
Your liver is an unsung hero, a powerhouse organ tirelessly working behind the scenes to keep you healthy. It meticulously cleans your blood, plays a crucial role in digesting the food you eat, and performs countless other functions essential for your well-being. But imagine if the very medications you take to feel better could inadvertently put this vital organ at risk.
This concerning phenomenon is known as drug-induced liver injury (DILI), a condition where medications cause harm to the liver. While the vast majority of drugs are perfectly safe when used as directed, it’s crucial to understand that certain common medications can, in some instances, make your liver sick. As Udoka Ikezuagu, M.D., a hospitalist at Loma Linda University Medical Center in Murrieta, California, explains, “While most medications are safe when taken as directed, older adults can be more sensitive to these risks, so it’s important to be aware and bring any concerns to your healthcare provider.”
The stakes are even higher for older individuals, who often juggle multiple prescriptions. A Lown Institute report revealed that roughly 40 percent of people aged 65 and older regularly take five or more prescription drugs. This increased medication load can escalate the risk of stress and potential damage to the liver. Understanding these risks is the first step towards empowering yourself with the knowledge to protect your liver. Let’s explore some of these common medications and discover practical ways to lower your risk of injury.

1. **Acetaminophen (Tylenol)**Acetaminophen stands out as a ubiquitous over-the-counter (OTC) medication, a go-to for many seeking relief from mild to moderate pain or aiming to reduce a fever. Its widespread availability and effectiveness make it a staple in medicine cabinets around the world, known by common names like Tylenol in the United States and Paracetamol internationally. Its accessibility, however, also contributes to its potential risks, as users might not always recognize the fine line between therapeutic use and potential harm.
While acetaminophen is generally considered safe when dosage instructions are diligently followed, the ease with which one can exceed the recommended amount is a significant concern. This is largely due to its presence in numerous combination medications, particularly popular cold and flu remedies. Without careful label reading, it’s all too easy to unintentionally consume too much acetaminophen across different products, putting undue stress on your liver and potentially leading to harm.
The risk of liver injury from acetaminophen is further amplified under certain conditions. Individuals who regularly consume alcohol, or those with a pre-existing history of liver problems, face a higher susceptibility to adverse effects. This highlights the importance of a comprehensive understanding of your personal health profile and medication intake, extending beyond just single-drug products to encompass all remedies you might be using concurrently.
To proactively safeguard your liver when using acetaminophen, always adhere strictly to the label’s directions and never exceed the recommended dose. The manufacturer typically sets the daily dose limit at 3,250 milligrams (mg) for adults, though some healthcare providers may permit up to 4,000 mg per day under specific guidance. Crucially, cultivate the habit of meticulously reading the ingredients list on all OTC medications to identify hidden acetaminophen. Before initiating acetaminophen, especially if you drink alcohol or have known liver issues, a conversation with your healthcare provider or pharmacist is an essential protective step.
Read more about: The Ultimate Road Trip Safety Playbook: 12 Non-Negotiable Rules to Keep Your Journey Smooth and Secure for Every Driver
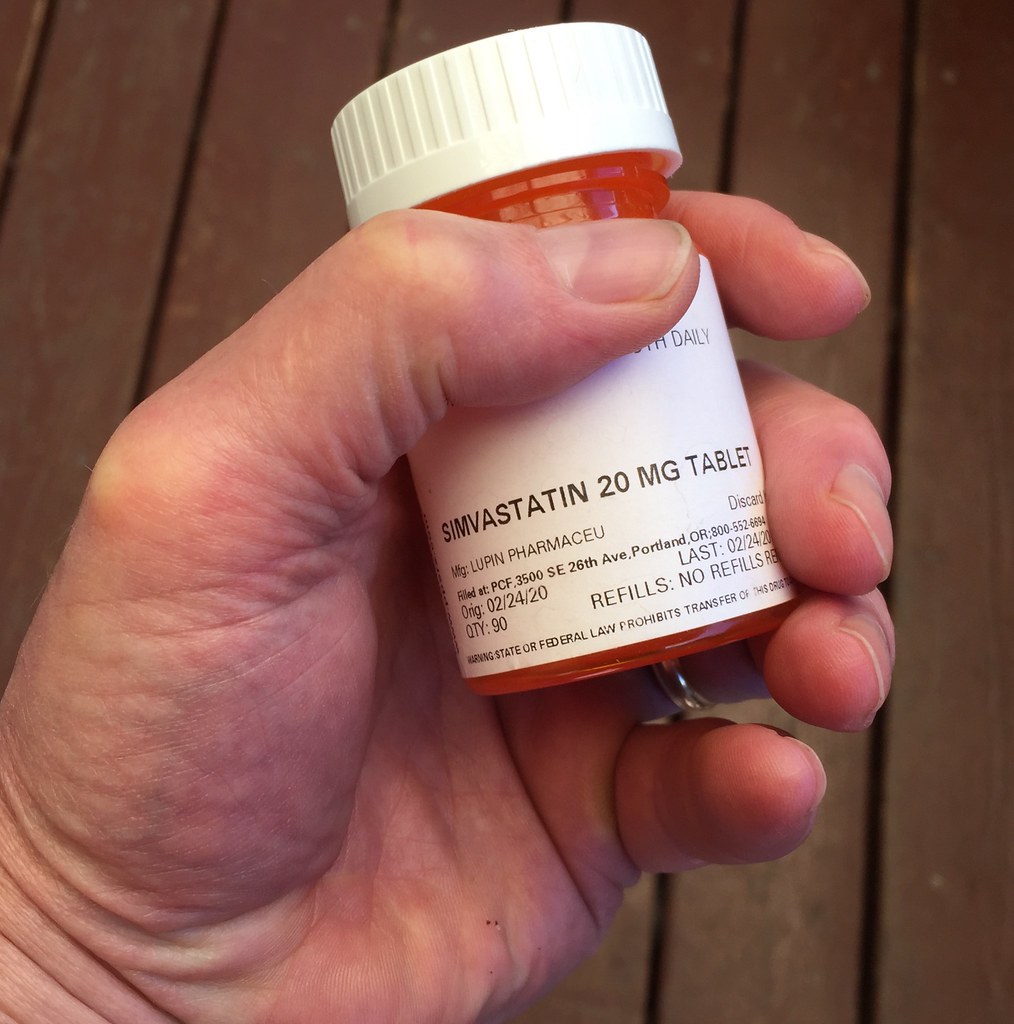
2. **Statins (e.g., Atorvastatin, Simvastatin)**Statins are a class of prescription medications widely prescribed for their remarkable ability to lower cholesterol levels and, consequently, reduce the risk of heart disease. These drugs, known by common names such as atorvastatin (Lipitor), simvastatin (Zocor), and rosuvastatin (Crestor), play a critical role in cardiovascular health management for millions worldwide. Their effectiveness in preventing serious cardiac events has made them a cornerstone of modern medicine, but like all powerful medications, they come with a profile of potential side effects.
While statins are generally considered safe and well tolerated by most patients, they do have a known interaction with liver function. One of the more common effects observed is an elevation in liver enzymes, particularly alanine aminotransferase (ALT). This increase often signals that the liver is working harder, though increases less than three times the upper limit of normal may not necessarily prompt your doctor to discontinue statin use. Encouragingly, these enzyme levels typically return to normal once the medication is stopped, indicating that for many, the effect is reversible.
It is in rare instances that statins can lead to more serious liver problems, a risk that becomes particularly pertinent if an individual already has pre-existing liver issues. This emphasizes the need for personalized medical assessment and ongoing monitoring, ensuring that the benefits of cholesterol reduction continue to outweigh any potential hepatic risks. The key lies in careful management and communication between patient and healthcare provider.
To mitigate the risk of liver injury while taking statins, your healthcare provider may recommend periodic blood tests to monitor your liver function. It’s important to note that not everyone on statins requires these tests, but they serve as a valuable tool for early detection if concerns arise. Common blood tests to check liver function include AST (aspartate aminotransferase), ALT (alanine aminotransferase), ALP (alkaline phosphatase), and Bilirubin, each with established normal ranges that guide clinical assessment.

3. **Amoxicillin-clavulanate (Augmentin)**Amoxicillin-clavulanate, an antibiotic commonly recognized by its brand name Augmentin, is a potent medication used to combat a wide array of bacterial infections. It combines amoxicillin, a penicillin-type antibiotic, with clavulanate, which helps prevent antibiotic resistance. This combination makes it a highly effective treatment for many common infections, yet its efficacy comes with a notable consideration regarding its impact on liver health, making it a critical drug for patient and clinician awareness.
This antibiotic can, in certain circumstances, cause harm to the liver. While the precise mechanism behind this effect isn’t fully understood, research points towards an allergic reaction primarily triggered by the clavulanate component of the medication. What makes amoxicillin-clavulanate-induced liver problems particularly insidious is their potential for delayed onset; liver issues can surface anywhere from a few days to several weeks after beginning the course of medicine, or even after the treatment has been completed. The likelihood of such complications further escalates with prolonged use and for individuals who already have existing liver problems.
Amoxicillin-clavulanate holds a significant, albeit concerning, distinction in the realm of drug-induced liver injury. It is frequently implicated as the most common agent leading to DILI in prospective studies, suggesting its widespread impact. A recent prospective study revealed that liver injury attributable to amoxicillin-clavulanate occurred in approximately one out of every 2300 users. This statistic underscores the importance of vigilance and patient education regarding its potential side effects.
Given its known potential for liver injury, it’s paramount to be alert for specific symptoms that could indicate a problem. Watch out for yellowing of the skin or eyes (jaundice), unusual tiredness, or dark-colored urine. Should you notice any of these signs, prompt contact with your healthcare provider is absolutely essential. Open communication about your symptoms can facilitate early diagnosis and intervention, which is critical for managing this type of adverse reaction effectively.

4. **Flucloxacillin**Flucloxacillin is a well-established antibiotic, often prescribed for its effectiveness against a range of bacterial infections. As an antimicrobial, it belongs to a class of drugs that have consistently been identified in various studies as common culprits in drug-induced liver injury (DILI). Its presence in the broader landscape of medications underscores the necessity for patients and healthcare providers to understand its potential hepatic implications, despite its therapeutic benefits in combating infections.
This medication is specifically listed in analyses of LiverTox data as a Category A drug, meaning it has been associated with more than 100 published case reports of liver injury. This substantial number of documented cases places flucloxacillin among drugs with a significant and undeniable potential for hepatotoxicity. The medical literature further reinforces this, noting that flucloxacillin is one of the ten most frequently implicated drugs in several DILI registries, highlighting its consistent association with liver adverse events across different populations.
The mechanism of liver injury from antibiotics like flucloxacillin can vary, but the consistent reporting of DILI cases points to a clear risk that cannot be overlooked. The widespread use of antibiotics contributes to their frequent appearance in DILI statistics, emphasizing that while they are vital for treating infections, they are not without their potential challenges to organ health. Clinicians are often advised to be aware of these risks when prescribing and monitoring patients.
To help protect your liver when prescribed flucloxacillin, proactive measures are key. It is vital to discuss any history of liver problems with your doctor and adhere strictly to the prescribed dosage and duration of treatment. Being aware of the signs of potential liver distress, such as unexplained fatigue, nausea, vomiting, or changes in urine color or skin complexion, is crucial. If any such symptoms emerge, immediate consultation with your healthcare provider is necessary to assess liver function and determine the appropriate course of action, ensuring your well-being remains the top priority.

5. **Erythromycin**Erythromycin is another significant antimicrobial, part of a family of antibiotics widely used to treat bacterial infections in patients who may have allergies to other antibiotics or for specific types of infections. Like flucloxacillin, it is listed as a Category A drug in analyses based on LiverTox data, indicating its association with more than 100 published cases of drug-induced liver injury. This positions erythromycin as a medication with a well-documented history of potential hepatotoxicity, making it a focus point for discussions on medication safety.
Antimicrobials, as a class, are frequently cited as leading causes of DILI across numerous prospective and retrospective studies. The data shows that antimicrobials constituted a substantial percentage of DILI cases, dominating not only Category A drugs but also being common agents in Categories B, C, and D. Erythromycin’s inclusion among the ten most frequently implicated drugs further solidifies its status as a drug that healthcare providers and patients should approach with informed caution regarding liver health.
The potential for erythromycin to cause liver injury is a recognized aspect of its pharmacological profile. While it serves as a valuable tool in treating infections, its hepatic effects necessitate careful consideration, particularly in individuals who might be more susceptible to liver dysfunction. The widespread use of such effective antibiotics means that even a low incidence rate of DILI can translate into a significant number of affected individuals, underscoring the importance of vigilance.
For those prescribed erythromycin, taking steps to protect your liver is a sensible approach. Ensure your healthcare provider is fully informed about your medical history, including any prior liver conditions or current medications you are taking, to allow for a comprehensive risk assessment. Pay close attention to your body for any unusual symptoms that could signal liver distress, such as persistent nausea, abdominal pain, dark urine, or yellowing of the skin or eyes. Promptly reporting these symptoms to your doctor ensures that any potential liver issues can be investigated and managed without delay.
Read more about: The Pharmaceutical Odyssey: Two Centuries of Innovation, Impact, and Unfolding Challenges

6. **Diclofenac**Diclofenac is a commonly prescribed nonsteroidal anti-inflammatory drug (NSAID), widely used to alleviate pain, reduce inflammation, and manage fever. Its efficacy makes it a popular choice for conditions ranging from arthritis to acute injuries, providing much-needed relief to countless individuals. However, despite its beneficial effects, diclofenac is also recognized for its potential impact on liver health, making it an important consideration in the broader discussion of drug-induced liver injury (DILI).
This NSAID is listed as a Category A drug in comprehensive analyses of data from LiverTox, signifying that it has been associated with more than 100 published case reports of liver injury. This places diclofenac squarely among medications known to carry a notable risk of hepatotoxicity. Furthermore, it holds the distinction of being the only drug, apart from antibiotics, to appear among the top ten implicated drugs in the DILIN registry, an important US study on DILI.
The potential for NSAIDs like diclofenac to cause liver injury highlights that DILI is not solely a concern for antibiotics. While many people associate NSAIDs with gastrointestinal side effects, their systemic effects can extend to the liver. The consistent reporting of diclofenac in DILI studies across different countries, including its mention in Spanish, DILIN, and Icelandic prospective studies, underscores its established role as a potential hepatotoxin that requires careful monitoring.
When using diclofenac, it is prudent to be proactive about liver protection. Always adhere to the lowest effective dose for the shortest possible duration, as advised by your healthcare provider, to minimize potential risks. It’s also crucial to avoid combining it with other medications that could similarly stress the liver without medical supervision. Vigilance for symptoms such as jaundice, unexplained fatigue, dark urine, or persistent nausea is important, and any such signs should prompt an immediate discussion with your doctor to ensure your liver health is properly assessed and managed.
We’ve journeyed through the crucial functions of your liver and explored how some commonly used medications can surprisingly pose a risk to its health. From the everyday pain reliever acetaminophen to the vital statins and various antibiotics, understanding these potential impacts is key to proactive health management. Now, let’s continue our deep dive into more medications and broader drug categories that warrant your attention, shedding light on their liver effects and empowering you with practical strategies to protect this indispensable organ.
Read more about: India: A Rising Global Power and Its Complex Path Forward

7. **Isoniazid**Isoniazid is a cornerstone medication in the fight against tuberculosis, a serious bacterial infection. Its efficacy in treating and preventing this disease has made it an indispensable tool in global health. However, despite its vital role, isoniazid is well-recognized in medical literature for its potential to cause drug-induced liver injury, a side effect that necessitates careful monitoring during treatment.
This antituberculosis agent has a documented history of hepatotoxicity, frequently appearing in studies as a significant cause of DILI. Research, including prospective studies from Spain and the DILIN cohort in the US, consistently lists isoniazid among the top implicated drugs. It’s known to predominantly induce a hepatocellular pattern of liver injury, meaning it directly affects the liver cells themselves, leading to inflammation and potential damage.
The risk of liver injury with isoniazid is notable, with some studies indicating a risk greater than 100 per 100,000 users. This elevated risk underscores why healthcare providers must engage in thorough patient counseling. As one of the drugs with a known clinical signature of liver injury, discussions with your doctor about potential symptoms and the importance of prompt discontinuation if these symptoms arise are paramount.
To safeguard your liver while taking isoniazid, strict adherence to your doctor’s instructions is critical, and any changes in your health should be reported immediately. Watch for signs like unusual fatigue, nausea, vomiting, dark urine, or yellowing of the skin or eyes. Regular liver function tests will likely be part of your treatment plan, allowing your healthcare provider to monitor your liver’s health and make any necessary adjustments swiftly.
8. **Sulfamethoxazole/Trimethoprim (Bactrim)**Sulfamethoxazole/Trimethoprim, often known by the brand name Bactrim, is a powerful combination antibiotic used to treat a wide range of bacterial infections, including urinary tract infections (UTIs), bronchitis, and certain types of pneumonia. This dual-action medication effectively targets bacteria by disrupting their folate metabolism, making it a valuable tool in infectious disease management.
As a sulfonamide antibiotic, Sulfamethoxazole/Trimethoprim falls into a class of drugs frequently implicated in DILI. It consistently ranks among the top 10 most frequently cited drugs causing liver injury in various registries and studies, including the DILIN cohort where antimicrobials constituted approximately 46% of all DILI cases. While generally effective, its broad use and chemical structure contribute to its potential for hepatic side effects.
The mechanism of liver injury from Sulfamethoxazole/Trimethoprim is not always fully understood, but it can manifest in various ways, ranging from mild enzyme elevations to more severe liver dysfunction. Patients with a known sulfa allergy should strictly avoid this medication due to the heightened risk of adverse reactions, which can include liver complications. It’s crucial to discuss any allergies with your doctor or pharmacist before starting treatment.
To protect your liver while on Sulfamethoxazole/Trimethoprim, be vigilant for any unusual symptoms. These include the characteristic yellowing of the skin or eyes (jaundice), persistent tiredness, or the appearance of dark-colored urine. Should you observe any of these warning signs, it is essential to contact your healthcare provider without delay. Prompt communication ensures that any liver issues can be identified and addressed quickly, optimizing your treatment outcome and safety.

9. **Nitrofurantoin (Macrobid)**Nitrofurantoin, commonly prescribed under brand names like Macrobid or Macrodantin, is an antibiotic specifically favored for its effectiveness in treating and preventing urinary tract infections (UTIs). It belongs to the nitrofuran class of antibiotics and works by targeting bacterial processes within the urinary tract, making it a focused and often preferred choice for these common infections.
Despite its targeted action and widespread use for UTIs, nitrofurantoin is another medication that has been implicated in drug-induced liver injury. Its presence in DILI registries, including the DILIN and Icelandic prospective studies, underscores its potential to affect liver health. While not as frequently cited as some other antibiotics for severe DILI, its consistent appearance in these studies indicates a recognized risk that warrants awareness.
The liver injury associated with nitrofurantoin can vary, presenting as acute hepatitis, cholestasis, or a mix of both. In some cases, chronic active hepatitis or cirrhosis can occur, especially with prolonged use. This highlights the importance of using the medication strictly as prescribed by your doctor and not for longer durations than necessary, particularly for patients with recurrent infections.
To minimize the risk of liver complications when taking nitrofurantoin, it’s vital to inform your doctor about your complete medical history, especially any pre-existing liver conditions. During your course of treatment, be attentive to your body and report any signs of liver distress such as unusual fatigue, nausea, abdominal pain, loss of appetite, dark urine, or yellowing of the skin or eyes. Your doctor can then conduct appropriate tests and guide you on the best course of action to protect your liver health.

10. **Ibuprofen**Ibuprofen is a widely recognized nonsteroidal anti-inflammatory drug (NSAID) available over-the-counter and by prescription, used extensively for pain relief, fever reduction, and to lessen inflammation from various conditions like arthritis or injuries. Its efficacy and accessibility make it a staple in medicine cabinets globally, offering quick relief for common ailments.
While generally considered safe when taken as directed, Ibuprofen, like other NSAIDs, carries a recognized potential for drug-induced liver injury. It appears in several lists of frequently implicated drugs, including the Spanish prospective study on DILI, alongside other NSAIDs like diclofenac which are explicitly noted for their hepatotoxic risk. Although less common than other side effects, liver injury from Ibuprofen is a documented concern that patients and healthcare providers should be mindful of.
The mechanism by which NSAIDs like Ibuprofen can cause liver damage is complex, but it can lead to various forms of injury, including dose-dependent effects or idiosyncratic reactions that are unpredictable. This underscores the importance of adhering to recommended dosages and avoiding prolonged use, especially when using higher strengths or combining it with other medications that also metabolize through the liver.
To protect your liver when using Ibuprofen, always follow the dosage instructions on the label and never exceed the maximum recommended daily amount. Opt for the lowest effective dose for the shortest possible duration to achieve symptom relief, which minimizes the overall exposure and potential strain on your liver. It’s also crucial to avoid combining Ibuprofen with other NSAIDs or other medications that could further stress the liver, unless specifically advised by a healthcare professional. If you experience persistent nausea, unexplained fatigue, dark urine, or yellowing of the skin or eyes, contact your doctor promptly.
Read more about: Unlock the Open Road: 12 Genius Ways to Double Your Car’s Cargo Space for Any Road Trip
11. **Azathioprine/6-Mercaptopurine**Azathioprine and its active metabolite, 6-Mercaptopurine, are potent immunosuppressive agents primarily used in the management of autoimmune diseases like Crohn’s disease, ulcerative colitis, lupus, and in preventing organ rejection after transplantation. These medications work by suppressing the immune system, which helps to control chronic inflammation and prevent the body from attacking its own tissues or transplanted organs.
Despite their critical therapeutic benefits, Azathioprine and 6-Mercaptopurine are well-known for their significant potential to cause drug-induced liver injury. In some studies, these drugs have been identified as having the highest risk of DILI among all medications. Both hepatocellular and cholestatic patterns of liver injury have been described, indicating a broad impact on liver cell function and bile flow. This makes them a particular concern for patients and clinicians alike.
The incidence rates of liver injury with Azathioprine are notably high, with one study from Iceland reporting DILI in one of every 133 users. Similarly, earlier retrospective studies using the General Practitioners Research Database found crude incidence rates of one per 1103 users. These statistics highlight a substantial and consistent risk, prompting medical professionals to maintain a high degree of vigilance.
Given the high risk of hepatotoxicity associated with Azathioprine/6-Mercaptopurine, close and continuous monitoring of liver function is absolutely essential throughout the course of treatment. Your healthcare provider will likely schedule regular blood tests to check liver enzyme levels and overall liver health. It is paramount to report any symptoms such as persistent fatigue, unexplained nausea, abdominal pain, dark urine, or jaundice immediately. Early detection and prompt intervention are key to managing any potential liver issues and ensuring the safest possible treatment outcome.

12. **Phenytoin**Phenytoin is an established antiepileptic drug, widely used to control and prevent various types of seizures, particularly tonic-clonic (grand mal) seizures and complex partial seizures. It works by stabilizing electrical activity in the brain, making it a crucial medication for individuals living with epilepsy. Its long history of use provides a wealth of clinical data, including insights into its potential side effects.
As an antiepileptic agent, Phenytoin belongs to a class of drugs that are frequently identified as causes of drug-induced liver injury. Antiepileptics have been noted in various DILI studies, including those from India and the General Practitioners Research Database, as significant contributors to liver adverse events. While DILI from Phenytoin is considered an idiosyncratic reaction, meaning it occurs unpredictably in susceptible individuals, its serious nature mandates awareness.
Liver injury associated with Phenytoin can manifest in different ways, ranging from mild liver enzyme elevations to more severe and sometimes life-threatening reactions like hypersensitivity syndrome, which can involve liver damage. The onset of DILI with Phenytoin can sometimes be delayed, occurring days or weeks after starting the medication, emphasizing the need for ongoing vigilance.
For patients prescribed Phenytoin, open communication with your healthcare provider is paramount. Ensure your doctor is fully aware of your medical history, especially any previous liver problems or other medications you are taking. Adhere strictly to the prescribed dosage and do not make any adjustments without medical consultation. Be alert for any symptoms that could indicate liver distress, such as jaundice, unexplained itching, dark urine, pale stools, persistent nausea, or unusual tiredness, and report them to your doctor immediately for prompt evaluation and management.
As we conclude our comprehensive look at common medications and their potential impact on liver health, it’s clear that vigilance and informed communication with your healthcare providers are your strongest allies. Understanding these risks empowers you to be an active participant in your health journey, ensuring that your liver, your body’s tireless detoxifier, remains robust. And the good news is, research continues to forge ahead, offering new hope. Scientists at the University of Barcelona, for instance, have recently unveiled promising findings in *Pharmacological Research* about two existing cardiovascular drugs, pemafibrate and telmisartan, which when used together, showed significant potential in reversing fat accumulation in animal models of metabolic liver disease. This exciting drug repurposing strategy highlights a future where managing liver health might become even more effective and accessible, offering a beacon of hope for conditions like fatty liver disease, which is rapidly becoming a global health concern. Until then, stay informed, stay proactive, and keep nurturing your liver’s well-being.



