When a loved one is nearing the end of their life, it’s a moment often cloaked in uncertainty and raw emotion. We instinctively want to ease their journey, to be present, and to reassure them with every soothing word and gentle action we can offer. But for many of us, the process of dying remains a mystery, a path uncharted, leaving us feeling helpless or unsure of how best to support someone we cherish.
It’s never easy to witness the subtle, yet profound, shifts that occur as life begins its final transition. The fear of the unknown can be overwhelming, not just for the person who is dying, but for their family and friends who are walking alongside them. Understanding what to expect, recognizing the signs, and knowing how to provide comfort can transform moments of anxiety into opportunities for deeper connection and peace.
In these incredibly tender moments, knowledge truly becomes a source of strength. We’re here to gently guide you through the common signs that indicate death may be near, offering a compassionate look at the changes you might observe in your loved one. This isn’t about clinical detachment; it’s about embracing a fundamental human experience with empathy and preparation, ensuring dignity and comfort prevail.
1. **The Fading Appetite: A Natural Shift**: One of the most common and often distressing changes you might notice is a significant decrease in appetite. As a person approaches death, their body naturally becomes less active, which simply means it requires much less energy. This beautiful, if heartbreaking, physiological adjustment leads to a gradual reduction in the desire for food and drink, sometimes to the point where they stop eating entirely.
It’s a natural and expected part of the body slowing down, not a sign that your loved one is suffering from hunger or thirst in the way we typically understand it. The most important thing you can do is never to push food or fluids. This can cause discomfort, choking, or even gastrointestinal pain. Instead, focus on providing comfort.
Keeping their mouth and lips moist with damp sponges or offering sips of liquid if they desire and are able to swallow can provide immense relief. Applying lip balm can prevent chapping and keep them comfortable. Remember, this decrease in appetite is their body’s way of preparing, and your role is to honor that process with gentle care.
2. **The Gentle Embrace of Sleep: Increased Drowsiness**: As the body conserves energy, you’ll likely notice your loved one spending much more time asleep or in a drowsy state. They may appear sleepy even when awake, or they might lose consciousness for periods ranging from a little while to several days. This increased sleep is caused in part by changes in the patient’s metabolism and a decreased need for energy.
It’s crucial to make them as comfortable as possible during these prolonged periods of rest. Gentle turning and repositioning every one to two hours can ease muscle stiffness and prevent pressure injuries to the skin. Creating a soothing and calm environment by dimming lights and perhaps playing soft music they enjoy can also be incredibly comforting.
Even if they seem detached or unresponsive, it’s vital to continue speaking to them gently and soothingly. Hearing is often the very last sense a person loses before death, so your calm, quiet voice can provide immense reassurance and a sense of your comforting presence, even if they cannot respond. They may still be able to hear you, and your words matter.
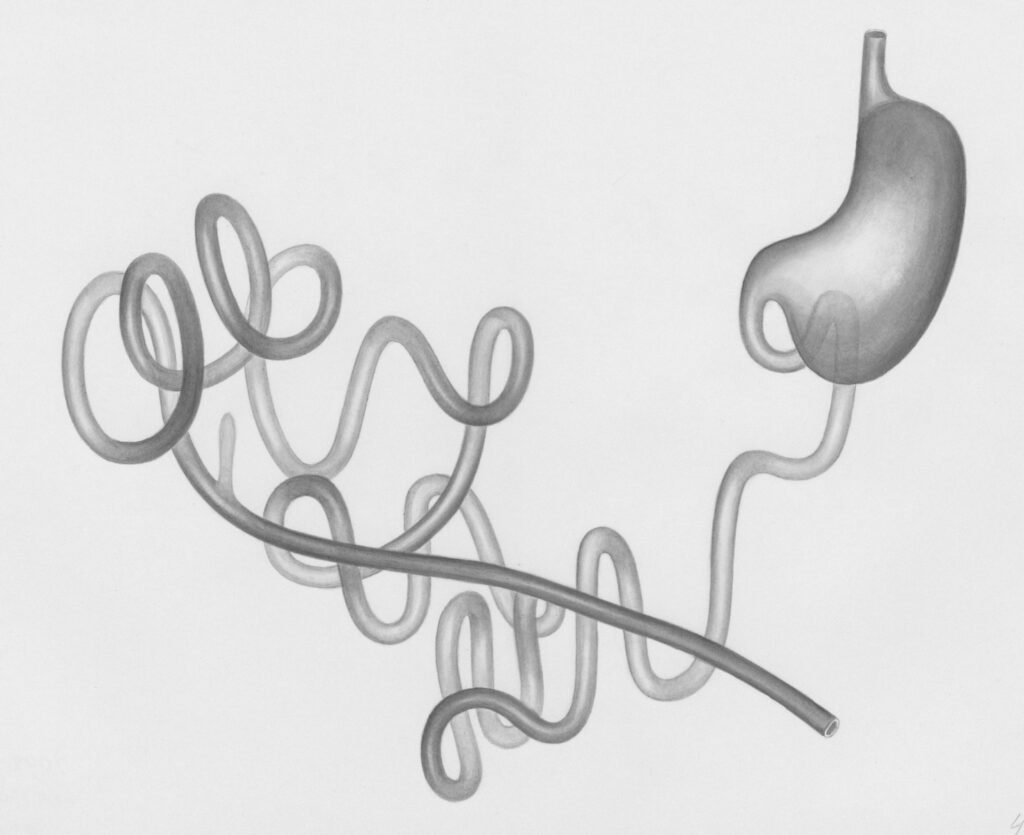
3. **Navigating Changing Habits: Bowel and Bladder Shifts**: Because a dying person is eating and drinking less, their body’s waste elimination processes also slow down. You might observe that their bowel movements become less frequent and smaller, and they may urinate less often. Their urine might also appear darker. In some cases, a person may lose control of their bladder and bowels, which is a normal and expected part of the dying process as muscles in the pelvic area relax.
While these changes can be distressing to witness, it’s important to understand that they are a natural part of the body shutting down. If incontinence becomes an issue, incontinence pads or a catheter can be used to maintain comfort and hygiene. A catheter, when properly in place, is painless and helps protect their skin while minimizing the need for frequent repositioning for diaper changes.
If constipation becomes evident, stool softeners or laxatives may be needed to maintain comfort, and your hospice or healthcare team can advise on this. These aren’t just practical steps; they’re acts of care that preserve your loved one’s dignity and ensure their comfort during a vulnerable time.

4. **The Softening Grip: Weakening Muscles and Movement**: In the days leading up to death, your loved one’s muscles may become noticeably weak. This means that tasks they could previously manage, like drinking from a cup, lifting objects, or even turning over in bed, may become impossible for them to do on their own. This weakening is a direct result of their body conserving energy and a decrease in circulation.
Your role here shifts to one of gentle assistance. Be prepared to help them with what were once simple, everyday movements. Offering support when they need to adjust their position, helping them take sips of water with a straw or teaspoon, or gently lifting their hand to yours can make a significant difference in their comfort and sense of security.
It’s a powerful way to show your presence and support, ensuring they don’t feel the burden of their weakening body alone. This physical assistance is also a profound emotional comfort, reminding them that they are seen, loved, and cared for in every moment.

5. **The Body’s Shifting Rhythms: Changes in Vital Signs**: As a person approaches death, their vital signs—the fundamental indicators of bodily function—begin to change and become irregular. You may notice their blood pressure dropping, sometimes significantly. Their heartbeat might become fast, faint, or irregular, and their pulse may become difficult to detect. These fluctuations or gradual decreases are expected as the body’s systems slow down.
While these changes can be alarming to witness, they are a natural progression as the body prepares for its final rest. It’s important to report these observations to the hospice nurse or other healthcare provider, as they can offer guidance and ensure comfort measures are in place. These symptoms can appear at any stage of a terminal illness but often become more pronounced in the final days or hours.
Understanding that these shifts are part of the process can help you remain calm and focused on providing loving support. The body is simply adjusting, moving towards a peaceful resolution of its functions, and your presence is the most vital sign of all.

6. **The Cooling Touch: Understanding Body Temperature Changes**: In the days before a person dies, their circulation significantly reduces, as blood flow is concentrated on vital internal organs. This means that very little blood flows to their extremities, such as their hands, feet, and legs, causing them to feel cold to the touch. Their skin may also take on a pale, purplish, or mottled appearance, especially on the knees, feet, or hands, due to this reduced circulation.
While these skin changes can look concerning, often the person who is dying does not feel cold themselves. It’s a visual sign for caregivers, indicating the body’s natural redistribution of blood. If a relative or friend thinks they may need one, offering a soft, warm blanket is a good idea to provide comfort. However, avoid using heating pads on their hands or feet, as fragile skin can burn easily.
Conversely, some individuals may develop a mild fever, and their torso and face might appear flushed and feel warmer. In these instances, a lukewarm washcloth on their forehead can provide some relief. These varying temperature shifts are all part of the body’s internal adjustments.

7. **The Breath’s Evolving Cadence: Altered Breathing Patterns**: As death nears, breathing patterns can become highly irregular and may be one of the most distressing signs for family members to witness. You might notice sudden changes in breath speed, with periods of rapid breathing alternating with slower, more shallow breaths, or even short pauses in breathing. Grunting, gurgling, or rattling noises, often referred to as a “death rattle,” may also occur.
This “death rattle” happens because the body can no longer reabsorb fluids in the throat or chest as well as it used to, leading to a buildup of secretions. While these sounds can be deeply unsettling for caregivers, it’s incredibly important to understand that this often does not indicate pain or suffering for the dying person. It’s usually more bothersome to those who are listening.
You can try to find a position that makes breathing easier for them, such as turning them on their side, elevating their head and shoulders, or having them sit up if possible. The hospice team may also recommend medications that can help manage these secretions. Remember, even with these changes, your presence and soothing actions continue to provide profound comfort.”
Beyond the more immediately observable physical changes, the journey toward life’s end often involves complex shifts in a person’s experience, both internally and in their interactions with the world. These deeper transformations, alongside the profound cultural and spiritual lenses through which we view dying, and the evolving role of modern medical care, help us to embrace this universal passage with greater understanding and compassion.

8. **Increasing Pain: Navigating the Toughest Challenge**: It can be incredibly difficult to come to terms with the fact that, as a loved one nears death, the treatment they once received may no longer be able to fully manage their pain levels. Witnessing a pained expression, hearing a groan, or even just sensing their discomfort is never easy, and the pain itself may increase as their underlying disease progresses, or as chronic conditions like arthritis worsen, or if new pressure injuries develop on fragile skin. This is a profound challenge for everyone involved.
Your role as a caregiver here is vital. Even if your loved one is non-verbal, there are often subtle signs of discomfort: agitation or restlessness, moaning or groaning, stiffening their body to resist movement, grimacing, or clenching their fists or teeth. It’s crucial to be attuned to these signals and communicate them promptly to the hospice team. They are equipped to discuss pain management strategies, possibly adjusting medication schedules or adding new pain relief to ensure comfort and dignity during these tender moments.

9. **The Quiet Withdrawal: Becoming Less Social**: As a person’s energy levels begin to dwindle, a natural and often deeply emotional shift occurs: they may start to withdraw, bit by bit, from the life around them. This process, sometimes described as “detaching,” means your loved one may not respond to questions as readily, show less interest in activities they once cherished, or interact less with family, caregivers, and friends. It’s a profound slowing down, an internal preparation for what’s to come.
While these changes can feel like a personal rejection or be deeply upsetting, it’s so important for loved ones not to be offended. This withdrawal is a natural part of the dying process, caused by decreased oxygen to the brain, reduced blood flow, and a mental preparation for their final journey. Continue to act as if your loved one can hear you and is aware of what is going on, as hearing is often the very last sense to lapse before death. Keeping the environment calm and peaceful, perhaps with dim lights or soft music, and arranging visits when the person is truly up to seeing someone can provide immense comfort without overwhelming them.
As we gently close this conversation, it’s clear that the journey towards death is as unique and individual as life itself, yet it is also marked by universal signs and profound shared human experiences. From the subtle shifts in the body’s functions to the complex dance of cultural rituals and personal reflections, understanding what to expect can transform moments of fear into opportunities for deeper connection and peace. It’s about being present, offering comfort, and ensuring that every soothing word and gentle action reaffirms the dignity and love we hold for those who are embarking on their final transition. In these tender moments, your compassionate presence truly is the most vital sign of all.