If you’ve been faithfully taking your vitamin D supplements but still come up deficient on labs, you’re certainly not alone in this frustrating experience. Many individuals meticulously adhere to their supplement regimen, yet their blood tests consistently reveal stubbornly low serum levels. This common dilemma points to a deeper, more complex issue than simply not taking enough of the ‘sunshine vitamin.’
Vitamin D is far more than just a nutrient; it functions as a hormone-like substance, critical for an astonishing array of bodily processes. It plays a vital role in immune defense, helping your body ward off infections, and is deeply involved in mood and mental health, often linked to conditions like depression. Beyond these, it’s essential for hormone balance, efficient calcium absorption and robust bone density, and even has a significant hand in controlling inflammation throughout the body. Its influence extends to gene expression, underscoring its foundational importance to overall health.
However, the effectiveness of your vitamin D supplement isn’t solely dependent on the dose you take; it’s intricately tied to how your body absorbs, processes, and utilizes it. The answer to why your supplement might not be working lies in a complex interplay between genetics, chronic inflammation, your gut health, and other physiological factors. Understanding these underlying ‘absorption killers’ is the first step toward a more targeted and effective approach to optimizing your vitamin D levels, moving beyond the guesswork to real solutions.

1. **Gene Mutations & Methylation Issues**One of the most significant yet often overlooked reasons for persistent vitamin D deficiency, despite supplementation, lies within our very genetic makeup. Some gene mutations can profoundly affect how your body processes and metabolizes vitamin D, making it difficult for the nutrient to be properly absorbed and converted into its active form. These genetic variations can alter enzyme functions crucial for vitamin D pathways, meaning that even a perfectly good supplement might not be utilized efficiently by your system.
Methylation, a fundamental biochemical process occurring billions of times per second in every cell of the body, is intimately linked to these genetic predispositions. It plays a critical role in numerous bodily functions, including DNA repair, immune function, energy production, and detoxification. When gene mutations interfere with the methylation cycle, it can create a cascade of metabolic inefficiencies that directly or indirectly impact the absorption and utilization of key nutrients, including vitamin D. This means your body might not be equipped to fully process the vitamin D you’re providing.
For individuals with such genetic mutations, the standard oral vitamin D supplements may simply not provide the desired therapeutic effect because the underlying biological machinery for processing it is compromised. This isn’t a failure of the supplement itself, but rather a reflection of your body’s unique biochemical landscape. The inability to properly methylate can lead to a buildup of intermediate compounds or a deficiency in critical cofactors, further disrupting the complex dance of vitamin D metabolism.
Fortunately, advancements in genetic testing now allow for the identification of specific mutations that impact vitamin D metabolism. This invaluable insight can transform a generalized supplementation strategy into a highly personalized one. Armed with this knowledge, healthcare providers can recommend tailored interventions, often including personalized supplementation with methylated nutrients. These specialized forms of nutrients, such as methylated folate and B12, are designed to be more readily utilized by the body, effectively bypassing the genetic roadblocks and supporting the optimal processing of vitamin D.
2. **MTHFR Gene Mutations**Among the various gene mutations that can disrupt vitamin D efficacy, the MTHFR (methylenetetrahydrofolate reductase) gene mutation is particularly noteworthy and increasingly recognized. The MTHFR gene provides instructions for making an enzyme that is critical for processing folate, a B vitamin that plays a central role in methylation. When this gene has mutations, the enzyme’s ability to function is impaired, leading to a less efficient methylation process throughout the body.
While an MTHFR mutation doesn’t directly cause vitamin D malabsorption, its downstream effects can significantly impede the body’s ability to utilize vitamin D effectively. A compromised methylation cycle can affect the production of various cofactors and the overall biochemical environment necessary for vitamin D conversion and action. This indirect impact means that even if vitamin D is absorbed, its journey to become biologically active and exert its many health benefits can be severely hampered.
Individuals with MTHFR mutations often struggle with a range of health issues due to impaired methylation, which can include difficulties in detoxification, neurotransmitter production, and homocysteine regulation. In this context, standard oral vitamin D supplements may not be sufficient to overcome the systemic inefficiencies created by the MTHFR mutation. The body’s intricate network of biochemical pathways is interconnected, and a disruption in one area, like methylation, can create ripple effects that undermine the effectiveness of nutrient intake in others, such as vitamin D metabolism.
This specific genetic challenge highlights why a ‘one-size-fits-all’ approach to vitamin D supplementation often falls short. For those identified with MTHFR gene mutations, alternative strategies are frequently necessary to achieve optimal vitamin D levels. The context specifically notes that injectable vitamin D bypasses the digestive tract, making it ideal for those with “MTHFR gene mutations.” This underscores the need for approaches that circumvent the body’s internal processing challenges, delivering the nutrient directly to the bloodstream for better utilization.

3. **Chronic Inflammation**Chronic inflammation, often described as a silent epidemic, serves as a pervasive barrier to effective vitamin D absorption and utilization. Unlike acute inflammation, which is a healthy, short-term response to injury or infection, chronic inflammation is a prolonged and often low-grade inflammatory state that can silently wreak havoc on virtually every system in the body. This persistent inflammatory environment creates a hostile landscape for nutrient absorption and metabolism, significantly hindering the benefits of vitamin D supplementation.
When the body is in a state of chronic inflammation, systemic processes are dysregulated, and the efficiency of nutrient uptake is compromised. Inflammation in the gut, for instance, can drastically reduce the absorption of fat-soluble vitamins like vitamin D. This isn’t just about the gut; systemic inflammation can impact cellular receptors and enzyme activities crucial for the proper conversion and activation of vitamin D within the body. Essentially, your body becomes less adept at processing and utilizing the vitamin D you are consuming.
Conditions characterized by chronic inflammation, such as autoimmune diseases, irritable bowel syndrome (IBS), or even generalized low-grade systemic inflammation, can create an environment where vitamin D is not properly absorbed or metabolized. The inflammatory cytokines and other mediators released during chronic inflammation can interfere with the vitamin D receptor (VDR) signaling, effectively blocking vitamin D’s ability to exert its beneficial effects, even if it manages to get into the bloodstream. This creates a vicious cycle, as optimal vitamin D levels are crucial for inflammation control.
The widespread impact of chronic inflammation means that addressing this underlying issue is paramount for anyone struggling with persistent vitamin D deficiency. Simply increasing the dose of an oral supplement might not be enough to overcome the inhibitory effects of a continuously inflamed system. As the context suggests, a full panel including vitamin D and a CRP (C-reactive protein, a common inflammation marker) test can provide crucial insights into your inflammatory status. Identifying and managing chronic inflammation is a cornerstone of ensuring your vitamin D can truly work for you.
Read more about: Listen Up: 14 Critical Signs Your Body Is Quietly Signaling Nutrient Deficiencies
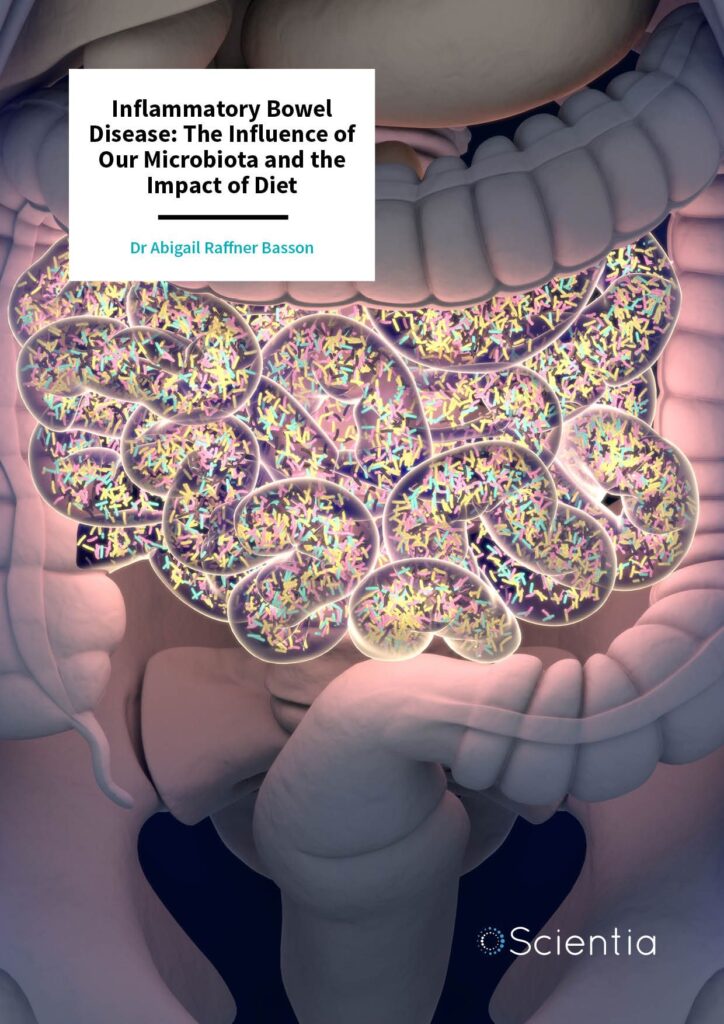
4. **Compromised Gut Health (Leaky Gut, IBS)**Intimately linked with chronic inflammation, the state of your gut health profoundly dictates your ability to absorb and utilize essential nutrients, including fat-soluble vitamins like D. A compromised gut, often manifesting as conditions like ‘leaky gut’ (increased intestinal permeability) or Irritable Bowel Syndrome (IBS), is a major ‘absorption killer’ for vitamin D supplements. The efficiency of your digestive tract is fundamental to extracting and absorbing the nutrients from the food you eat and the supplements you take.
In cases of leaky gut, the tight junctions between the cells lining your small intestine become compromised, allowing undigested food particles, toxins, and microbes to ‘leak’ into the bloodstream. This triggers a systemic inflammatory response, which, as discussed, further inhibits nutrient absorption. More directly, a damaged or inflamed gut lining simply cannot efficiently transport fat-soluble vitamins into the body. These vitamins require a healthy, intact intestinal wall for their proper uptake, and a compromised barrier significantly diminishes this capacity.
Conditions like IBS, characterized by chronic digestive discomfort, bloating, and irregular bowel habits, also signify a gut environment that is far from optimal for nutrient absorption. The dysbiosis (imbalance of gut bacteria) and inflammation often associated with IBS can impair the secretion of bile, which is essential for emulsifying dietary fats, and therefore, for absorbing fat-soluble vitamins. Without proper fat digestion and a healthy gut lining, the vitamin D from your supplement may pass through your system largely unabsorbed, rendering your efforts ineffective.
Ultimately, the principle is clear and unwavering: “Poor gut function = poor nutrient absorption.” This highlights that merely taking a vitamin D supplement without addressing underlying gut issues is akin to trying to fill a leaky bucket. To truly optimize your vitamin D levels, a comprehensive approach to gut health is indispensable. The context explicitly advises to “Improve Gut Health – Address inflammation, food sensitivities, and gut permeability,” emphasizing the actionable steps you can take to rebuild your digestive integrity and enhance your body’s ability to absorb vital nutrients.

5. **Specific Malabsorption Syndromes**Beyond general gut health issues and low-grade inflammation, certain distinct clinical conditions, known as malabsorption syndromes, present a severe and direct barrier to nutrient uptake, making vitamin D supplements largely ineffective. These syndromes represent a more profound impairment of the small intestine’s ability to adequately absorb nutrients from digested food, including fat-soluble vitamins like D. They are not merely mild digestive upsets but rather significant physiological dysfunctions that severely impede the body’s capacity to derive nutritional benefit from ingested substances.
Malabsorption syndromes often involve damage to the intestinal lining, enzyme deficiencies, or issues with bile production and flow, all of which are crucial for the digestion and absorption of fats and, by extension, fat-soluble vitamins. For instance, conditions affecting the pancreas (which produces digestive enzymes) or the liver and gallbladder (which produce and store bile) can dramatically reduce the availability of these critical components needed for vitamin D absorption. When these systems are compromised, the vitamin D, even if consumed in adequate amounts, simply cannot enter the bloodstream efficiently.
The challenges posed by malabsorption syndromes are particularly acute for fat-soluble vitamins because their absorption mechanism is more complex than that of water-soluble vitamins. They require the presence of dietary fats and bile salts to form micelles, which are then absorbed by the intestinal cells. In the presence of a malabsorption syndrome, this intricate process is severely disrupted or entirely circumvented. Consequently, individuals with such conditions will continue to exhibit low vitamin D levels despite diligent oral supplementation, as their digestive system is fundamentally unable to process and absorb it.
Recognizing the profound impact of these syndromes, the context highlights “Malabsorption syndromes” as one of the key reasons why injectable vitamin D is ideal. For these individuals, bypassing the digestive tract entirely by administering vitamin D directly into the bloodstream becomes not just a preference, but a medical necessity. Injectable vitamin D ensures that the nutrient is absorbed directly into circulation, circumventing the compromised gastrointestinal system and providing a reliable pathway to raise and maintain optimal vitamin D levels, offering a vital solution where oral supplements have consistently failed.
Navigating the complexities of vitamin D absorption extends beyond the foundational issues of genetics, inflammation, and gut health. A myriad of other intricate factors can subtly, yet significantly, undermine your body’s ability to effectively use this crucial nutrient. These additional ‘absorption killers’ often intertwine with one another, creating a challenging landscape for achieving optimal vitamin D levels, even with diligent supplementation. Understanding these deeper influences is paramount for anyone seeking to finally resolve their persistent deficiency and unlock vitamin D’s full spectrum of health benefits.
Let’s delve into these often-overlooked yet critical aspects, moving us closer to a truly personalized and effective strategy for vitamin D optimization. It’s about recognizing that your body’s unique biochemistry is constantly interacting with its environment and internal state, demanding a holistic approach to wellness.
6. **Specific Autoimmune Responses**While chronic inflammation broadly impacts vitamin D efficacy, specific autoimmune responses represent a more targeted and persistent challenge. Autoimmune diseases, characterized by the immune system mistakenly attacking healthy body tissues, create a unique physiological environment that can directly interfere with vitamin D pathways. These conditions often involve heightened and sustained inflammatory signals, which, as we’ve discussed, are inherently hostile to efficient nutrient utilization and metabolism.
In many autoimmune disorders, the very cells that are meant to respond to vitamin D — immune cells like T cells and B cells — may have dysregulated vitamin D receptors (VDRs). These VDRs are like locks on the cellular surface, and vitamin D is the key. If the locks are compromised or the signaling pathways downstream are disrupted due to ongoing immune attack, even an adequate amount of circulating vitamin D may not be able to exert its full immunomodulatory effects. This means the critical role vitamin D plays in immune defense and inflammation control can be severely blunted in individuals facing autoimmune challenges.
The relationship between vitamin D and autoimmunity is often a two-way street. Lower vitamin D status is frequently observed in individuals with autoimmune conditions and is inversely associated with the rates of many infections and chronic disorders. Conversely, an autoimmune state can make it harder to achieve optimal vitamin D levels, creating a vicious cycle where deficiency might exacerbate the condition, and the condition itself impedes effective vitamin D action. This intricate interplay underscores why simply increasing oral vitamin D intake might not be sufficient for those with specific autoimmune responses.
For individuals with autoimmune disorders, a targeted approach is essential. This often involves not only rigorous monitoring of vitamin D levels (aiming for optimal ranges of 60–80 ng/mL, as opposed to simply “normal” levels) but also comprehensive management of the underlying autoimmune condition itself. Injectable vitamin D can be particularly beneficial in these cases, as it bypasses potential gastrointestinal absorption issues often associated with autoimmune diseases and delivers the nutrient directly, ensuring greater bioavailability to immune cells that might be struggling with utilization.
Read more about: Listen Up: 14 Critical Signs Your Body Is Quietly Signaling Nutrient Deficiencies

7. **The Dynamics of Fat Cell Storage**Vitamin D is a fat-soluble vitamin, which means it requires dietary fat for absorption and is stored in the body’s adipose (fat) tissue. While this storage mechanism is generally beneficial, acting as a reserve, it can become a significant “absorption killer” in individuals with higher body fat percentages, such as those who are overweight or obese. The dynamics of fat cell storage can effectively sequester vitamin D, making it less available for the body’s critical functions.
When there’s an increased amount of adipose tissue, fat cells tend to “trap” vitamin D, diverting it away from the bloodstream where it’s needed to be converted into its active forms and utilized by various tissues and organs. This sequestration means that despite consuming adequate amounts of vitamin D—either through diet or oral supplements—the amount circulating in the blood (as measured by serum 25(OH)D) can remain stubbornly low. This physiological phenomenon creates a paradox where individuals may be taking their supplements diligently but still show deficiency on lab tests.
The scientific literature consistently supports this observation, noting that serum 25-hydroxyvitamin D concentration (25(OH)D) is inversely associated with obesity. The more body fat an individual carries, the greater the potential for vitamin D to be held hostage in adipose tissue, reducing its bioavailability for immune defense, bone health, mood regulation, and inflammation control. This is a critical distinction, as having vitamin D stored away is not the same as having it actively circulating and performing its hormone-like functions throughout the body.
Therefore, for individuals struggling with obesity or higher body fat, achieving optimal vitamin D levels often necessitates a more aggressive strategy. This may include significantly higher oral doses, under medical supervision, or considering injectable vitamin D to bypass the sequestration effect and ensure direct delivery into the bloodstream. Furthermore, addressing overall metabolic health and working towards a healthy body composition can naturally improve vitamin D dynamics, allowing the body to utilize this vital nutrient more efficiently.
Read more about: Beyond Instinct: 15 Cutting-Edge Vehicles for 2025 Designed to Shield You from Common Driving Pitfalls and Enhance Your Safety

8. **The Influence of Chronic Stress**In our fast-paced world, chronic stress has become an pervasive factor, silently undermining numerous bodily functions, including nutrient metabolism and vitamin D efficacy. When the body is subjected to prolonged periods of stress, it triggers a cascade of physiological responses, primarily involving the hypothalamic-pituitary-adrenal (HPA) axis, leading to elevated levels of stress hormones, most notably cortisol. This sustained state of physiological alert can profoundly interfere with the body’s ability to absorb, process, and utilize vitamin D.
Elevated cortisol, a hallmark of chronic stress, can directly impact vitamin D pathways. It can influence liver enzymes responsible for converting vitamin D into its usable form (25-hydroxyvitamin D) and may also deplete crucial cofactors, such as magnesium, that are essential for vitamin D activation. Beyond direct interference, chronic stress often exacerbates systemic inflammation and contributes to gut dysbiosis, both of which are established “absorption killers.” This creates a detrimental feedback loop where stress impairs vitamin D, and vitamin D deficiency can, in turn, worsen stress-related symptoms like fatigue, low energy, and mood swings or depression.
Moreover, chronic stress diverts the body’s resources. When the body is in a constant ‘fight or flight’ mode, energy and metabolic processes are prioritized for immediate survival rather than for long-term health maintenance, such as efficient digestion and nutrient absorption. This means that even if a vitamin D supplement is ingested, the body’s compromised state due to stress can hinder its effective uptake and subsequent utilization. The intimate link between stress, mood, and vitamin D levels underscores the multifaceted nature of this nutrient’s importance.
Addressing chronic stress is, therefore, an indispensable part of any comprehensive plan to optimize vitamin D levels. Incorporating stress-reduction techniques—such as mindfulness, regular exercise, adequate sleep, and seeking psychological support—can significantly improve overall physiological resilience. By mitigating the impact of chronic stress, you create a more favorable internal environment for your body to absorb and effectively utilize vitamin D, thereby enhancing its broad health benefits, from immune defense to hormone balance and improved mental health.
Read more about: Future-Proofing Your Career by 2030: 12 Essential Strategies for Professionals in an AI-Driven World
9. **Environmental Toxin Exposure**Our daily lives expose us to a multitude of environmental toxins, from pollutants in the air and water to chemicals in food and household products. While often unseen, the cumulative burden of these toxins can place immense stress on the body’s detoxification systems, particularly the liver and kidneys. These two organs are absolutely critical for the metabolism and activation of vitamin D, and their compromised function due to toxin exposure can significantly prevent vitamin D efficacy.
The liver is responsible for the first hydroxylation step, converting vitamin D into 25-hydroxyvitamin D (25(OH)D), the primary circulating form measured in blood tests. The kidneys then perform the second hydroxylation, transforming 25(OH)D into the biologically active hormone, 1,25-dihydroxyvitamin D. When these organs are overwhelmed by environmental toxins, their metabolic efficiency can decline, directly impairing the crucial conversion processes necessary for vitamin D to become usable. This means even if you’re taking your supplement, your body might not be able to effectively turn it into the form it needs.
Furthermore, chronic toxin exposure often triggers and sustains systemic inflammation, a powerful inhibitor of vitamin D absorption and signaling, as we’ve explored. Toxins can also disrupt the delicate balance of the gut microbiome, contributing to increased intestinal permeability, or ‘leaky gut,’ which further compromises the absorption of fat-soluble vitamins like D. This creates a complex web of interactions where environmental factors not only directly impair vitamin D metabolism but also exacerbate other underlying absorption issues.
Supporting the body’s detoxification pathways and minimizing exposure to environmental toxins are essential strategies for improving vitamin D utilization. This includes consuming a nutrient-dense diet rich in antioxidants, staying well-hydrated, and considering practices that reduce overall toxin load. By reducing the burden on your liver and kidneys and supporting healthy detoxification, you create a cleaner, more efficient internal environment, allowing your body to process and activate vitamin D more effectively, ultimately unlocking its full health potential.
**The Bottom Line: A Personalized Path to Optimal Vitamin D**
It’s clear now that achieving optimal vitamin D levels is far more nuanced than simply taking a pill. We’ve journeyed through the intricate landscape of genetic predispositions, chronic inflammation, gut health impairments, specific autoimmune responses, the dynamics of fat cell storage, the pervasive influence of chronic stress, and the subtle yet significant impact of environmental toxin exposure. Each of these factors can act as a formidable barrier, explaining why so many individuals remain deficient despite their best efforts with supplementation.
Your body’s unique biochemistry, lifestyle, and environmental interactions all play a pivotal role in how effectively you absorb and utilize this vital hormone-like nutrient. The path to truly optimizing your vitamin D isn’t a ‘one-size-fits-all’ solution; it’s a personalized expedition into your own physiological landscape. This is where the true power of targeted wellness emerges, moving beyond generalized advice to solutions tailored precisely for you.
Read more about: Sandra Bullock’s Ageless Radiance: Unveiling the Skincare Secrets That Keep Her Forever Young
Stop guessing and start uncovering the real ‘why’ behind your vitamin D dilemma. By embracing a comprehensive approach that includes thorough testing, addressing underlying health issues, and exploring advanced options like injectable vitamin D or personalized nutrient protocols, you can finally move towards vibrant health. This journey, ideally guided by a functional wellness provider, empowers you to take control, understand your body’s specific needs, and build a foundation for lasting well-being. It’s time to unlock the full potential of your vitamin D and experience the profound benefits it offers for your immune system, mood, bones, and overall vitality.