In an era increasingly focused on public health and the intricate connections between diet and disease, a new study has brought to light an unsettling truth about beverages that are ubiquitous in daily life: diet sodas and their sugary counterparts. For years, consumers have been navigating a complex landscape of dietary advice, often perceiving artificially sweetened drinks as a benign, or even beneficial, alternative to sugar-laden options. This perception, however, is now being rigorously challenged by emerging scientific evidence that compels a reevaluation of our beverage choices.
This latest research underscores a critical public health concern, revealing a direct and significant link between the regular consumption of both diet and sugary drinks and an increased risk of severe liver conditions. The findings call into question the very notion of a ‘healthy’ substitute when it comes to sweetened beverages, urging a deeper understanding of how these drinks impact our metabolic systems and, specifically, the health of our liver. As the global burden of noncommunicable diseases continues to rise, insights like these become indispensable for guiding informed personal choices and public health policies.
At the heart of this discussion is metabolic dysfunction-associated steatotic liver disease (MASLD), a condition rapidly gaining prominence as a leading cause of liver ailments worldwide. The implications of this new study extend far beyond individual dietary habits, resonating with broader efforts by international health organizations to address unhealthy eating patterns that contribute to a spectrum of noncommunicable diseases, including diabetes, heart disease, stroke, and various cancers. The collective evidence paints a clear picture: our daily drink choices carry profound and previously underestimated consequences for our long-term health.
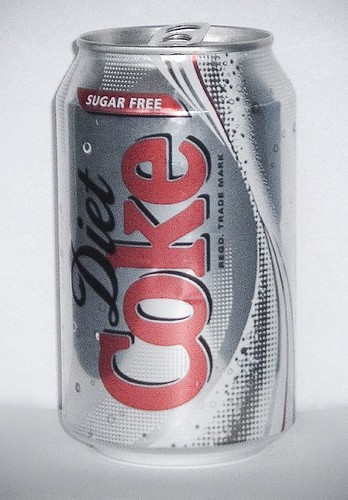
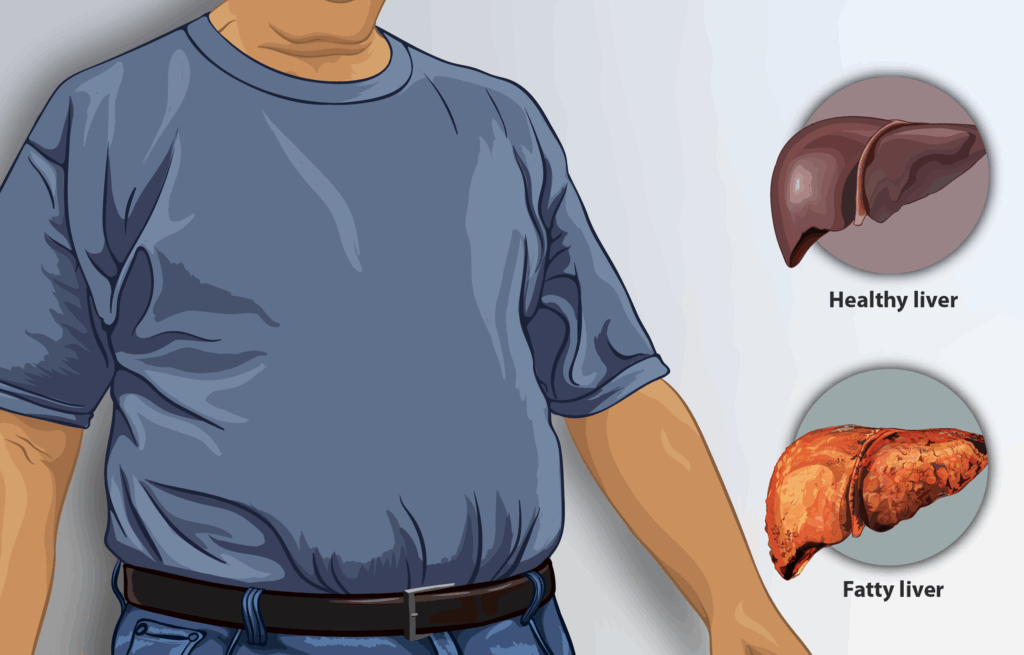
1. **The Alarming New Study on Diet Soda and MASLD Risk**Groundbreaking new research, unveiled on October 6 at the 2025 United European Gastroenterology Week conference in Berlin, Germany, has cast a stark new light on the risks associated with diet soda consumption. The study reveals an unsettling association between even modest intakes of artificially sweetened beverages and a heightened risk of developing metabolic dysfunction-associated steatotic liver disease, or MASLD, previously known as non-alcoholic fatty liver disease (NAFLD).
According to these new findings, consuming as little as 9 ounces of a single diet soda per day could elevate the risk of MASLD by a striking 60%. This amount is notably less than a standard 12-ounce can of soda, suggesting that even moderate consumption, often perceived as harmless or a ‘dietary cheat,’ carries significant health implications for the liver. The study meticulously tracked 124,000 individuals in the UK Biobank, who were initially free from liver disease, over a decade, utilizing detailed 24-hour dietary questionnaires.
Lihe Liu, a graduate student in the Department of Gastroenterology at the First Affiliated Hospital of Soochow University, Suzhou, China, and lead author of the study, emphasized the surprising nature of these results. Liu stated, “Our study shows that (low- or non-sugar-sweetened beverages) were actually linked to a higher risk of MASLD, even at modest intake levels such as a single can per day.” This statement directly challenges deeply ingrained assumptions about the safety profile of diet beverages, underscoring the urgent need for consumers and health professionals alike to reconsider their role in daily diets.

2. **Sugary Beverages: A Persistent Threat to Liver Health**The new research also reinforces long-standing concerns regarding the health impacts of traditional sugar-sweetened beverages. While diet sodas garnered particular attention for their unexpected risks, the study confirmed that sugary drinks are similarly implicated in the development of MASLD, increasing the risk by 50% with as little as 9 ounces per day. This adds a critical new dimension to the well-documented scrutiny that sugary drinks have faced for decades.
News surrounding the health risks of soda, especially those containing added sugars like cane and high-fructose corn syrup, is not new. The fizzy bubbles themselves, caused by carbon dioxide gas, along with many other ingredients within soda, affect one’s stomach more than some might realize. However, the specific pathway through which these sugars contribute to liver disease has become clearer, particularly concerning fructose.
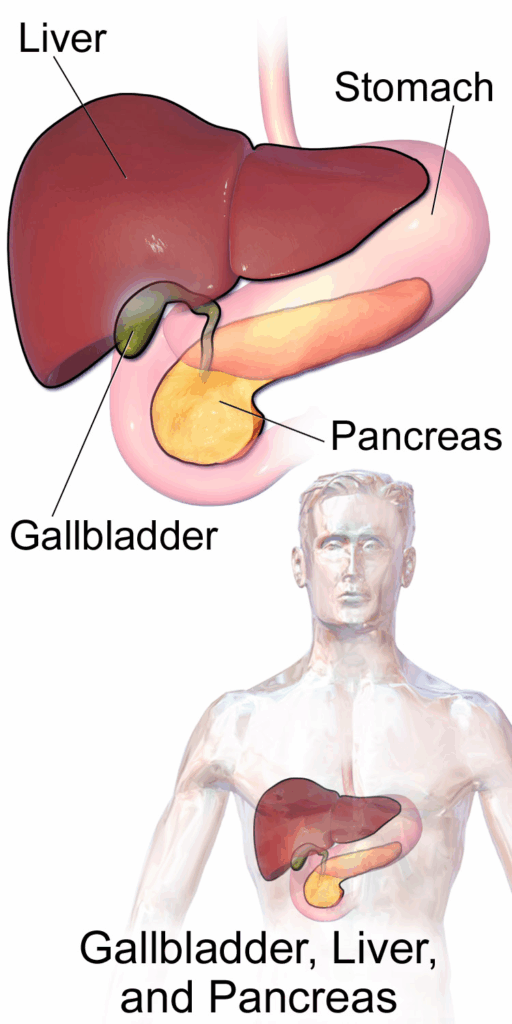
Dr. Wesley McWhorter, a spokesperson for the Academy of Nutrition and Dietetics, highlighted the metabolic intricacies, explaining that “Your body processes them similarly, but fructose is primarily metabolized in the liver. When consumed in excess, especially from sugary drinks and other concentrated sources, fructose can promote fat accumulation in the liver, a key contributor to non-alcoholic fatty liver disease.” This explains why the liver bears the brunt of excessive sugar intake, setting the stage for serious health complications.
3. **Understanding Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD)**Metabolic dysfunction-associated steatotic liver disease, or MASLD, is rapidly emerging as a silent epidemic, representing the most common global form of liver disease. This condition, previously recognized as non-alcoholic fatty liver disease (NAFLD), involves the accumulation of excessive fat within the liver cells, an alarming development that can occur even in individuals who consume little to no alcohol. The name change to MASLD reflects a broader understanding of its metabolic underpinnings.
The progression of MASLD is particularly concerning because the damage it inflicts can escalate to severe liver scarring, a condition known as cirrhosis. This scarring is comparable to the destructive effects observed in individuals with heavy alcohol use, highlighting the seriousness of the disease. Furthermore, MASLD is identified as one of the leading causes of liver cancer, underscoring its profound implications for public health and patient outcomes.
The prevalence of MASLD is staggering and continues to rise. Within the past three decades alone, NAFLD – its former designation – is estimated to have surged by 50% in the United States, illustrating the rapid increase in this liver ailment. Currently, nearly four out of ten people in the country are afflicted with NAFLD, making it a widespread and pressing health crisis that demands immediate attention and effective preventative strategies.

4. **The Mechanisms: How Sugars and Fructose Impact the Liver**The critical role of sugar, particularly fructose, in the development of MASLD lies in its unique metabolic pathway within the human body. As Dr. Wesley McWhorter elucidated, while various sugars are processed similarly, “fructose is primarily metabolized in the liver.” This distinction is crucial, as an overload of fructose can overwhelm the liver’s capacity to process it efficiently, leading to detrimental effects.
When fructose is consumed in excessive amounts, particularly from concentrated sources such as sugary drinks, the liver converts this surplus into fat. This process, known as *de novo lipogenesis*, promotes fat accumulation directly within the liver cells. This hepatic fat accumulation is the defining characteristic of non-alcoholic fatty liver disease, now termed MASLD, making sugary beverages a significant dietary culprit in its development.
Beyond direct fat accumulation, the consumption of foods and drinks high in free sugars contributes to excess caloric intake, which in turn leads to unhealthy weight gain, overweight, and obesity. Obesity is a major risk factor for MASLD and a host of other noncommunicable diseases (NCDs). Recent scientific evidence further indicates that free sugars can adversely influence blood pressure and serum lipids, suggesting that reducing free sugars intake can mitigate risk factors for cardiovascular diseases, highlighting the multifaceted negative impact of these sweeteners on metabolic health.

5. **Challenging the “Healthier Choice” Perception of Diet Alternatives**For many years, diet alternatives to sugar-sweetened beverages have been widely marketed and perceived by the public as the healthier option, a way to enjoy familiar tastes without the caloric burden of sugar. However, the new study critically challenges this entrenched perception. Lihe Liu, the lead author, observed, “(Sugar-sweetened beverages) have long been under scrutiny, while their ‘diet’ alternatives are often seen as the healthier choice. Both, however, are widely consumed and their effects on liver health have not been well understood.”
This insight is particularly impactful because it means that even when individuals consciously choose diet sodas to ‘avoid some of the bad,’ they may inadvertently be exposing themselves to other, equally concerning health risks. The study’s finding that low- or non-sugar-sweetened beverages were linked to a higher risk of MASLD, even at modest intake levels, directly contradicts the common assumption that these drinks are harmless. It signifies a profound need to reconsider their role in diet and liver health, especially given MASLD’s emergence as a global health concern.
Moreover, the Cleveland Clinic suggests that the brain’s reaction to artificial sweeteners might mimic its response to sugary sweets. Frequent ingestion of artificial sweeteners could potentially amplify cravings for high-calorie foods, thereby increasing the risk of weight gain. This suggests that the perceived benefit of calorie reduction in diet drinks may be offset by an altered metabolic response and increased desire for other unhealthy foods, making the choice of diet soda far from unequivocally beneficial.
Read more about: Nourishing Your Future: 8 Groundbreaking Food Insights for Health and Vitality After 40

6. **The Critical Role of Water in Liver Protection and Overall Health**Amidst the sobering revelations about the risks posed by diet and sugary sodas, a clear and fundamental solution emerges: water. Health experts consistently advocate for water as the optimal choice for hydration, and the new study provides compelling evidence of its protective benefits. When feelings of thirst arise, reaching for a glass of water is, perhaps, the most prudent action one can take for liver health and overall well-being.
Crucially, the study investigating the links between sweetened beverages and MASLD also examined the impact of substituting these drinks with water. Researchers observed a significant reduction in risk for those who made this simple switch. Specifically, participants who replaced sugary beverages with water experienced a 13% lower risk of MASLD, while those who substituted diet drinks saw an even greater reduction of more than 15%.
Sajid Jalil, a clinical associate professor of gastroenterology and hepatology at Stanford University School of Medicine, underscored this vital message, stating, “The study showed that both regular and diet soft drinks may harm the liver over time, while choosing water or unsweetened drinks could help protect it.” This reinforces the long-held dietary wisdom that emphasizes consuming plenty of water, along with a diverse intake of fruits, vegetables, legumes, nuts, and whole grains, as cornerstones of a truly healthy diet.
Read more about: Sandra Bullock’s Ageless Radiance: Unveiling the Skincare Secrets That Keep Her Forever Young

7. **The Broader Implications: A Call for Reassessment of Dietary Habits**The findings of this new research on diet and sugary sodas and their link to MASLD serve as a powerful catalyst for a comprehensive reassessment of our collective dietary habits. It highlights a critical component within the larger landscape of unhealthy dietary patterns that have taken root globally, driven by factors such as the increased production of processed foods, rapid urbanization, and evolving lifestyles. These societal shifts have unfortunately led to a widespread consumption of foods high in energy, fats, free sugars, and salt/sodium, often at the expense of vital nutrients found in fruits, vegetables, and dietary fiber.
This reevaluation is not merely about individual choices; it resonates with the urgent calls from global health organizations. For instance, WHO Member States have agreed to ambitious targets, including halting the rise in diabetes and obesity among adults, adolescents, and children by 2025. The pervasive consumption of sweetened beverages directly undermines these critical public health objectives, exacerbating the prevalence of conditions that place immense strain on healthcare systems worldwide.
Ultimately, a healthy diet is recognized as a fundamental shield against malnutrition in all its forms and against the growing tide of noncommunicable diseases, including diabetes, heart disease, stroke, and cancer. The insights from this study underscore that even seemingly innocuous dietary elements, like sweetened drinks, play a significant and potentially detrimental role in this broader health equation. It necessitates a deeper, more critical look at the ingredients in our food and drink supply and how they contribute to or detract from a healthy life. The shift away from these beverages is not just a personal health decision, but a vital step in addressing a global health challenge.
The revelations about sweetened beverages and their impact on liver health compel us to look beyond individual dietary choices and toward the broader frameworks that guide public health. Understanding these new findings within the context of established global dietary guidelines and robust public health initiatives is paramount. These frameworks are not just theoretical constructs; they are practical tools designed to foster healthy eating and mitigate the pervasive health risks now starkly illuminated by the liver disease research.

8. **Global Dietary Guidelines: Foundations for Lifelong Health**A healthy diet forms the bedrock of protection against malnutrition in all its forms and serves as a primary defense against noncommunicable diseases (NCDs) such as diabetes, heart disease, stroke, and cancer. These foundational principles are universally applicable, though their specific manifestation can vary with individual characteristics like age, gender, lifestyle, and cultural context. The essential components, however, remain constant, guiding individuals and populations toward optimal health.
Central to these guidelines is the concept of energy balance: caloric intake must align with energy expenditure to prevent unhealthy weight gain. Beyond this fundamental balance, specific macronutrient recommendations are critical. For instance, total fat intake should not surpass 30% of total energy, with a crucial emphasis on reducing saturated fats to less than 10% and trans-fats to less than 1%. The shift towards unsaturated fats is strongly advised, particularly the elimination of industrially-produced trans-fats, which have no place in a healthy diet.
Further refinement of these guidelines targets sugar and salt consumption. Limiting free sugars to less than 10% of total energy intake is considered a healthy practice, with a further reduction to less than 5% suggested for additional health benefits. Similarly, keeping salt intake below 5 grams per day, equivalent to less than 2 grams of sodium, is crucial for preventing hypertension and reducing the risk of cardiovascular diseases. These precise recommendations collectively form a comprehensive strategy to safeguard metabolic and overall health.

9. **Prioritizing Whole Foods: The Indispensable Role of Fruits, Vegetables, and Whole Grains**The cornerstone of a balanced diet, as consistently advocated by health authorities, lies in the abundant consumption of fruits, vegetables, legumes, nuts, and whole grains. These food groups are rich in essential nutrients and dietary fiber, providing a natural defense against NCDs and supporting overall metabolic function. The recommendations are explicit, calling for at least 400 grams, or five portions, of fruits and vegetables per day, excluding starchy roots like potatoes and cassava.
Incorporating these vital foods into daily life can be straightforward with a few practical strategies. Always including vegetables in meals, opting for fresh fruit and raw vegetables as snacks, and prioritizing seasonal produce are effective ways to increase intake. Furthermore, aiming for a wide variety of fruits and vegetables ensures a broad spectrum of nutrients, maximizing the health benefits derived from these natural powerhouses.
This emphasis on whole, unprocessed foods directly counters the dietary patterns that contribute to conditions like MASLD. By filling our plates with nutrient-dense options, we naturally reduce the space and craving for processed foods high in free sugars and unhealthy fats. This shift is not merely about avoiding harm; it is about actively building resilience and promoting liver health through superior nutrition.

10. **Strategic Reduction: Tackling Unhealthy Fats and Excessive Salt**Beyond prioritizing whole foods, a healthy diet necessitates a strategic reduction in certain components, particularly unhealthy fats and excessive salt. Reducing total fat intake to less than 30% of total energy helps prevent unhealthy weight gain, a significant risk factor for MASLD. This involves a crucial shift away from saturated fats, which should constitute less than 10% of total energy, and industrially-produced trans-fats, which should be less than 1% and ideally eliminated entirely, towards beneficial unsaturated fats found in sources like fish, avocados, nuts, and certain oils.
Beyond prioritizing whole foods, a healthy diet necessitates a strategic reduction in certain components, particularly unhealthy fats and excessive salt. Reducing total fat intake to less than 30% of total energy helps prevent unhealthy weight gain, a significant risk factor for MASLD. This involves a crucial shift away from saturated fats, which should constitute less than 10% of total energy, and industrially-produced trans-fats, which should be less than 1% and ideally eliminated entirely, towards beneficial unsaturated fats found in sources like fish, avocados, nuts, and certain oils.
Practical adjustments in cooking and food choices can significantly impact fat intake. Opting for steaming or boiling over frying, replacing butter and lard with polyunsaturated-rich oils like soybean or sunflower oil, and choosing reduced-fat dairy and lean meats are effective strategies. Limiting the consumption of baked and fried foods, and pre-packaged snacks that often contain industrially-produced trans-fats, is equally important for long-term health.
Similarly, managing salt intake is critical for preventing hypertension, heart disease, and stroke. Most individuals consume far too much sodium, largely from processed foods. To combat this, limiting added salt and high-sodium condiments during cooking, avoiding table salt, and selecting lower-sodium products are advised. Checking nutrition labels is a simple yet powerful tool for consumers to make informed choices. Increasing potassium intake through fresh fruits and vegetables can further mitigate the adverse effects of elevated sodium consumption, offering a dual approach to cardiovascular and overall health.

11. **Policy and Regulatory Interventions: Shaping a Healthier Food Environment**Creating a healthy food environment requires more than individual effort; it demands concerted action from governments and various stakeholders. Governments play a pivotal role in this transformation by fostering policies and investment plans that actively promote healthy diets and safeguard public health. This involves aligning national policies across trade, food, and agriculture to achieve coherent health outcomes, moving beyond a narrow focus on production to encompass the health impacts of food systems.
Effective policy interventions include increasing incentives for producers and retailers to cultivate and sell fresh fruits and vegetables, thereby enhancing their availability and affordability. Concurrently, reducing incentives for the food industry to continue producing processed foods high in saturated fats, trans-fats, free sugars, and salt is essential. Policymakers should also encourage the reformulation of food products to reduce these harmful components, with a clear goal of eliminating industrially-produced trans-fats altogether.
Further regulatory measures are vital. Implementing WHO recommendations on the marketing of foods and non-alcoholic beverages to children can shield younger generations from pervasive unhealthy influences. Establishing standards to ensure the availability of healthy, nutritious, safe, and affordable foods in public institutions like schools and workplaces, alongside exploring regulatory instruments like nutrition labeling and economic incentives such as taxation on unhealthy products, are crucial steps. Moreover, encouraging food services to improve their nutritional quality, offer healthy choices, and review portion sizes contributes to a pervasive culture of wellness.

12. **Empowering the Consumer: Education and Awareness as Protective Tools**While policies lay the groundwork, empowering consumers with knowledge and practical skills is equally vital for driving demand for healthy foods. Promoting widespread consumer awareness of what constitutes a healthy diet is a fundamental step, enabling individuals to make informed choices that benefit their well-being. This educational effort should begin early and continue throughout life, integrating nutrition literacy into daily routines.
Schools, in particular, serve as crucial environments for fostering healthy habits. Developing robust school policies and programs that encourage children to adopt and maintain healthy diets, alongside educating children, adolescents, and adults about nutrition and healthy dietary practices, builds a foundation for lifelong wellness. Furthermore, encouraging culinary skills, even among children in school settings, can empower individuals to prepare nutritious meals at home, reducing reliance on processed options.
Point-of-sale information, including clear and standardized nutrition labeling that adheres to Codex Alimentarius Commission guidelines, is another powerful tool. The addition of front-of-pack labeling can significantly facilitate consumer understanding, enabling quick and easy identification of healthier choices. Complementing these initiatives, providing accessible nutrition and dietary counseling at primary health-care facilities ensures that individuals receive personalized guidance to navigate their dietary needs effectively, turning knowledge into actionable health improvements.

13. **Nurturing Early Health: Optimal Nutrition for Infants and Young Children**The foundation of lifelong health is laid in the earliest stages of life, making optimal nutrition for infants and young children critically important. Healthy dietary practices must begin early, with exclusive breastfeeding recommended during the first six months of life, and continued breastfeeding until two years of age and beyond. This crucial practice not only fosters healthy growth and cognitive development but also offers long-term benefits, significantly reducing the risk of becoming overweight or obese and developing NCDs later in life.
From six months onward, breast milk should be complemented with a diverse array of adequate, safe, and nutrient-dense foods. A key directive during this period is to avoid adding salt and sugars to complementary foods, preventing the early introduction of habits that can contribute to later health problems. These early nutritional experiences shape taste preferences and metabolic programming, influencing health outcomes for decades.
To support these vital practices, global initiatives such as the International Code of Marketing of Breast-milk Substitutes and subsequent World Health Assembly resolutions are crucial in protecting breastfeeding from commercial pressures. Policies that promote the protection of working mothers and support breastfeeding in health services and communities, exemplified by the Baby-friendly Hospital Initiative, create an environment where optimal infant and young child feeding can thrive. These collective efforts safeguard the health of the youngest populations, building a healthier future generation.

14. **Global Commitment: WHO’s Vision for a Healthier World Through Diet**The global health community, spearheaded by the World Health Organization (WHO), has long recognized the profound impact of diet on public health and has established ambitious strategies to address it. The adoption of the “WHO Global Strategy on Diet, Physical Activity and Health” in 2004 marked a pivotal moment, rallying governments, international partners, the private sector, and civil society to take coordinated action. This strategy provides a comprehensive blueprint for supporting healthy diets and physical activity worldwide, laying the groundwork for subsequent, more targeted interventions.
Further solidifying this commitment, WHO has implemented specific initiatives to tackle key drivers of unhealthy diets. In 2010, recommendations on the marketing of foods and non-alcoholic beverages to children were endorsed, guiding countries in developing policies to reduce the harmful impact of advertising on young audiences. The “Comprehensive Implementation Plan on Maternal, Infant and Young Child Nutrition,” adopted in 2012, set six global nutrition targets to be achieved by 2025, including a halt to the rise in diabetes and obesity among adults, adolescents, and children.
The global commitment extends to comprehensive NCD prevention and control. The 2013–2020 Global Action Plan provided guidance to achieve targets such as a 30% reduction in salt intake by 2025. Recognizing the alarming rise in childhood obesity, the Commission on Ending Childhood Obesity was established in 2014, proposing recommendations to tackle this global challenge. Furthermore, the Second International Conference on Nutrition (ICN2) in 2014 resulted in the Rome Declaration on Nutrition and a Framework for Action, reinforcing the importance of diversified, safe, and healthy diets. Through these robust strategies and collaborative efforts, WHO continues to champion a future where healthy diets are accessible and integral to global well-being, actively working to mitigate the health risks highlighted by the latest liver disease research and foster truly healthy lives for all. The journey is ongoing, but the direction is clear: towards a world where informed choices, supported by sound policies and a vibrant food environment, empower every individual to thrive.


