
Imagine being able to fix a disease by repairing a faulty gene inside the body. This once futuristic idea is rapidly becoming a life-changing reality for many patients, and 2025 stands as a monumental year in this incredible journey. Gene therapy, a true frontier of modern medicine, is actively modifying or replacing defective genes within a person’s cells to treat or prevent a vast spectrum of diseases.
This cutting-edge approach holds immense promise for serious conditions that have long plagued humanity, including various cancers, inherited genetic disorders, debilitating blood diseases, and even some chronic illnesses. Unlike conventional treatments that merely manage symptoms, gene therapy targets the very root cause of these health problems. It’s a fundamental shift in how we conceive of healing, offering a path to long-term correction rather than temporary relief.
Indeed, 2025 is proving to be a watershed moment for gene therapy research, marked by a cascade of remarkable breakthroughs that are fundamentally reshaping the landscape of medical treatment. These advancements are offering unprecedented hope for patients who, until now, faced limited or even no viable options. We are witnessing an era where the intricate machinery of life itself is being re-engineered for better health, moving beyond the realm of science fiction and firmly into clinical practice.

1. **CRISPR-based Gene Therapy for Sickle Cell Disease & Beta-Thalassemia (Casgevy)**One of the most profound successes defining the current era of gene therapy is the landmark clearance of Casgevy (Exagamglogene Autotemcel). This revolutionary treatment stands as the very first CRISPR-based therapy, initially authorized for sickle cell disease in late 2023. Its subsequent FDA approval in January for transfusion-dependent beta-thalassemia (TDT) further solidified its position as a game-changer for two devastating blood disorders.
Casgevy operates by leveraging the precision of CRISPR gene editing to directly address the faulty gene responsible for these conditions. This targeted approach represents a monumental leap forward, moving beyond symptom management to offering a potential cure. For patients grappling with the chronic pain and complications of sickle cell disease or the lifelong need for transfusions in beta-thalassemia, this therapy offers a new dawn of hope.
The impact on patients treated with Casgevy has been nothing short of transformative. Early trials have demonstrated that patients are living without the excruciating pain crises characteristic of sickle cell disease, and many no longer require regular blood transfusions. These are life-altering outcomes, alleviating immense physical and emotional burdens. The success of Casgevy also underscores the incredible potential of gene editing technologies to permanently correct genetic errors, setting a precedent for future therapies.
Behind this scientific marvel are pioneers like Vertex Pharmaceuticals and CRISPR Therapeutics. Their collaborative efforts brought this innovative treatment from the laboratory to the clinic, showcasing the power of advanced research and development in translating complex genetic science into practical, life-saving applications. The journey of Casgevy illustrates the rigorous process involved in proving the safety and efficacy of such cutting-edge treatments, paving the way for further advancements in the field of gene editing.
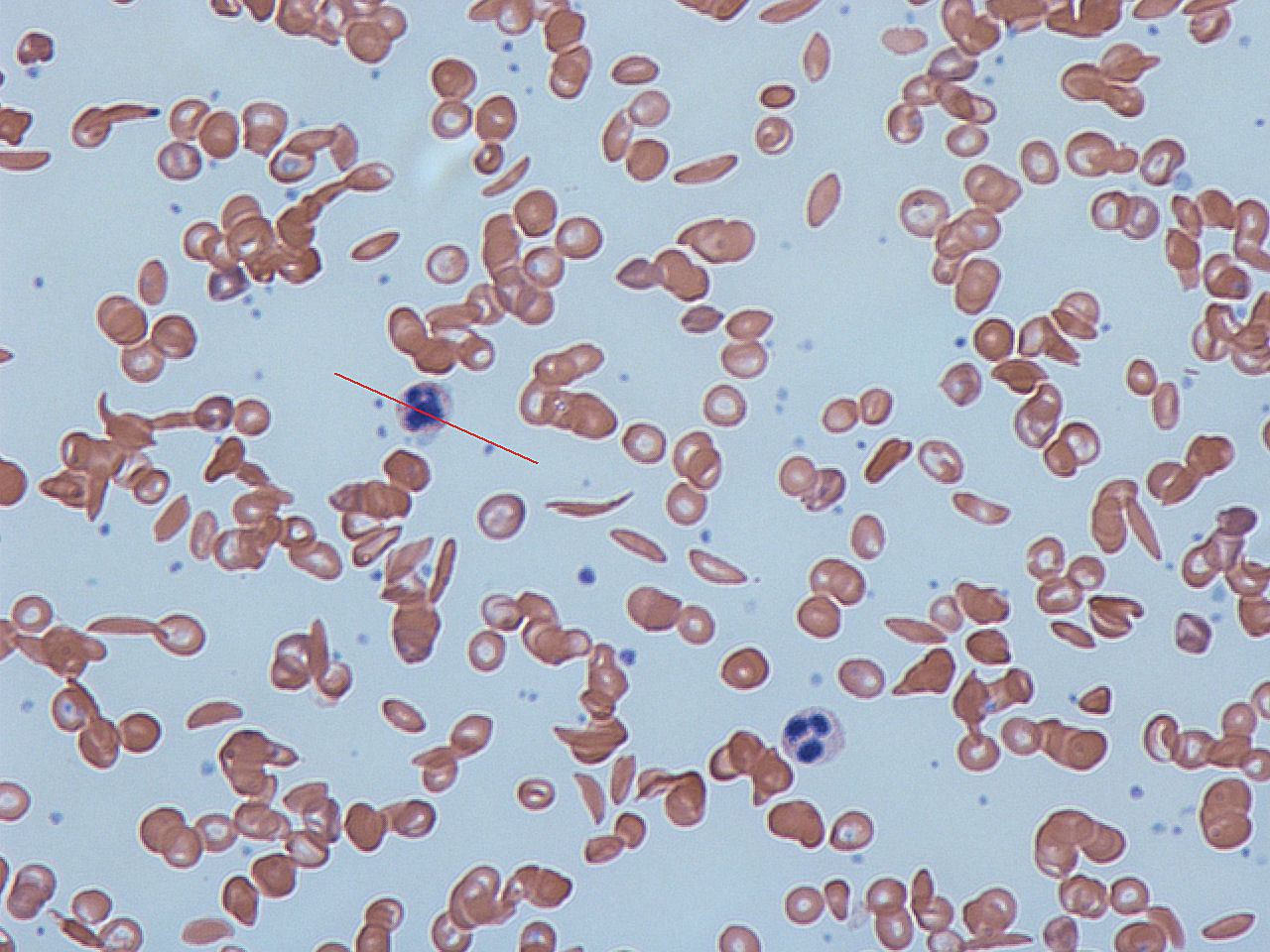
2. **Base Editing for Sickle Cell Disease**While Casgevy represents a significant milestone, the landscape of gene editing continues to evolve with even more refined techniques. A new technique, distinct yet complementary to the broader CRISPR approach, is base editing. This advanced method has emerged as another remarkable success in 2025, specifically for its application in treating sickle cell disease, offering a nuanced way to correct genetic errors without cutting the DNA double helix entirely.
Base editing precisely modifies individual DNA bases, correcting the faulty gene responsible for sickle cell disease with even greater accuracy and potentially fewer off-target effects. This innovative approach enhances the safety profile and refines the efficacy of genetic correction. Early trials utilizing base editing have corroborated the profound benefits observed in other gene therapies for this condition, further solidifying the potential for a curative intervention.
Patients undergoing base editing treatments for sickle cell disease are experiencing similar dramatic improvements, living without the debilitating pain crises and significantly reducing or eliminating their need for regular blood transfusions. The ability to fine-tune genetic repairs at such a molecular level opens new avenues for therapeutic development. It represents a continuous push towards increasingly precise and less invasive genetic interventions.
Companies like Beam Therapeutics are at the forefront of pioneering base editing technologies. Their foundational work in developing and applying this next-generation gene editing approach has positioned them as key players in the future of genetic medicine. The ongoing success of base editing platforms highlights the rapid pace of innovation within the gene therapy sector, promising a future where genetic diseases can be addressed with unparalleled accuracy.
Read more about: Decoding mRNA: A Comprehensive Overview of its Molecular Biology and Role in Modern Vaccine Development

3. **Advances in Cancer Gene Therapy**Gene therapy is profoundly transforming the way certain cancers are approached and treated, particularly through the innovation of CAR-T cell therapy. This sophisticated method involves altering a patient’s own immune cells, specifically T-cells, to equip them with the ability to recognize and destroy cancer cells with remarkable precision. In 2025, this personalized cancer gene therapy has yielded excellent results against some of the most challenging malignancies.
Notably, this approach has shown significant promise in treating difficult cancers such as glioblastoma, an aggressive type of brain cancer that traditionally has a very poor prognosis, and various advanced blood cancers. By genetically editing a patient’s T-cells to express chimeric antigen receptors (CARs), these cells become super-soldiers, engineered to specifically target and eliminate tumor cells while minimizing damage to healthy tissues. This represents a significant paradigm shift from conventional chemotherapy.
The impact on patient outcomes has been substantial. Survival rates have markedly improved for individuals battling these aggressive cancers, offering a lifeline where previously there was little hope. Furthermore, patients are experiencing fewer severe side effects compared to traditional chemotherapy regimens, greatly enhancing their quality of life during and after treatment. This improvement in both efficacy and tolerability makes CAR-T cell therapy a cornerstone of modern oncology.
Leading pharmaceutical giants and innovative biotech firms are driving this revolution. Gilead/Kite, with its leading CAR-T franchise including Yescarta and Tecartus, and Bristol Myers Squibb (BMS), known for Abecma and Breyanzi, have reported strong quarterly revenues, underscoring the commercial success and clinical adoption of these therapies. Novartis’s Kymriah also stands as a pioneer in the CAR-T space. Moreover, Adaptimmune’s Tecelra gaining approval for synovial sarcoma in August exemplifies the diversification of CAR-T applications, extending beyond blood cancers to solid tumors.
Read more about: Beyond the Leg Warmers: 14 Defining Moments of the 80s That Still Resonate Today

4. **Gene Therapy for Leber Congenital Amaurosis (Luxturna)**Another significant breakthrough in 2025 arrives in the realm of inherited eye disorders, bringing light to those afflicted by genetic blindness. A new gene therapy, Luxturna (voretigene neparvovec), has been approved this year for Leber congenital amaurosis (LCA), a rare inherited eye disease. This therapy has provided a beacon of hope by helping patients regain partial vision, a truly life-changing outcome for individuals born with or developing severe visual impairment due to this condition.
The mechanism behind Luxturna is elegantly precise: it involves injecting a healthy gene directly into the retina. This healthy gene is delivered by AAV2 vectors, which carry a modified form of the human RPE65 gene. Once inside the retinal cells, the new gene enables them to start functioning normally, correcting the genetic defect that caused the vision loss. This targeted approach ensures that the therapeutic gene reaches the specific cells responsible for vision, maximizing efficacy.
Luxturna is specifically designed for individuals with biallelic disease-causing variants in RPE65, addressing the root genetic cause of a specific form of LCA. Clinical trials have demonstrated its profound benefits. In a phase III trial involving 31 participants, Luxturna administration yielded substantial improvements in visual function. These benefits were not fleeting; they were sustained for an impressive 3–4 years, showcasing the long-term potential of this gene therapy.
Safety has been a paramount consideration, and the trials have been reassuring. Notably, no severe adverse reactions were observed after one year of administration (ClinicalTrials.gov Identifier: NCT00999609), affirming its robust safety profile. Luxturna’s success has also spurred further investigations into other gene abnormalities linked to hereditary retinal disorders, with numerous ongoing clinical trials exploring similar approaches. This pioneering therapy from Roche represents a monumental step towards combating inherited blindness, offering a tangible path to restored sight.

5. **Gene Therapy for Spinal Muscular Atrophy (SMA) (Zolgensma)**Progress in managing rare metabolic diseases has also been a hallmark of 2025’s gene therapy landscape. Among these, treatments for spinal muscular atrophy (SMA) stand out as a significant achievement. SMA is a debilitating genetic disorder that affects the nerve cells responsible for controlling voluntary muscle movement, leading to muscle weakness and wasting. Gene therapy has offered a dramatic reversal of this progressive condition.
With a single-dose treatment, patients, particularly infants and young children, have shown dramatic improvements in muscle strength, movement, and crucially, life expectancy. This single intervention fundamentally alters the disease’s trajectory, offering a stark contrast to the previous prognosis for SMA. The ability of gene therapy to provide such profound and lasting benefits from a one-time administration highlights its potential to revolutionize care for these severe inherited conditions.
Novartis, a global leader in cell and gene therapy, has been at the forefront of this breakthrough with Zolgensma. As one of their pioneer therapies, Zolgensma delivers a functional copy of the SMN1 gene, which is defective in SMA patients, allowing the body to produce the necessary protein for motor neuron survival. This targeted genetic correction addresses the underlying cause of the disease, offering a long-term solution rather than continuous management of symptoms.
The success of Zolgensma and similar therapies for rare metabolic diseases underscores how gene therapy can offer true long-term solutions for conditions that previously demanded lifelong medications and frequent, often invasive, hospital visits. It represents a paradigm shift where complex genetic diseases can be effectively neutralized, providing improved quality of life and extended lifespans for affected individuals and their families.

6. **Gene Therapy for Pompe Disease**Building upon the triumphs seen in SMA, gene therapy has also made substantial strides in managing other rare metabolic diseases, including Pompe disease. This is another severe genetic disorder where the body cannot produce enough of an enzyme called acid alpha-glucosidase (GAA), leading to the accumulation of glycogen in cells and causing progressive muscle weakness, particularly in the heart and skeletal muscles. The advancements in gene therapy are now offering new hope for these patients.
Similar to other successful gene therapy interventions for rare conditions, the development for Pompe disease aims to provide a single-dose treatment that can restore the body’s ability to produce the missing enzyme. This genetic correction can prevent or significantly reduce the accumulation of glycogen, thereby halting or even reversing the disease’s devastating progression. Patients treated with these therapies have shown notable improvements in muscle function and overall health.
The promise of such treatments lies in their capacity to offer fundamental, long-term solutions. By addressing the enzyme deficiency directly at the genetic level, gene therapy for Pompe disease could free patients from the burden of frequent enzyme replacement therapy infusions. This transition from ongoing symptomatic management to a potential one-time corrective treatment profoundly enhances patient autonomy and quality of life.
These ongoing developments demonstrate the broad applicability of gene therapy principles across a spectrum of rare inherited metabolic disorders. The meticulous research and clinical trials in this area are designed to ensure both the safety and efficacy of these life-changing treatments, building on the knowledge gained from conditions like SMA. It’s a testament to the scientific community’s dedication to tackling diseases with previously limited therapeutic avenues.
7. **Gene Therapy for Beta-Thalassemia (Zynteglo)**Beyond the revolutionary CRISPR-based therapy of Casgevy, another significant breakthrough in the treatment of beta-thalassemia is Zynteglo. This gene therapy, developed by Bluebird Bio, received approval for beta-thalassemia requiring regular transfusions, offering a new, potentially curative option for patients who depend on frequent blood transfusions to survive. Its approval in August 2022 highlighted its crucial role in addressing a severe unmet medical need.
Zynteglo works by introducing a functional copy of the beta-globin gene into the patient’s own hematopoietic stem cells, which are then reinfused. This allows the body to produce healthy adult hemoglobin, thereby reducing or eliminating the need for chronic red blood cell transfusions. For individuals with transfusion-dependent beta-thalassemia, this treatment can dramatically improve their lives, freeing them from the constant cycle of hospital visits and associated complications.
Bluebird Bio, despite its competitive standing in the cell and gene therapy sector, has faced mounting pressure from larger rivals. However, the approval of Zynteglo, alongside Skysona and Lyfgenia, demonstrates their pioneering role in bringing gene therapies for ultra-rare diseases to market. While their therapies address smaller patient populations, their impact on those individuals is immense, generating revenue and solidifying their place in the gene therapy landscape.
The development and approval of Zynteglo exemplify the dedication required to advance gene therapies for rare genetic blood disorders. It provides a testament to the rigorous scientific development and clinical testing necessary to bring such complex treatments to patients. This therapy not only offers a new treatment modality but also represents hope for a future where inherited blood disorders can be effectively cured, transforming lives one gene at a time.
As we continue our journey through the revolutionary landscape of gene therapy in 2025, the depth and breadth of innovation are truly breathtaking. Beyond the foundational breakthroughs discussed, the field is pushing ever further, addressing a wider array of conditions with increasingly sophisticated and targeted approaches. These next advancements underscore the relentless pursuit of genetic solutions, bringing us closer to a future where many debilitating diseases are not just managed, but potentially cured at their very source.

8. **Gene Therapy for Retinitis Pigmentosa (RP)**Retinitis pigmentosa, or rod-cone dystrophy, represents a diverse group of hereditary diseases characterized by the initial deterioration of rod photoreceptor cells. This progressive loss is subsequently followed by cone photoreceptors and RPE degeneration, leading to a gradual and profound loss of vision. The underlying mechanism often involves a shortened rhodopsin due to genetic mutations, which significantly impairs the cells’ capacity for protein folding and transport, ultimately causing cell death through unfolded protein responses.
Patients afflicted with RP typically experience nyctalopia, or night blindness, as one of the earliest symptoms. As the disease advances, they face restricted visual fields and eventually central vision loss, severely impacting their daily lives. A range of genes, including Usher syndrome type IIA (USH2A, Usherin), retinitis pigmentosa 2 homolog (RP2), and phosphodiesterase 6B (PDE6B), are known to harbor harmful mutations associated with RP.
RP is broadly categorized into nonsyndromic and syndromic forms. The nonsyndromic variant exclusively causes retinal dystrophy without affecting other organs, impacting approximately one in 5,000 individuals, and can be inherited as autosomal-dominant (30-40% of cases), autosomal-recessive (50-60%), or X-linked traits (5-15%). Syndromic RP, on the other hand, presents with additional systemic disorders alongside retinal degeneration, exemplified by conditions like Leber congenital amaurosis (LCA), Usher syndrome, and Bardet–Biedl syndrome.
While Luxturna’s success for LCA, a specific form of syndromic RP caused by RPE65 mutations, has been a beacon, it has also propelled a surge of investigations into other gene abnormalities linked to hereditary retinal disorders. Numerous clinical trials are actively exploring similar gene therapy approaches. The future of personalized, precision RP treatment is being rapidly accelerated by technologies focusing on efficient vector delivery, CRISPR/Cas9, and induced pluripotent stem cells (iPSCs)-based cell transplants. Although challenges remain in ensuring long-term safety, developing efficient delivery systems, managing immune responses, and addressing the high costs, the potential for restoring sight remains a powerful motivator.

9. **Gene Therapy for X-linked Retinitis Pigmentosa (XLRP)**A distinct and challenging form of inherited retinal degeneration, X-linked Retinitis Pigmentosa (XLRP), is commonly caused by mutations in the RPGR (GTPase regulator) gene. This specific genetic defect leads to severe progressive vision loss, primarily affecting males due to its X-linked inheritance pattern. Addressing RPGR mutations has become a critical focus for gene therapy researchers.
Promising preclinical studies have demonstrated the potential of RPGR gene-editing using sgRNA (Cas9) and AAV vectors to preserve photoreceptors in mouse models of RPGR-related XLRP. Notably, subretinal injection of CRISPR-Cas9 AAV vectors has successfully reinstated the open reading frame of RPGRORF15 in a subset of cells, showing widespread distribution throughout the retina of rd9 mice. These findings laid a crucial foundation for clinical translation.
In human trials, a phase I/II clinical trial (NCT03116113) employed a dose-escalation design using a single subretinal injection of BIIB112, an AAV vector encoding codon-optimized human RPGR (AAV8-coRPGR). While safety concerns were observed, primarily limited to steroid-responsive subretinal inflammation in high-dose groups, the results were encouraging. Six patients exhibited notable improvements in their visual field, with benefits commencing at one month and sustained until the last follow-up assessment.
Further accelerating the field, a phase I/II dose escalation trial of rAAV2–RPGR for children and adults with XLRP caused by faulty RPGR has recently been completed, with results eagerly anticipated. Additionally, several other clinical studies are actively underway, including a phase I/II clinical trial (NCT03316560) assessing the safety and effectiveness of rAAV2tYF–GRK1–RPGR. Another significant phase III study (NCT05926583) is evaluating the safety and effectiveness of AAV5–hRKp.RPGR for treating Japanese XLRP patients with RPGR mutations.
These ongoing developments indicate a robust and dedicated effort to combat XLRP. Gene therapy offers a tangible possibility of reversing the damage caused by RPGR mutations, recovering eyesight, and fundamentally transforming the management of this debilitating condition. As our understanding of the precise molecular mechanisms underlying XLRP continues to improve, the emergence of novel and highly targeted therapeutic avenues appears increasingly likely.

10. **Gene Therapy for Age-related Macular Degeneration (AMD)**Age-related macular degeneration (AMD) stands as the leading cause of severe, permanent vision loss in adults over the age of 55, posing a significant public health challenge. This complex eye disease manifests in two primary forms: dry AMD, which involves the thinning of the macula, and the more aggressive neovascular (wet) AMD, characterized by abnormal blood vessel growth under the retina. Genetic factors play a crucial role in AMD pathogenesis, with at least 103 AMD-related genes or loci identified to date. Key contributors include changes in the CFH and HTRA1 loci, alongside genes related to lipid metabolism such as ApoE, tissue inhibitor of metalloproteinases-3 (TIMP3), and hepatic lipase.
Current clinical treatments for AMD include traditional approaches like laser and radiotherapy, as well as photodynamic therapy with ranibizumab for specific conditions like polypoidal choroidal vasculopathy. However, anti-VEGF therapy remains the primary therapeutic approach for neovascular AMD, utilizing pharmacological agents such as anti-VEGF monoclonal antibody fragments (pegaptanib, ranibizumab), fusion VEGF binding proteins (aflibercept, conbercept), and bevacizumab to suppress abnormal blood vessel growth.
Gene therapy has emerged as a particularly promising avenue for AMD treatment, offering the potential for long-term efficacy and reduced treatment burden. Research has demonstrated the long-term safety and effectiveness of AAV2 vector-mediated VEGF therapy. However, clinical development faces hurdles; a phase I/II trial (NCT03066258) for RGX-314, a rAAV vector containing coding sequences for soluble anti-VEGF, reported severe adverse events such as atrial fibrillation, retinal detachment, and visual impairment across different dose groups, with incidence rates ranging from 16.67% to 33.33% after 24 weeks.
In contrast, other trials have shown a more favorable safety profile. A phase I trial (NCT01024998) assessing the safety and tolerability of a single intravitreal administration of AAV2-sFLT01 revealed no severe eye-related adverse events, suggesting the approach is safe and well-tolerated across all dosage levels. Adverum Biotechnologies’ ADVM-022 is currently in a phase I clinical trial as an intravitreal gene therapy for neovascular AMD. Preliminary results have been encouraging, confirming its safety and efficacy in maintaining sustained levels of aflibercept, which could significantly reduce the treatment burden and improve vision outcomes for patients.
Beyond these, preclinical studies are expanding the therapeutic landscape. Suprachoroidal injections of RGX-314, an AAV8 vector expressing anti-VEGF-A Fab, have shown promising results in animal models, effectively suppressing VEGF-mediated vasodilation and vascular leakage in rats. Another potential therapy involves BT2, a dibenzoxazepinone, which has exhibited inhibitory effects on vascular permeability and angiogenesis by suppressing retinal CD31, phospho-extracellular signal-regulated kinase, vascular cell adhesion molecule-1, and VEGF-A 165 expression in neovascular AMD. Furthermore, human complement factor I carried by AAV constructs is also proving successful in preclinical investigations, highlighting the diverse strategies being explored to combat this pervasive cause of blindness.

11. **Gene Therapy for Duchenne Muscular Dystrophy (DMD)**Duchenne Muscular Dystrophy (DMD) stands as a severe, progressive genetic disorder that relentlessly leads to muscle degeneration and profound weakness. It primarily affects boys, caused by mutations in the dystrophin gene, which results in the absence or malfunction of the crucial dystrophin protein—a protein essential for maintaining the integrity and function of muscle cells. The relentless progression of DMD has long presented a significant challenge in medical treatment, leading to loss of ambulation, respiratory failure, and cardiac complications.
In a monumental step forward, gene therapy has emerged as a groundbreaking approach for DMD, offering hope where previously there was little. Sarepta Therapeutics has been at the forefront of this battle with their pioneering therapy, Elevidys. This revolutionary treatment is designed to deliver a micro-dystrophin gene, a truncated yet functional version of the dystrophin protein, to the patient’s muscle cells. Elevidys represents a significant advance in the therapeutic landscape for neuromuscular diseases, addressing the fundamental genetic defect.
The mechanism behind gene therapy for DMD involves utilizing viral vectors, typically AAV, to carry the modified dystrophin gene into the patient’s body. Once delivered to the muscle cells, this new genetic material enables the cells to produce the micro-dystrophin protein, which can then help to stabilize muscle fibers and reduce the rate of damage. This targeted genetic correction aims to compensate for the missing or defective dystrophin, thereby addressing the root cause of the disease rather than merely managing its symptoms.
Clinically, the impact of such gene therapies is profoundly important. While not a complete cure, these treatments hold the potential to slow disease progression, improve muscle strength, and significantly enhance the quality of life for individuals living with DMD. Companies like Solid Biosciences are also actively developing their own microdystrophin gene therapy candidates, contributing to a growing pipeline of innovative solutions. These advancements signify a transformative shift in the management of DMD, offering renewed hope for extended functional independence and improved long-term outcomes.

12. **Gene Therapy for Hemophilia**Hemophilia refers to a group of inherited bleeding disorders that severely impair the body’s ability to form blood clots, leading to prolonged bleeding after injury or surgery, and often spontaneous internal bleeding. These debilitating conditions are caused by deficiencies in specific clotting factors, most commonly Factor VIII (Hemophilia A) or Factor IX (Hemophilia B), significantly impacting patients’ quality of life and often requiring lifelong, frequent intravenous infusions of the missing clotting factor.
Gene therapy is now fundamentally reshaping the treatment paradigm for hemophilia, moving beyond continuous replacement therapy to offering a potential one-time, long-term solution. For Hemophilia A, BioMarin Pharmaceutical has emerged as a pioneer with its gene therapy, Roctavian. This innovative treatment aims to introduce a functional copy of the gene responsible for producing Factor VIII into the patient’s cells, ideally enabling the body to produce sufficient levels of the clotting factor itself, thereby reducing or eliminating the need for regular prophylactic infusions.
The advancements in gene therapy also extend to Hemophilia B, with several notable breakthroughs. Pfizer is actively developing Beqvez, a gene therapy designed to address the Factor IX deficiency. Similarly, uniQure, in collaboration with CSL Behring, has brought forward Hemgenix for Hemophilia B. These therapies deliver a functional gene for Factor IX, allowing for sustained endogenous expression of the clotting factor. This approach offers patients the promise of dramatically fewer bleeding episodes and a life less constrained by the constant need for treatment.
The overall impact of these gene therapies on hemophilia patients is nothing short of revolutionary. By providing a mechanism for sustained, in-body production of crucial clotting factors, they offer the promise of improved hemostatic control, a significant reduction in bleeding episodes, and a much-enhanced quality of life. This shift from chronic, reactive treatment to a potentially curative genetic intervention represents a monumental leap forward, fundamentally transforming how inherited blood disorders are managed and offering unprecedented liberation for patients.

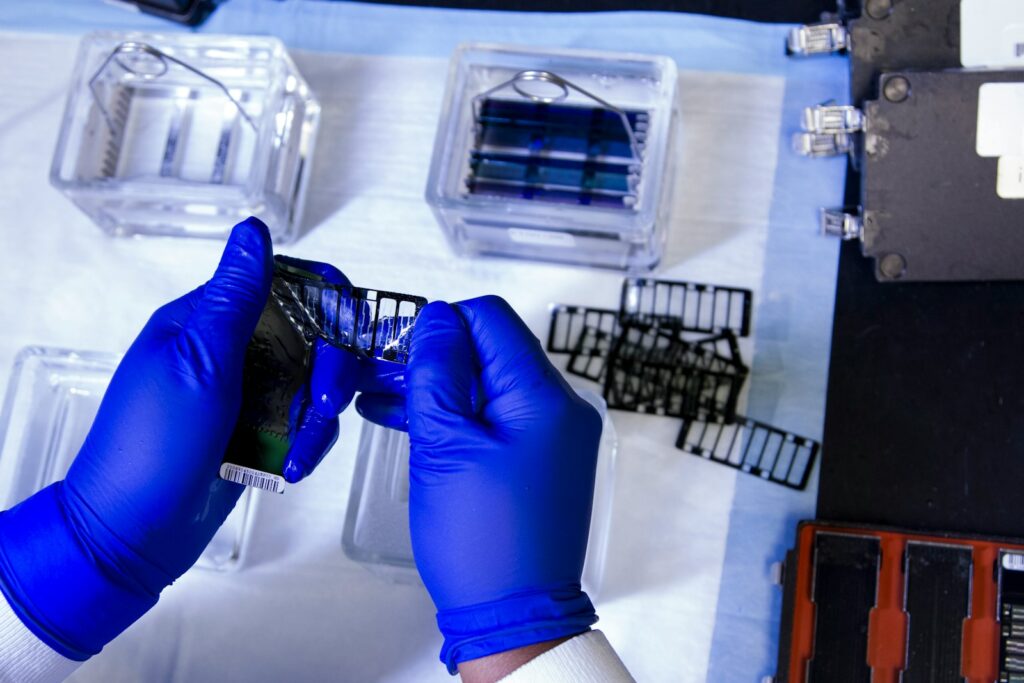
13. **Next-Generation Gene Editing and Delivery Platforms**Beyond the specific disease-focused treatments, some of the most profound breakthroughs in gene therapy are occurring at the foundational level, within the very technologies that enable genetic modification and delivery. These next-generation gene editing tools and advanced vector delivery systems are not just incremental improvements; they are fundamentally pushing the boundaries of genetic medicine, expanding its applicability and enhancing its safety and precision across a wider spectrum of conditions.
One of the most exciting areas is the advancement of *in vivo* CRISPR editing. Intellia Therapeutics, for instance, stands at the forefront of this innovation, having conducted the first systemic *in vivo* CRISPR trial. This revolutionary approach aims to deliver gene editing components directly into the patient’s body to correct genetic defects within living cells, bypassing the need to remove, modify, and reinfuse cells. This represents a major technical leap, streamlining the process and potentially making gene therapy accessible for systemic diseases that are difficult to target ex vivo.
The role of artificial intelligence (AI) in optimizing gene therapy components is also rapidly gaining traction. Dyno Therapeutics is pioneering the use of AI to design and optimize AAV (adeno-associated virus) capsids. This intelligent design process allows for the creation of more efficient, targeted, and safer viral vectors, ensuring that therapeutic genes are delivered precisely to the intended cells or tissues while minimizing off-target effects. This innovation is critical for enhancing the efficacy of treatments and broadening their therapeutic window.
Furthermore, the toolkit for gene editing continues to expand with the discovery of novel CRISPR systems and other cutting-edge platforms. Metagenomi, for example, is dedicated to discovering and developing new CRISPR systems, which promise to offer even greater precision, versatility, and fewer immunogenic responses than current tools. Companies like Editas Medicine and Caribou Biosciences are also continuously refining their CRISPR-based therapies, exploring innovative ways to apply gene editing for a diverse range of genetic disorders and cancers. These advancements are not merely about fixing one gene, but about building a robust and adaptable set of technologies that can tackle almost any genetic challenge.
These platform innovations are accelerating the pace of discovery and translation within the gene therapy sector. By improving the fundamental ability to edit genes with unparalleled precision and deliver them efficiently to target cells, they promise a future where gene therapies can be applied to an even wider array of diseases with greater safety and effectiveness. This relentless pursuit of next-generation technologies is truly ushering in a new era of personalized and curative genetic medicines, offering unprecedented hope for transforming human health.
Read more about: Microsoft’s Enduring Legacy: A Comprehensive Look at the Tech Giant’s Evolution from Software Pioneer to Global Conglomerate
In 2025, gene therapy is clearly demonstrating its power to rewrite the narrative of human disease. From curing inherited blood disorders and halting aggressive cancers to restoring lost vision and correcting rare metabolic defects, these breakthroughs are illuminating a path toward a future where genetic conditions are not just managed, but fundamentally overcome. The momentum is undeniable, and as our understanding of genetics deepens and technological capabilities advance, we stand on the cusp of an era where repairing the very blueprint of life becomes a routine, life-changing reality for millions.



