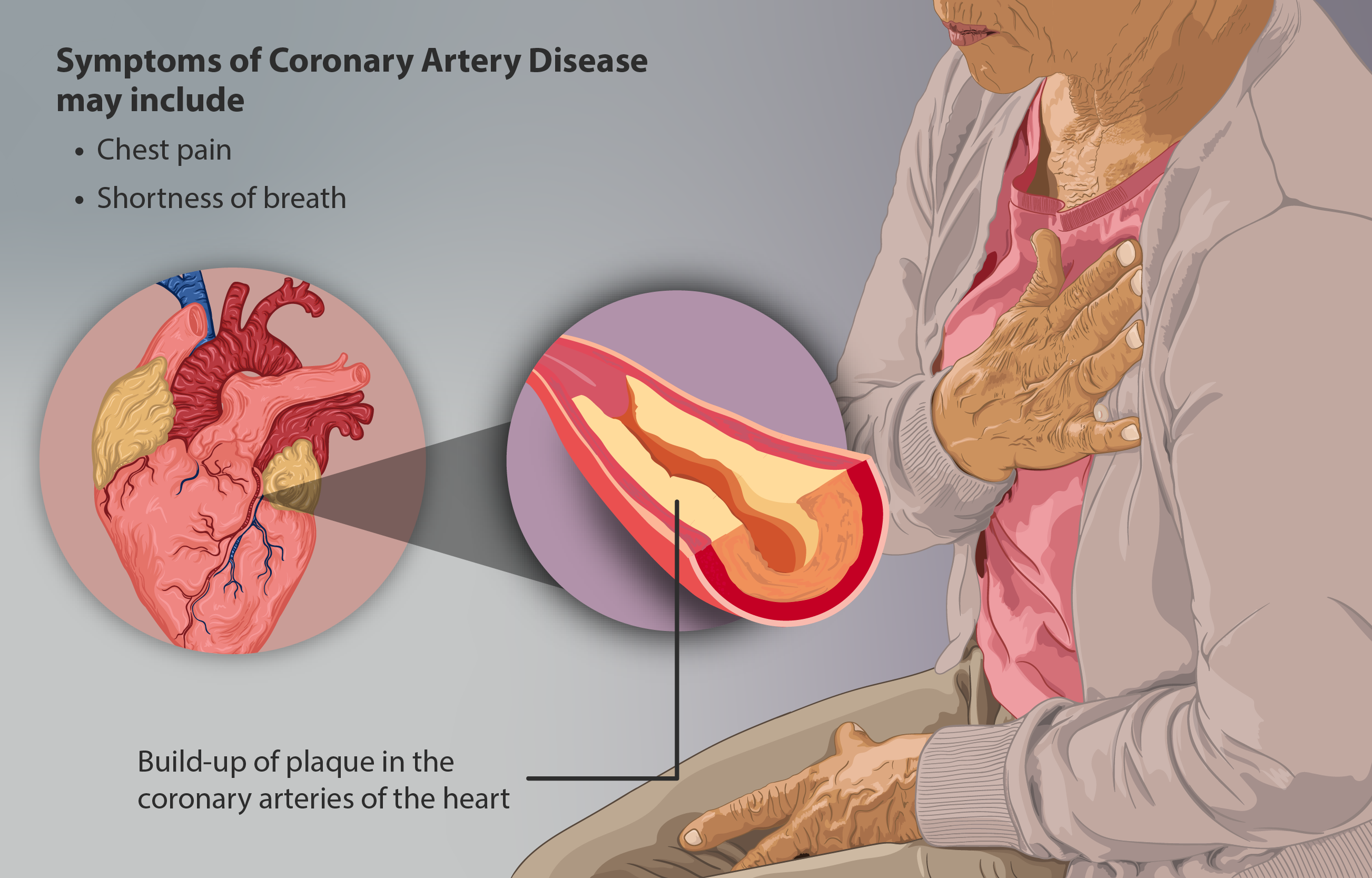
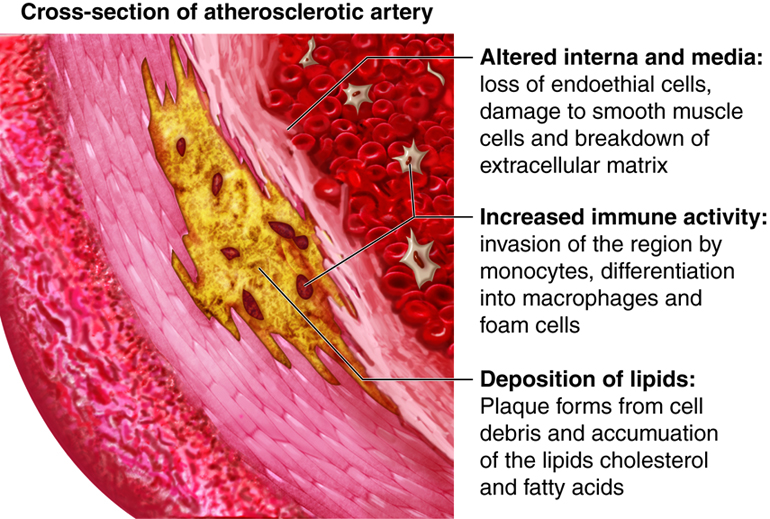
4. **Understanding Angina: A Signal of Coronary Artery Disease**Angina, a symptom of coronary artery disease, indicates the heart muscle lacks sufficient oxygen-rich blood. This chest pain manifests as “a pressure or squeezing sensation,” as per the National Heart, Lung, and Blood Institute. Recognizing angina is a critical warning, necessitating swift medical evaluation to avert more severe cardiac events.
Angina often spreads beyond the chest to the shoulders, neck, and jaw, a characteristic referred pain pattern. This interconnectedness of sensations requires comprehensive symptom assessment for accurate diagnosis. Other symptoms include a “burning or aching in the chest behind the breastbone,” weakness, sweating, and shortness of breath, all pointing to myocardial ischemia.
Treatment combines medications to improve blood flow and reduce heart workload with crucial lifestyle changes. Dietary adjustments, increased physical activity, and stress management are vital for mitigating coronary artery disease progression. This holistic approach enhances cardiovascular health and prevents future complications, emphasizing the importance of integrated care.

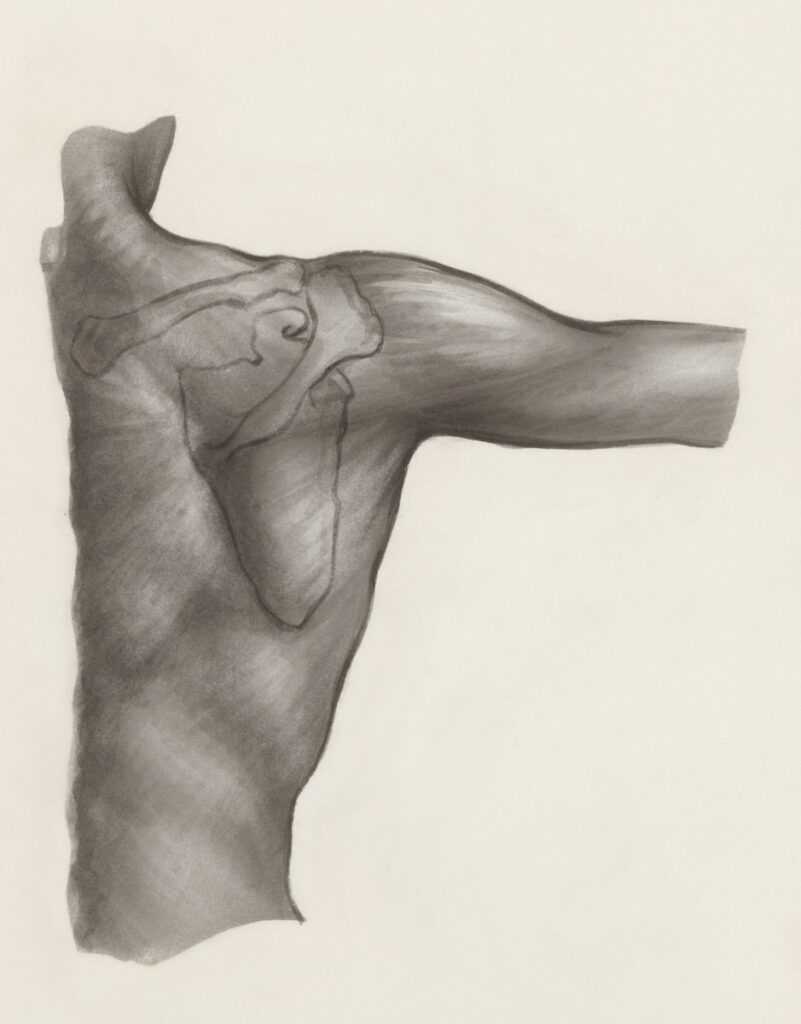
5. **Thoracic Outlet Syndrome: Nerve and Blood Vessel Compression**Thoracic Outlet Syndrome (TOS) describes nerve and blood vessel compression within the thoracic outlet, between the first rib and collarbone. This anatomical constriction becomes problematic when surrounding structures impinge on these vital bundles. Understanding this mechanism is key to diagnosing a condition causing significant discomfort and potential impairment.
TOS can result from neck injuries, repetitive movements, or poor posture, which alter the space in the thoracic outlet. The National Organization for Rare Disorders highlights how these factors can lead to damage or compression. Such impingement can produce diverse symptoms, necessitating a thorough examination.
Symptoms include “pain, tingling, or numbness in the arm, hand, or fingers,” arm swelling or aching, neck pain, headaches, and “pale or white discoloration of the hand and fingers.” Treatment involves over-the-counter anti-inflammatories, thrombolytic drugs for clots, and physical therapy for posture and strength. In severe cases, surgery may be considered for decompression.
6. **Common Front Shoulder Injuries: Bursitis, Tears, and Fractures**The shoulder’s high mobility makes it prone to injuries, particularly affecting the front and side. Understanding these common ailments is crucial for accurate diagnosis and effective treatment, as they significantly impact daily function. These conditions range from inflammation to acute structural damage, each with distinct presentations.
Shoulder bursitis, inflammation of fluid-filled sacs, causes gradual pain that worsens with overhead arm lifting. A SLAP tear involves damage to the labrum cartilage, often from trauma or repetitive overhead activities, leading to clicking or catching sensations. Rotator cuff tears affect tendons, resulting from wear and tear or sudden injury, causing deep aching, especially at night.
Proximal humeral fractures, breaks in the upper arm bone, cause intense front shoulder pain. These high-energy injuries, common in individuals over 60, present with immediate, severe pain and obvious deformity. Accurate identification of these varied front shoulder issues ensures appropriate therapeutic intervention, from conservative care to surgical repair, and optimal recovery.
Navigating the intricate landscape of pain that extends beyond the chest and into the shoulder, neck, and upper back requires a comprehensive understanding of both localized conditions and referred sensations. While the initial focus on potential cardiac emergencies is paramount, a multitude of other factors, from chronic degenerative conditions to systemic illnesses and everyday postural habits, contribute to this complex array of symptoms. This second section endeavors to unravel these further complexities, offering deeper insights into the diverse origins of shoulder, neck, and referred pain.

7. **Neck and Spinal Origins of Referred Shoulder Pain** Pain originating in the cervical and thoracic spine frequently manifests as discomfort in the shoulder region, often leading to diagnostic challenges. As individuals age, the discs and joints within the neck can undergo degenerative changes, resulting in stiffness and pain. This wear and tear can directly irritate nerves, causing sensations that radiate outwards, often perceived as shoulder pain rather than a direct neck issue. The interconnectedness of the spinal column and peripheral nerve pathways means that problems in the neck can intricately influence sensations perceived throughout the upper torso and limbs.
When movement of the head exacerbates shoulder pain, it strongly suggests that the actual problem may lie within the neck rather than the shoulder joint itself. Conditions such as arthritis, disc degeneration, or the narrowing of neural canals within the upper spine (cervical and thoracic regions) can lead to a variety of symptoms. These spinal issues can cause pain that refers across both shoulders, underscoring the importance of evaluating the cervical spine in cases of persistent or unexplained shoulder discomfort.
Nerve pain originating from the neck or spine typically presents as a sharp, burning, or shooting sensation that can travel anywhere from the neck down the arm, potentially extending all the way to the hand. This neural involvement is often accompanied by changes in sensation, such as tingling and numbness, and may also result in weakness in the affected arm. Identifying these specific nerve-related symptoms is crucial for distinguishing spinal or neural impingement from more localized muscular or joint issues in the shoulder.

8. **Chronic and Positional Factors in Shoulder and Neck Discomfort** Everyday habits and long-term postural issues significantly contribute to chronic neck and shoulder pain. Poor posture, particularly hunching over a desk or computer for prolonged periods, strains the muscles in the neck and shoulders, increasing the risk of discomfort. Similarly, repetitive motions, such as typing or using a mouse extensively, can lead to muscle strain and tension that accumulates over time, developing into chronic pain. These occupational and lifestyle factors are often overlooked but are potent drivers of persistent musculoskeletal issues.
Beyond work-related ergonomics, other lifestyle elements play a role. Sleeping in an improper position, such as on the stomach with the head turned to the side for extended periods, or using a pillow that fails to support proper spinal alignment, can cause significant strain. Additionally, engaging in activities requiring repetitive overhead work, like certain household chores or manual labor, can introduce strenuous movements that elevate the risk of developing shoulder and neck pain.
The improper carrying of heavy loads, especially if done repeatedly or on one side of the body, creates muscle tension and can lead to trigger points, resulting in localized or referred pain. This imbalance not only causes immediate discomfort but can also lead to uneven muscle development, further stressing the neck and shoulder musculature. Moreover, emotional and physical stress and anxiety are well-documented contributors to increased muscle tension, which can exacerbate or directly cause chronic neck and shoulder pain. Conditions like frozen shoulder, also known as adhesive capsulitis, develop gradually, starting with pain and progressing to severely restricted movement, often linked to such chronic inflammatory processes.

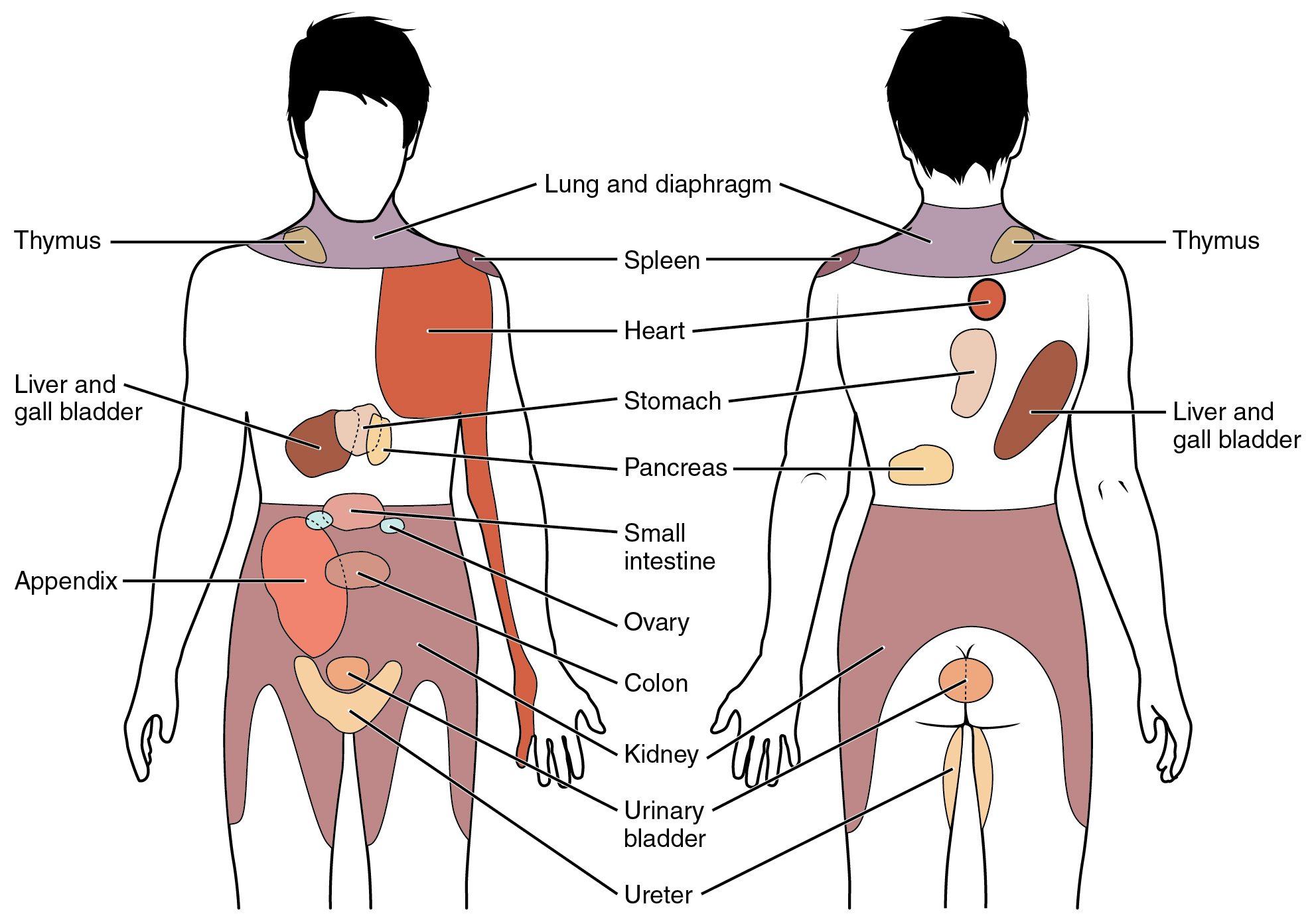
9. **Systemic Illnesses Presenting as Shoulder Blade Pain** Pain localized to the shoulder blades can often be a deceptive symptom, signaling underlying systemic illnesses that require urgent medical attention. While frequently attributed to musculoskeletal strain, this discomfort can arise from critical conditions affecting the heart, lungs, or abdominal organs. Understanding these potentially serious associations is vital for appropriate diagnostic assessment.
Cardiac problems, although typically associated with chest pain, can manifest as pain between the shoulder blades. Conditions such as heart attacks, aortic dissection—a tear in a major heart vessel causing immediate, severe pain—or pericarditis, which is inflammation of the heart’s lining, may present with referred pain in this area. Especially in women, heart attack pain can be felt more profoundly in the back of the shoulder and between the shoulder blades, necessitating immediate medical evaluation if accompanied by other symptoms like shortness of breath or sweating.
Lung conditions also frequently refer pain to the shoulder blade region. Lung cancer, particularly a Pancoast tumor that develops above the lungs, often causes pain in the shoulders, arms, and shoulder blades. Other concerning pulmonary issues, such as a pulmonary embolism (a blood clot in the lungs) or a collapsed lung (pneumothorax), can present with shoulder blade pain, often accompanied by shortness of breath, reinforcing the need for prompt medical assessment.
Furthermore, abdominal and pelvic issues can surprisingly cause referred shoulder blade pain, particularly if nerves around the diaphragm become inflamed. Gallstones, peptic ulcer disease, acid reflux, and liver illness can trigger right shoulder blade pain, while pancreatitis, an inflammation of the pancreas, is more frequently associated with left-sided shoulder blade discomfort. Even shingles, a viral infection of the chest wall, can cause stinging or burning pain in the shoulder blade region before the characteristic rash appears. In rare instances, tumors in the chest, such as lymphomas or cancers of the stomach, esophagus, or liver, can metastasize to the bones of the shoulder blades, making persistent or unexplained pain in this area a concerning symptom that warrants thorough investigation for underlying malignancy.
10. **Specific Nerve Compression Syndromes Beyond the Thoracic Outlet** While Thoracic Outlet Syndrome addresses a specific area of nerve compression, other distinct neurological conditions can cause significant shoulder and arm pain due to nerve involvement. These syndromes often present with characteristic patterns of burning, shooting pain, altered sensation, and weakness, demanding careful differentiation from musculoskeletal issues.
Brachial neuritis, a rare inflammatory condition affecting the brachial plexus—a network of nerves controlling the shoulder and arm—is one such syndrome. It typically develops very quickly, often at night, causing intense pain in the shoulder and arm. This condition can affect individuals of any age but is most common in young to middle-aged adults, highlighting its unpredictable onset and the severe discomfort it can inflict.
Another specific neural phenomenon is T4 syndrome, also known as Upper Thoracic Syndrome. This condition presents a complex combination of symptoms, including thoracic pain that may radiate across the shoulder blades and down one or both arms. Patients often experience headaches, stiffness, and muscle spasms, with the primary focus of pain typically located around the T4 vertebra. The diffuse nature of its symptoms underscores the challenge in diagnosing such nerve-related conditions and distinguishing them from more common musculoskeletal complaints.
General nerve pain, whether from direct nerve damage or impingement by surrounding structures like spinal vertebrae and discs, can cause discomfort anywhere along the nerve pathway from the neck to the hand. This type of pain is consistently associated with altered sensation, such as tingling and numbness, and often accompanied by a noticeable weakness in the affected limb. Recognizing these distinct neural presentations is crucial for accurate diagnosis and the implementation of targeted therapies, which differ significantly from treatments for muscular or joint-related pain.
11. **Understanding Pain Patterns in the Posterior Shoulder and Scapula** Pain experienced around the back of the shoulders and between the shoulder blades can stem from a variety of sources, ranging from acute muscle strains to chronic structural issues. The posterior shoulder pain diagram highlights that conditions in this area can sometimes overlap with those referring pain down the side and back of the arms, necessitating careful assessment of specific pain patterns and associated symptoms.
Muscle strains are a very common cause of pain across the top part of the back of the shoulders, particularly affecting the upper trapezius muscles. Overworking these muscles through heavy lifting, racket sports, or prolonged tension from poor computer posture can trigger significant discomfort. Similarly, overloading the trapezius muscles is a frequent cause of pain between the shoulder blades, often linked to heavy lifting, repetitive overhead work, carrying heavy bags, stress, or underlying muscle weakness.
Structural issues such as rotator cuff tears can also cause pain down the outer side of the shoulder and part way down the arm. These can be acute injuries from a fall or heavy lifting, or degenerative tears resulting from repetitive wear and tear. Shoulder impingement syndrome, another common condition, can also cause diffuse pain down the outer part of the arm when structures get repeatedly squashed between the shoulder bones, often due to repetitive movements or wear. Additionally, conditions like scapulothoracic bursitis, known as Snapping Scapula Syndrome, cause a constant, dull ache in the shoulder blade with a grinding or snapping sensation during arm movements, reflecting an issue with the shoulder blade’s motion over the rib cage. Even a fractured shoulder blade, though requiring considerable force, presents with severe posterior pain. Pinpoint areas of deep, dull aching pain around the shoulder can also indicate trigger points, which are small, tight bands of fascia that are extremely sensitive to touch, particularly common in the trapezius muscle fibers.

12. **Distinguishing Specific Symptoms: Night Pain, Clicking, and Burning Sensations** Beyond general location, the specific characteristics of shoulder pain offer invaluable diagnostic clues. Symptoms such as pain that worsens at night, burning sensations, or audible clicking and grinding sounds can point towards distinct underlying conditions, guiding medical professionals toward a more precise diagnosis. Understanding these nuanced presentations is paramount when the pain feels diffuse or encompasses the entire arm.
Shoulder pain experienced predominantly at night, or when lying on the affected side, is a common indicator of several conditions, including rotator cuff tears and frozen shoulder. This nocturnal exacerbation often suggests inflammation or impingement that becomes more pronounced with certain sleeping positions or during periods of rest when muscle guarding is reduced. Such persistent nighttime discomfort often significantly disrupts sleep patterns and impacts overall quality of life, necessitating prompt medical attention.
Burning shoulder pain can be particularly indicative of nerve involvement, as seen in conditions like brachial neuritis or more general nerve damage originating from the neck. While muscle strains can also produce a burning sensation, especially with acute injury, a consistent, radiating burn often points to neural irritation. Similarly, sharp shoulder pain can be a symptom of a wide range of issues, from a SLAP tear to inflammation in the rib cartilage, and distinguishing its origin often requires a comprehensive assessment of accompanying symptoms and physical movements.
Audible symptoms such as clicking, popping, or grinding within the shoulder joint are significant diagnostic markers. A SLAP tear, for instance, often results in clicking or catching sensations, while scapulothoracic bursitis can produce a grinding or snapping sound with arm movements. These mechanical sounds suggest structural irregularities or friction within the joint, providing concrete evidence of internal damage or dysfunction. Additionally, limited range of motion and pain when lifting the arm are common indicators of conditions like shoulder bursitis, rotator cuff tears, or impingement syndrome, further refining the diagnostic picture.
The human body’s capacity to signal distress through varied forms of pain, from the subtle ache to the acute, radiating sensation, is a complex testament to its intricate design. As we have explored, chest, shoulder, and neck pain are not always singular in origin; they are often interconnected symptoms of a broader physiological narrative. From distinguishing the urgent alarm of a cardiac event to recognizing the insidious onset of chronic conditions, understanding these signals empowers both patients and practitioners to navigate the path toward accurate diagnosis and effective care. This journey through the nuances of physical discomfort reinforces the profound importance of informed observation, timely intervention, and a holistic approach to health and well-being. Always remember, when confronting persistent or severe pain, consulting a healthcare provider remains the most prudent course of action to ensure appropriate diagnosis and tailored treatment. The body speaks in many tongues, and learning to listen is the first step towards healing.