Every second that passes by, your heart works hard to keep you alive. By pumping your blood through your circulatory system, each heartbeat ensures that your tissues, organs, systems and cells all get the oxygen and nutrients they need to carry out their daily biological processes. This continuous, vital work underscores why understanding key health metrics, particularly your blood pressure, is not just beneficial but essential for proactive health management.
Far from being just another set of numbers, your blood pressure reading provides critical insights into the efficiency and strain on your cardiovascular system. These measurements offer a window into how effectively your heart is performing its tireless task and the force exerted on your arteries. For many, the array of measurements and medical terminology can feel daunting, creating a barrier to truly grasping what these numbers signify for individual well-being.
This comprehensive guide aims to demystify blood pressure readings, transforming complex medical concepts into clear, actionable understanding. We will explore what the numbers mean, delineate the different blood pressure categories, and provide practical advice on maintaining heart health. By empowering you with this knowledge, our goal is to help you make informed decisions, apply concrete recommendations, and take proactive steps towards preventing complications and maintaining overall cardiovascular wellness.
1. **The Fundamental Role of Blood Pressure**Your heart is a remarkable organ, relentlessly working to sustain life. Every beat is a testament to its commitment, propelling blood through an intricate network of arteries, veins, and capillaries that make up your circulatory system. This continuous circulation is absolutely critical, as it ensures that every cell, tissue, and organ in your body receives the vital oxygen and nutrients necessary for their daily biological processes.
The force with which this blood moves through your arteries is what we measure as blood pressure. It is a fundamental indicator of cardiovascular health, reflecting the efficiency and effort behind your heart’s pumping action. When we talk about blood pressure, we are essentially discussing how hard your heart is working to deliver life-sustaining blood to every corner of your body.
Therefore, gathering information about your blood pressure numbers provides us with important details about the workload on your heart. Understanding these measurements allows healthcare professionals to assess potential risks and helps individuals take informed steps to safeguard their long-term health. It serves as an early warning system, highlighting areas where intervention might be needed to maintain the smooth functioning of your entire physiological system.
Read more about: 10 Critical Car Maintenance Tasks You Can’t Afford to Ignore
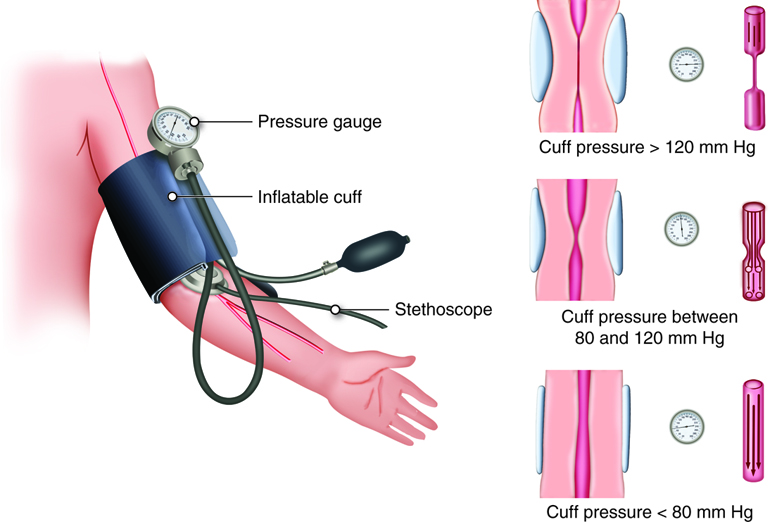
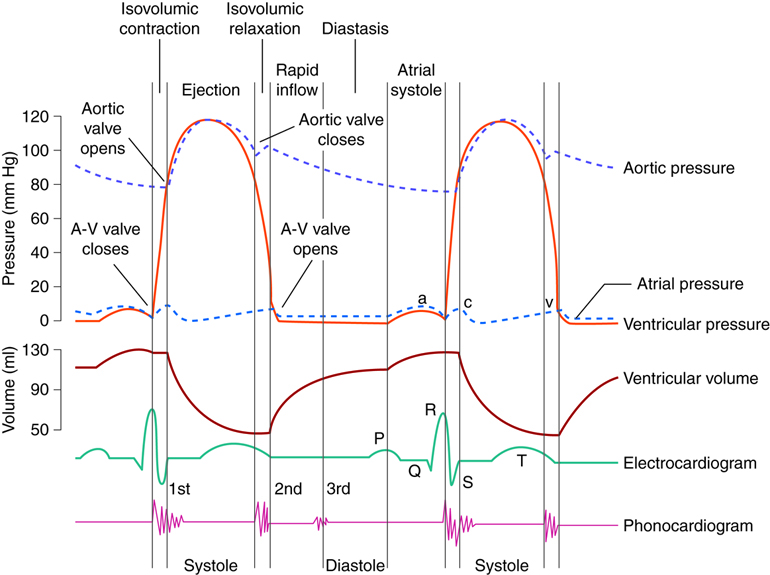
2. **Decoding the Numbers: Systolic and Diastolic Pressure**When you receive a blood pressure reading, you’ll notice it’s always expressed as two numbers, typically one above the other, measured in millimeters of mercury (mm Hg). These two distinct numbers provide different, yet equally crucial, pieces of information about your heart’s performance throughout its cycle of beating and resting. It’s essential to understand what each number represents to fully grasp your reading.
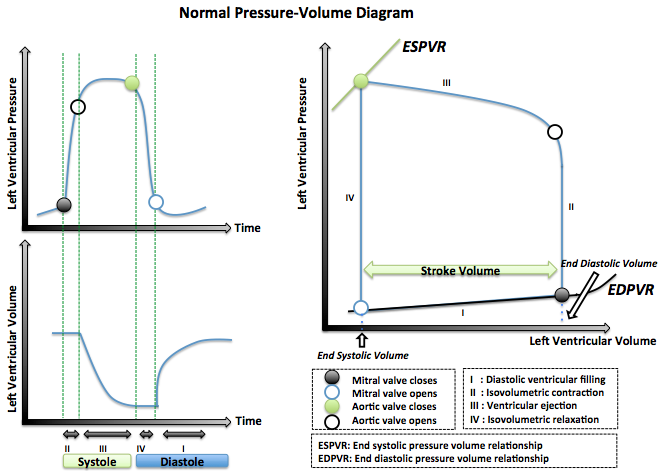
The top number is called the systolic pressure. This measurement captures the force exerted on your arteries precisely when your heart beats, or “squeezes,” actively pushing blood out into your arterial system. Dr. Luke Laffin, a cardiologist, explains that systolic blood pressure measures “the force that’s exerted on your arteries when your heart squeezes and sends blood into your arteries.” It reflects the peak pressure during the heart’s contraction.
Conversely, the bottom number is known as the diastolic pressure. This figure measures the pressure within your arteries during the period between heartbeats, when your heart is at rest and relaxing, filling back up with blood. Dr. Laffin clarifies that diastolic blood pressure measures “the force that’s exerted on your arteries during diastole, when your heart is at rest and relaxing between beats.” Together, these two numbers paint a comprehensive picture of both the pumping and resting phases of your cardiac cycle.
3. **Understanding Blood Pressure Categories**To standardize the interpretation of blood pressure readings and guide appropriate health interventions, medical bodies like the American College of Cardiology and the American Heart Association have established clear categories. These categories help healthcare professionals and individuals understand what a particular reading means for their health status and what actions might be advisable.
These guidelines, updated in 2017 in the United States, aim to create lower thresholds across five categories in an effort to reduce the risk of heart disease and stroke. By targeting and maintaining lower blood pressure levels, the hope is to reduce the damage that’s caused to blood vessels when blood pressure is elevated over time. The five general categories include normal, elevated, stage 1, stage 2, and a critical “hypertensive crisis.”
It’s important to note how readings are categorized when the systolic and diastolic numbers fall into different ranges. The rule is straightforward: “If your top and bottom numbers fall into two different categories, your correct blood pressure category is the higher category.” For example, if your reading is 125/85 mm Hg, which involves an elevated systolic and a stage 1 diastolic, you are classified as having stage 1 hypertension.
Read more about: A Financial Advisor’s Blueprint: 15 Essential Investment Strategies for a Secure Retirement in 2025

4. **Normal Blood Pressure: The Ideal Range**Achieving and maintaining normal blood pressure is a cornerstone of good cardiovascular health, signifying that your heart and blood vessels are operating efficiently without undue strain. According to the guidelines, blood pressure numbers “less than 120/80 mm Hg are considered within the ideal range.” This is the benchmark for optimal heart function, indicating minimal risk from blood pressure alone.
Dr. Laffin concurs, stating, “An ideal blood pressure would be less than 120 millimeters of mercury (mm Hg) for the systolic blood pressure and less than 80 mm Hg for the diastolic blood pressure.” For individuals whose readings consistently fall within this healthy zone, the primary recommendation is to maintain these excellent numbers through a commitment to a healthy lifestyle.
This commitment involves several key components. Paramount among them are adopting a heart-healthy diet, engaging in regular physical exercise, and ensuring you get sufficient, restorative sleep. These lifestyle choices collectively support overall well-being and play a crucial role in preventing or delaying the onset of high blood pressure or other related health complications, thereby safeguarding your cardiovascular future.
Read more about: Understanding Blood Pressure: A Comprehensive Guide for Seniors and Caregivers
5. **Elevated Blood Pressure: A Call for Vigilance**The category of “elevated blood pressure” serves as an important early warning signal, indicating that your readings are consistently higher than normal but not yet reaching the threshold for hypertension. Specifically, this category applies “when your readings are consistently between 120 and 129 mm Hg systolic and less than 80 mm Hg diastolic.” While not yet full-blown high blood pressure, this stage necessitates attention.
People identified with elevated blood pressure face an increased risk of progressing to full-fledged high blood pressure, or hypertension, in the future. This progression, however, is not inevitable. It presents a critical opportunity to intervene proactively through lifestyle adjustments, which can often prevent the condition from worsening.
The recommendation for elevated blood pressure is clear: “Maintain or adopt a healthy lifestyle.” This involves reinforcing or implementing habits such as a balanced, heart-healthy diet, regular physical activity, and adequate sleep. By taking these steps, individuals can effectively manage their condition and significantly reduce their risk of developing more serious cardiovascular issues down the line, highlighting the power of early intervention.
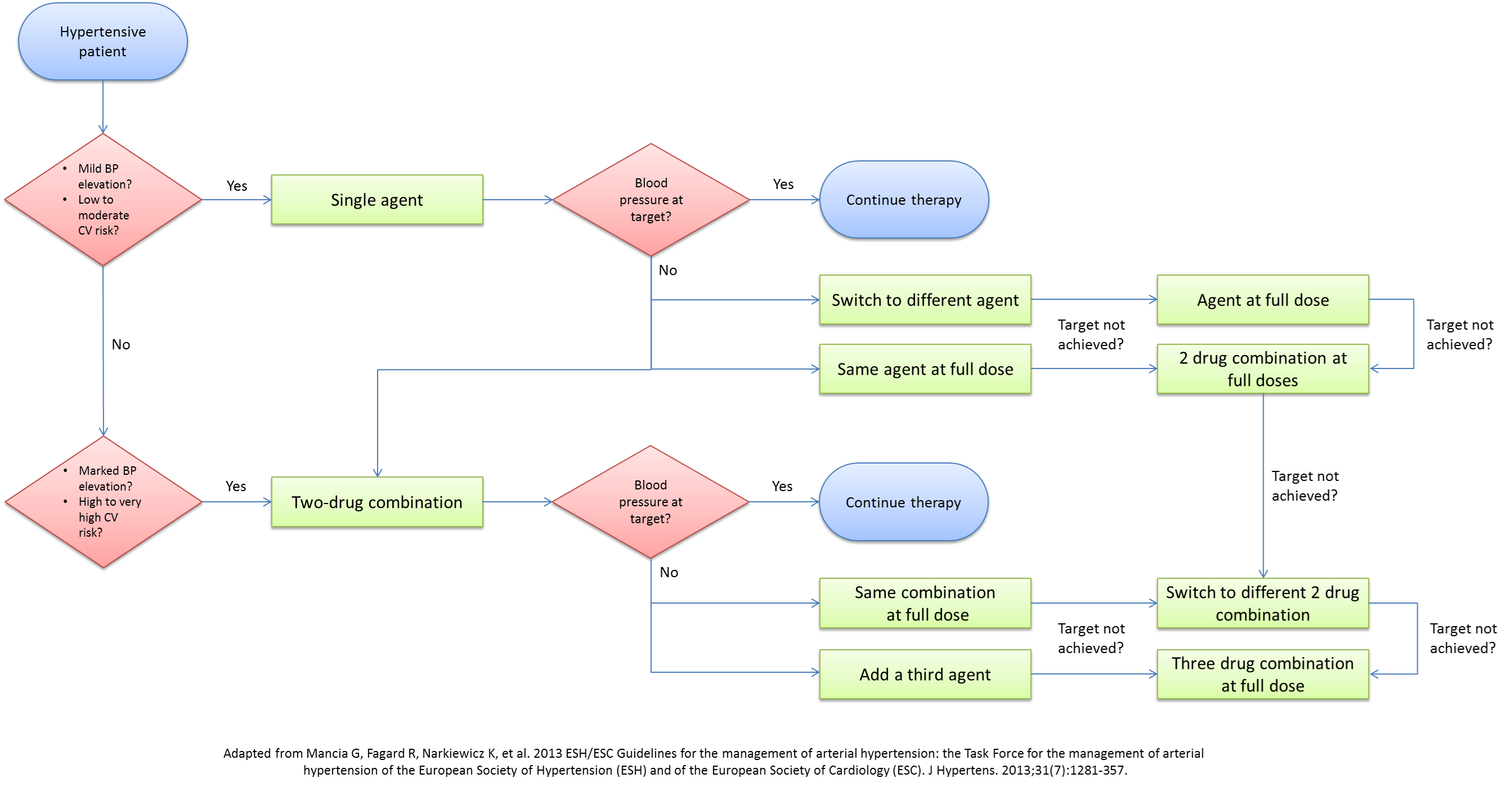
6. **Stage 1 Hypertension: When Lifestyle Meets Medical Advice**When blood pressure readings consistently rise beyond the elevated category, they enter the realm of “Stage 1 hypertension.” This occurs “when your blood pressure readings consistently fall within the range of 130 to 139 mm Hg systolic and/or 80 to 89 mm Hg diastolic.” This stage marks a more serious level of high blood pressure that typically requires a dual approach to management.
For individuals diagnosed with Stage 1 hypertension, especially if they have a personal history of cardiovascular disease, heart attack, or stroke, the recommendations become more assertive. While a healthy lifestyle remains fundamental, it is often complemented by medical intervention. The guidance is to “Maintain or adopt a healthy lifestyle. Talk to a healthcare professional about taking one or more medicines.”
This combination of lifestyle modifications and potential medication is crucial for effectively controlling blood pressure at this stage. The aim is to lower the readings back into a normal or near-normal range, thereby reducing the strain on the cardiovascular system and mitigating the long-term risks associated with sustained high blood pressure, such as damage to vital organs.

7. **Diagnosing High or Low Blood Pressure: Beyond a Single Reading**A diagnosis of high blood pressure, or hypertension, is a significant medical determination that is rarely made based on a single measurement. It is well understood that numerous factors can temporarily influence blood pressure throughout the day, including stress levels, recent food intake, and even ambient temperature. Therefore, healthcare providers employ a methodical approach to ensure accuracy.
“A diagnosis of high blood pressure is usually based on the average of two or more readings taken on separate visits.” This strategy helps to account for temporary fluctuations and ascertain if a consistently elevated pressure is indeed present. Moreover, for the initial assessment, “The first time your blood pressure is checked, it should be measured in both arms to see if there is a difference.” Subsequently, “the arm with the higher reading should be used” for future measurements to ensure consistency and capture the most accurate possible reading.
It is important to remember that for diagnosis, “only one of your numbers needs to be higher than it should be to be diagnosed with high blood pressure, and only one needs to be lower than it should be to be diagnosed with low blood pressure.” This means if your systolic pressure is over 140 mm Hg, or your diastolic pressure is over 90 mm Hg, you may be diagnosed with high blood pressure, irrespective of the other number. Similarly, if your top number is under 90 mm Hg or your bottom number is under 60 mm Hg, you may be diagnosed with low blood pressure. The context also clarifies conditions like Isolated Systolic Hypertension (systolic > 140mmHg, diastolic healthy) and Isolated Diastolic Hypertension (diastolic > 90mmHg, systolic healthy), emphasizing that a single elevated or lowered number can be diagnostically significant. An accurate reading is paramount, as it “helps your healthcare team decide what kind of treatment you may need, if any.”

8. **Stage 2 Hypertension: Navigating a More Serious Diagnosis**When blood pressure readings consistently exceed Stage 1 thresholds, they enter the “Stage 2 hypertension” category, indicating a more significant cardiovascular strain. This is diagnosed “when your blood pressure readings are consistently 140 mm Hg or higher for systolic and 90 mm Hg or higher for diastolic.” This classification signifies persistently high pressure on your arteries, demanding immediate attention and often a more intensive management approach.
Cardiologist Dr. Luke Laffin explains the physiological impact of this sustained elevation: “Your heart has to pump against this pressure, and this pressure is then transmitted to all your organs like your brain and your kidneys.” This constant resistance forces the heart, a muscle, to work much harder. Over time, “The heart has to squeeze against that pressure to actually eject the blood. It’s a muscle. So, if you have to squeeze against all that pressure, your heart is going to thicken and it’s going to damage itself.”
The implications of such long-term stress extend beyond the heart, potentially affecting vital organs throughout the body. The primary goal of intervention at this stage is to protect these organs from progressive damage. Consequently, managing Stage 2 hypertension typically involves a comprehensive strategy that combines lifestyle adjustments with medical treatment.
For those diagnosed, leading health organizations recommend maintaining a healthy lifestyle and consulting a healthcare professional about taking “more than one medicine.” This dual approach aims to significantly lower blood pressure, mitigating the risk of serious complications such as heart attacks and strokes.

9. **Hypertensive Crisis: Recognizing a Medical Emergency**While sustained high blood pressure requires ongoing management, blood pressure can acutely spike to dangerously high levels, constituting a “hypertensive crisis.” This critical medical situation is defined by readings “over 180/120 mm Hg.” Such extreme numbers demand immediate attention and, depending on accompanying symptoms, may necessitate emergency medical care.
If you obtain a reading above 180/120 mm Hg and feel relatively well, without new symptoms, it’s advisable to “wait a couple of minutes and retake your measurements again.” If readings remain consistently high, contact a healthcare provider for prompt evaluation. However, the presence of new or concerning symptoms changes the protocol dramatically.
If you are “experiencing any new symptoms you haven’t felt before or something doesn’t feel right to you, going to the emergency room is more important than stopping to measure your blood pressure.” Dr. Laffin advises immediate emergency medical evaluation for symptoms like chest pain, shortness of breath, severe headache, weakness, extreme fatigue, garbled speech, or facial droop, especially with a history of heart disease or high blood pressure.
He stresses, “There’s no specific blood pressure threshold over which someone needs to go to the emergency department, but if you’re having new concerning symptoms you haven’t experienced before, these are issues where you definitely need to be seen in the emergency department right away even if you have normal blood pressure and especially if you have high blood pressure.”
10. **Low Blood Pressure (Hypotension): When Numbers Dip Too Low**While attention often focuses on high blood pressure, equally important is understanding when blood pressure falls too low, a condition called hypotension. This occurs “if you’re getting systolic readings of less than 90 mm Hg” or if your diastolic pressure is under 60 mm Hg. Similar to high blood pressure, diagnosis can be made if “only one of your numbers needs to be lower than it should be.” This condition can present various symptoms and, in certain circumstances, be serious.
Symptoms associated with hypotension often include dizziness, fainting, and fatigue, indicating insufficient blood flow to vital organs. Cardiologist Dr. Luke Laffin explains potential causes: “Sometimes, if we have infections or we’re dehydrated, our blood pressure can be low.” He adds, “If we have significant bleeding, our blood pressure can be low and that can be dangerous, particularly more acutely.” These examples highlight that while some instances may be benign, others signal an underlying issue requiring urgent attention.
Beyond acute scenarios, persistent or symptomatic low blood pressure risks long-term health issues, including “acute kidney injury or stroke” without proper treatment. This underscores the need for individuals experiencing consistent hypotension symptoms to seek medical evaluation. Understanding the cause is the first step toward effective management, which may involve addressing underlying conditions, adjusting medications, or adopting specific lifestyle modifications.

11. **High Blood Pressure: The “Silent Killer” Unveiled**One of the most insidious aspects of hypertension is its often symptomless nature, earning it the ominous moniker “the silent killer.” This term reflects the reality that “Most people don’t feel any different even when their blood pressure is elevated,” as Dr. Laffin explains. Without obvious warning signs, individuals can live for years with dangerously high blood pressure, unaware of the damage silently occurring within their bodies.
The human body is remarkably adaptable, often compensating for elevated blood pressure for short to medium periods. Dr. Laffin notes, “For most people, our body is able to adapt to high blood pressures for short-to-medium periods of time.” This adaptive capacity, while seemingly beneficial, creates a false sense of security, allowing the condition to progress unchecked without immediate discomfort.
However, this adaptation comes at a significant long-term cost. “The problem is the long-term elevations in blood pressure and the impact it has over the long term — left ventricular hypertrophy (the thickening of the heart muscle), kidney disease, heart failure — these all manifest over years to decades as you continue to have untreated high blood pressure.” The relentless force on arterial walls leads to structural changes and functional impairments, culminating in serious conditions preventable with earlier detection.
The “silent killer” designation powerfully reminds us of the importance of regular blood pressure screenings, even in the absence of symptoms. Early detection through routine checks is the most effective defense against the silent progression of hypertension and its devastating consequences, empowering proactive intervention before irreversible damage occurs.

12. **Monitoring Blood Pressure at Home: Empowering Self-Care**Home blood pressure monitoring is a powerful tool for managing health, supplementing clinic readings and tracking treatment. For accurate results, a standardized protocol is essential: use a validated cuff recommended by your healthcare provider. Validated systems are available through resources like the American Medical Association’s database.
Before any measurement, ensure you “be at rest, seated, with your feet flat on the floor, your back straight and supported, and your arm resting at heart height for three to five minutes.” Dr. Laffin also advises avoiding coffee or smoking recently, and having an empty bladder, as “these are all things that can raise your blood pressure.” These steps minimize variables that could artificially inflate readings.
To ensure a representative assessment, it’s recommended to take “not one, but two or three measurements separated by 30 to 60 seconds between each measurement.” Dr. Laffin explains: “It’s common to see a small decrease from the first to the second measurement and then from the second to the third.” This multi-measurement approach provides a more accurate average than a single reading, which might be influenced by initial stress.
Consistent home monitoring offers profound benefits. “Keeping track of these numbers over time can also help your cardiologist and other healthcare providers determine any potential diagnoses should any symptoms or concerns arise.” For those with hypertension, Dr. Laffin advises checking blood pressure “at least once every two to four weeks at home,” and more frequently following “medication changes, other lifestyle changes or a personal history of heart disease or stroke,” providing a continuous feedback loop for effective health management.

13. **Identifying Emergency Symptoms: When to Seek Immediate Medical Help**While regular monitoring and proactive management are crucial, it is equally vital to recognize when symptoms signal a medical emergency requiring immediate attention. Certain signs, especially when accompanied by high blood pressure or a history of cardiovascular issues, should prompt an immediate trip to the emergency room. The focus shifts from numbers to critical physiological distress.
Dr. Luke Laffin strongly advises seeking emergency medical evaluation for new concerning symptoms such as chest pain, shortness of breath, severe headache, weakness, extreme fatigue, garbled speech, or facial droop. These are indicators of potential organ damage or acute cardiovascular events requiring urgent professional assessment and intervention to prevent severe harm.
Crucially, the decision to go to the emergency room should not hinge on obtaining a perfect blood pressure measurement. As Dr. Laffin stresses, “There’s no specific blood pressure threshold over which someone needs to go to the emergency department, but if you’re having new concerning symptoms you haven’t experienced before… you definitely need to be seen in the emergency department right away.” In such instances, “going to the emergency room is more important than stopping to measure your blood pressure,” as swift action can make a critical difference in outcomes.
Read more about: Navigating the Complexities of Body Pain: A Definitive Guide to Chest, Shoulder, and Neck Discomfort

14. **Holistic Management: Integrating Lifestyle and Medical Approaches**Successfully managing blood pressure—whether preventing its rise, controlling elevated readings, or treating established hypertension—involves a comprehensive strategy integrating lifestyle modifications and, when necessary, medical interventions. This holistic approach empowers individuals to take charge of their cardiovascular health, aiming for sustained well-being.
At the core of prevention and early management is a commitment to a heart-healthy lifestyle. This foundation, emphasized across all blood pressure categories, encompasses a “heart-healthy diet,” “regular physical exercise,” and “sufficient, restorative sleep.” These pillars optimize cardiovascular function, reducing strain and often preventing or delaying the onset of high blood pressure.
When blood pressure readings escalate to Stage 1 or Stage 2 hypertension, medical intervention becomes a crucial complement. While healthy habits remain fundamental, healthcare professionals may recommend or prescribe “one or more medicines” for Stage 1, and potentially “more than one medicine” for Stage 2. This dual strategy effectively controls blood pressure, significantly reducing the risk of complications.
Management plans are also highly individualized. The Mayo Clinic notes, “These recommendations address high blood pressure as a single health condition. If you also have heart disease, diabetes, chronic kidney disease or certain other conditions, you may need to treat your blood pressure more aggressively.” Working closely with your healthcare team ensures a personalized plan considering your unique health profile, ensuring the most effective and safest path to optimal blood pressure control.
Decoding your blood pressure numbers is a powerful step towards proactive health management, transforming abstract measurements into actionable insight. From understanding the nuances of systolic and diastolic readings to recognizing various categories—from ideal normal to critical hypertensive crisis—this knowledge empowers you. By embracing regular monitoring, identifying emergency symptoms, and committing to holistic management strategies that blend healthy lifestyles with appropriate medical guidance, you can actively safeguard your cardiovascular future. Remember, staying informed and working closely with your healthcare team is your best defense against the “silent killer” and key to a healthier, more vibrant life.