In an era defined by profound environmental shifts and unprecedented demographic changes, two urgent global concerns—climate change and rapid population aging—are converging to create a complex web of challenges for communities and public policies worldwide. The average human lifespan has seen remarkable extensions, a testament to advancements in nutrition, technology, and medicine. This triumph of modern society, coupled with declining birth rates, has led to a significant increase in the population of individuals aged 65 years or older.
Indeed, projections indicate a monumental shift: from approximately 703 million older adults globally in 2019, this demographic is expected to swell to 1.5 billion by 2050, representing an increase from 9% to 16% of the world’s population. As individuals age, however, they naturally experience physical and mental declines, rendering them more susceptible to external stressors such as extreme temperatures and pervasive air pollution. This heightened vulnerability places older adults at the forefront of climate change’s adverse health consequences.
Recognizing this critical intersection, a recent systematic review embarked on a vital mission: to meticulously gather and analyze quantifiable health indicators that illuminate the intricate connection between climate change and the physical and mental well-being of the older population. This in-depth investigation synthesized findings from nineteen rigorous studies conducted between 2015 and 2022, offering a sobering, yet crucial, panoramic view of how a hotter, more volatile world is subtly, and sometimes overtly, accelerating the aging process and exacerbating health vulnerabilities for our eldest generations. Join us as we explore the specific and often alarming ways climate phenomena are impacting older adults.

1. **Extreme Heat and Renal, Respiratory, and Heat-Related Hospitalizations**The relentless increase in global temperatures manifests acutely through extreme heat events, which pose a significant and immediate threat to the health of older adults. These periods of intense warmth push the human body’s thermoregulatory systems to their limits, particularly in an aging population whose natural ability to adapt to temperature fluctuations may be diminished. The consequences can be severe, leading to a surge in hospitalizations for a range of heat-related, renal, and respiratory conditions.
A compelling case-crossover study conducted in the USA between 1992 and 2006 meticulously examined the impact of extreme heat, revealing a clear and troubling correlation. Researchers found that two-day extreme heat effects were associated with an 8% increase (with a 95% confidence interval of 6–11%) in hospitalizations for renal, heat, and respiratory causes. Extending this period, six-day extreme heat effects correlated with an even higher surge, an 11% increase (95% CI: 8–14%) in these crucial hospital admissions.
Further dissecting the vulnerability across age groups within the older population, the study highlighted that individuals aged 78 years or older faced a significantly elevated risk of renal, heat, or respiratory hospitalizations six days following extreme heat exposure. Their risk increased by 15% (95% CI: 11–19%), a stark contrast to the 7% increase (95% CI: 4–10%) observed in the 65–77 years age group. This differential vulnerability underscores the compounded challenges faced by the oldest among us, as their physiological reserves dwindle and their capacity to cope with environmental stressors is further compromised, making adaptation strategies even more critical.

2. **Smoke Waves from Wildfires and Respiratory Illness Hospitalizations**Beyond direct temperature impacts, climate change fuels other environmental hazards with severe health implications. Wildfires, for instance, are becoming more frequent and intense, releasing vast plumes of smoke into the atmosphere. These ‘smoke waves’ carry fine particulate matter (PM2.5) that can infiltrate deep into the lungs, triggering respiratory illnesses and exacerbating pre-existing conditions, particularly in vulnerable populations like older adults.
An ecological study conducted in the USA from 2004 to 2009 shed light on the specific risks posed by these high-pollution episodes resulting from wildfire smoke. The findings revealed a notable increase in hospitalizations for respiratory illnesses, including chronic obstructive pulmonary disease (COPD) and other respiratory tract infections, during smoke-wave days compared to non-smoke-wave days. Interestingly, the study uncovered a gender disparity in these outcomes, with females exhibiting a higher risk of hospital admissions than males, at 10.4% and 3.7% respectively.
The research further elucidated the role of socioeconomic factors in modulating this vulnerability. The relative risk of respiratory admissions on smoke-wave days was found to be notably higher for individuals residing in areas characterized by lower educational attainment (RR = 1.13, 95% CI: 0.97–1.31) when compared to those living in areas with higher educated individuals (RR = 1.06, 95% CI: 0.98–1.14). This suggests that social determinants of health, such as access to information, resources, and potentially better housing or healthcare, play a crucial role in buffering the adverse effects of environmental pollution stemming from climate-driven events.

3. **Drought Periods: Dual Impact on Respiratory Health and Mortality**Droughts, characterized by prolonged periods of insufficient precipitation, represent another significant manifestation of climate change with complex health consequences for older adults. While the immediate effects of heat are often highlighted, droughts can subtly and significantly alter environmental conditions, affecting both physical health and mortality rates. Their impact can be surprising, sometimes leading to unexpected outcomes depending on geographical and historical exposure.
A retrospective cohort study in the USA, spanning from 2000 to 2013, investigated the health effects of full drought periods, defined as lasting 150 days or more. During these extended dry spells, the study observed an intriguing dual impact: respiratory-related hospitalizations actually decreased by -1.99% (95% PI: -3.56, -0.38) compared to non-drought periods. This counter-intuitive finding might be attributed to reduced humidity or a decrease in certain allergens during drought conditions.
However, the same study painted a grimmer picture regarding mortality. It reported that the risk of mortality significantly increased by 1.55% (95% PI: 0.17–2.95) during high-severity worsening drought periods. Crucially, the negative health outcomes were found to be more pronounced in geographic locations that experienced less frequent droughts. This observation suggests a phenomenon of population acclimatization, where communities accustomed to droughts may develop adaptive capacities, while those unaccustomed are disproportionately affected when such events occur, highlighting the importance of regional resilience strategies in a changing climate.

4. **Sea Surface Temperature Variability (ENSO/AMO) and Cardiovascular Health**The vast oceans, through their complex dynamics, exert a profound influence on global climate patterns, and their variability can have far-reaching health implications, even for cardiovascular health in older adults far from the coast. Phenomena like the El Niño-Southern Oscillation (ENSO) and the Atlantic Multidecadal Oscillation (AMO) represent large-scale sea surface temperature (SST) fluctuations that alter weather systems worldwide, consequently affecting human health.
A multi-country ecological study conducted across the USA, Canada, and the UK from 2000 to 2017 meticulously linked SST variability to cardiovascular outcomes. The research indicated that a shift from cool to warm phases of ENSO was associated with a reduction in acute myocardial infarction (AMI) admissions in Canada (adjusted RR 0.89; 95% CI: 0.80–0.99). However, this same shift correlated with an alarming increase in AMI deaths in the USA (RR 1.09; 95% CI: 1.04–1.15), underscoring the geographically varied and often contradictory impacts of these climate drivers.
Similarly, the Atlantic Multidecadal Oscillation (AMO) also showed a significant influence. During its strong positive phase, AMO was linked to reduced AMI admissions in eastern Canada (RR 0.93; 95% CI: 0.87–0.98). Yet, simultaneously, it was associated with an increased risk of ischemic heart disease (IHD) deaths in the UK (RR 1.08; 95% CI: 1.03–1.14). These findings collectively illustrate that large-scale oceanic temperature shifts, though seemingly distant, can profoundly disrupt cardiovascular health in older populations across different continents, pointing to the interconnectedness of global climate systems and local health vulnerabilities.
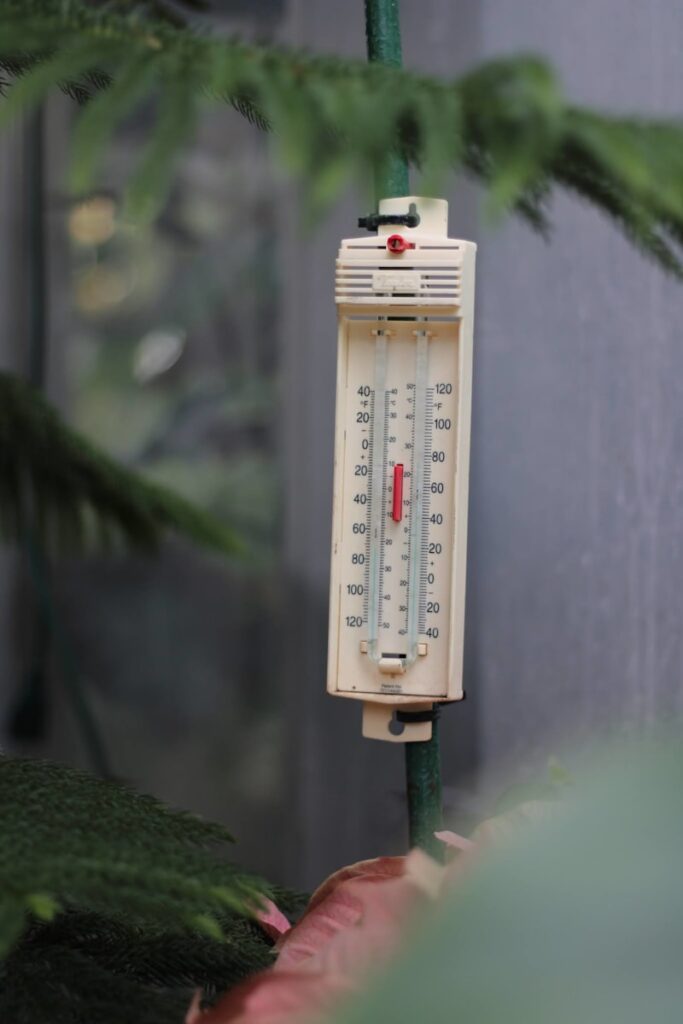
5. **Non-optimum Temperatures (Cold and Heat) and All-cause Mortality**While the focus often leans towards extreme heat in a warming world, the reality for older adults is that any deviation from optimum temperatures, whether excessively hot or cold, can significantly elevate mortality risks. The human body, particularly as it ages, struggles to maintain a stable internal temperature when faced with environmental extremes, leading to physiological stress that can exacerbate existing health conditions or directly contribute to fatal outcomes.
A comprehensive ecological study conducted in Bulgaria between 2000 and 2017 provided striking evidence of this pervasive threat. It reported that a substantial 12.3% (95% CI: 7.3–16.8%) of all deaths during that period were directly attributable to non-optimum temperatures. Delving deeper, the study revealed that moderate cold was the largest contributor to temperature-attributable mortality, accounting for 10.9% (95% CI: 5.8–15.6%) of these deaths.
While moderate heat also contributed (1.1%; 95% CI: 0.5–1.6%), even extreme cold (0.6%; 95% CI: 0.4–0.7%) and extreme heat (0.3%; 95% CI: 0.1–0.4%) presented measurable, though smaller, attributable mortality percentages. This underscores that both ends of the temperature spectrum, including conditions that might not be considered ‘extreme’ by the general public, pose a significant and often underestimated threat to older adults, particularly highlighting the insidious danger of prolonged moderate cold exposure.

6. **Increased Temperature and Acute Psychiatric Hospitalizations**The impact of climate change extends far beyond physical ailments, deeply affecting mental health, particularly in vulnerable populations. As temperatures rise and extreme weather events become more frequent, the psychological burden on older adults can escalate, leading to increased stress, anxiety, and the exacerbation of pre-existing mental health conditions. This invisible toll on the mind is a critical, yet often overlooked, aspect of climate change’s health consequences.
A compelling case-crossover study performed in the USA from 2000 to 2016 meticulously investigated the link between increased temperatures and acute psychiatric hospitalizations. The findings revealed a statistically significant increase in the relative risk of hospitalization for various mental health disorders during periods of elevated temperature, even in the cold season. Specifically, for every 5°C increase in short-term exposure to cold season temperature, the relative risk of hospitalization for depression rose by 3.66% (95% CI: 3.06–4.26).
The study further elaborated on this alarming trend, showing a 3.03% increase (95% CI: 2.04–4.02%) in hospitalizations for schizophrenia and a 3.52% increase (95% CI: 2.38–4.68%) for bipolar disorder under the same temperature conditions. These figures underscore the profound and often destabilizing effect of temperature fluctuations on the mental well-being of older adults, highlighting the urgent need for mental health support and adaptive strategies to help this population cope with the psychological stressors of a changing climate.

7. **High Daily Temperature and Renal Function Impairment**The kidneys, vital organs responsible for filtering waste and regulating fluid balance, are particularly susceptible to the stresses imposed by high ambient temperatures, especially in older adults. As individuals age, renal function naturally declines, and the ability of the kidneys to efficiently respond to environmental stressors like dehydration or heat-induced physiological changes becomes compromised. This vulnerability is further compounded by common age-related conditions and medications.
An Israeli retrospective cohort study conducted between 2006 and 2011 explored the association between high daily temperatures and renal function impairment, focusing on a population where anti-hypertensive medication use is common. The study found that a daily increment of 5°C was significantly associated with an increase in creatinine levels, a key indicator of impaired renal function. Among patients in the non-treatment group, baseline creatinine adjusted 0.824 mg/dL showed a percentage change of 1.212% (95% CI: 0.082–2.354).
The impact was even more pronounced in the group treated with anti-hypertensive medication, where the baseline adjusted creatinine of 1.032 mg/dL saw a larger percentage change of 3.440% (95% CI: 1.227–5.700), suggesting a potential interaction between medication and heat stress on kidney function. Reinforcing this finding, a Canadian retrospective cohort study from 2005 to 2012 revealed that heat periods were associated with an 11% higher risk for acute kidney injury (AKI). These studies collectively highlight that elevated temperatures pose a tangible and serious threat to renal health in older adults, necessitating careful monitoring and proactive hydration strategies during warm weather events.
Navigating the increasingly complex tapestry of climate change, our journey continues beyond immediate, acute health crises to explore the broader systemic impacts that subtly, yet profoundly, reshape the health landscape for older adults. This section delves into overarching mortality trends, the insidious creep of cognitive decline, and unexpected physical risks. Crucially, we also illuminate how inherent vulnerabilities such as age itself, and socioeconomic standing, amplify these challenges, creating a multi-layered threat that demands our focused attention and adaptive strategies.

8. **All-Cause Mortality from Temperature Deviation and Seasonal Mean Temperature**Beyond the dramatic surges in heat-related hospitalizations, the more subtle, yet pervasive, changes in temperature patterns across seasons and even within daily cycles exert a significant toll on overall mortality rates among older adults. These deviations from what the human body considers ‘optimum’ temperatures represent a chronic stressor, challenging the delicate physiological balance required to sustain life, particularly in those whose adaptive capacities are already diminished by age.
Research conducted in Japan, spanning over four decades, revealed a sobering truth: even moderate abnormalities in daily temperature, quantified by the temperature deviation index (TDI), were consistently associated with an increase in all-cause mortality. Specifically, an average 0.5% increase in mortality was observed for every 1-unit rise in TDI. This vulnerability was further amplified on summer days with otherwise moderate temperatures, where the mortality increase climbed to 1.9% per 1-unit increase in TDI, underscoring the insidious danger of seemingly less extreme conditions when they deviate from typical patterns. Similarly, a comprehensive ecological study in the USA indicated that even a modest 1°C rise in summer mean temperature corresponded to a 2.46% increase in the death rate, while winter saw a 1.46% increase, illustrating the year-round impact of warming trends on life expectancy.
Such findings highlight that it is not merely the spikes of extreme heat that pose a threat, but the overall shift in ambient temperature norms. The study also elucidated the impact of temperature variability—the fluctuations within seasons—showing that a 1°C increase in temperature variability translated to a 3.71% rise in annual summer deaths and a 0.59% increase in winter. This nuanced understanding of temperature-related mortality reveals how both rising averages and greater unpredictability in our climate contribute to an accelerated aging process and heightened mortality risk for our elderly populations.

9. **Heart Failure-Related Mortality and Hospitalizations from Temperature Decreases**While much of the discourse around climate change and health rightfully focuses on the perils of rising temperatures, an equally critical, and often overlooked, aspect is the impact of cold. For older adults, particularly those with pre-existing cardiovascular conditions like heart failure, even a modest drop in ambient temperature can significantly increase the risk of severe health events, including hospitalizations and death. The body’s physiological response to cold, such as vasoconstriction and increased blood pressure, can place immense strain on an already compromised heart.
A retrospective cohort study conducted in Canada meticulously tracked the relationship between mean daily temperatures and heart failure outcomes over a decade. The results unveiled a clear and concerning pattern: for every 1°C decrease in the mean daily temperature, the risk of heart failure events—encompassing both death and hospitalization—increased by approximately 0.7%. This effect was consistent whether observed over a three-day or seven-day lag period, indicating that sustained or even short-term decreases in temperature can quickly trigger adverse outcomes for vulnerable individuals.
This specific finding underscores the need for a comprehensive approach to climate adaptation that considers both ends of the temperature spectrum. Older adults, often with reduced mobility and less efficient thermoregulation, may struggle to maintain core body temperature during colder periods, leading to complications that can rapidly escalate. Protecting this demographic from temperature extremes, both hot and cold, is paramount in mitigating the cardiovascular burden imposed by a fluctuating climate.

10. **Extreme ENSO Conditions and Non-Accidental All-Cause Mortality Risks**Far from localized weather events, large-scale oceanic phenomena, such as the El Niño-Southern Oscillation (ENSO), exert a profound global influence, fundamentally altering weather patterns and, consequently, human health. These irregular periodic variations in tropical Pacific Ocean temperatures ripple across continents, affecting everything from rainfall to storm frequency, and as research now reveals, significantly impacting all-cause mortality among older populations.
A retrospective cohort study in China, spanning two decades, meticulously analyzed the health consequences of extreme ENSO conditions. The findings unequivocally demonstrated that both exceptionally low and exceptionally high levels of ENSO, observed over lag periods of up to 12 months, were consistently associated with increased non-accidental all-cause mortality risks. This intricate connection reveals how distant oceanic temperature fluctuations can translate into tangible threats to human life, highlighting the interconnectedness of global climate systems and local health vulnerabilities.
These large-scale climate drivers, often perceived as abstract meteorological concepts, possess a direct and measurable impact on public health. The study’s insights into ENSO-related mortality emphasize that the health implications of climate change are not confined to direct exposure to heatwaves or air pollution but extend to the broader, systemic alterations in global weather patterns. Understanding these far-reaching effects is crucial for developing robust, geographically tailored public health strategies that account for the diverse manifestations of a changing climate.

11. **Daily Temperature Range (DTR) and Cardiovascular Emergency Admissions**Beyond merely average or extreme temperatures, the diurnal temperature range (DTR)—the difference between the maximum and minimum temperatures within a single day—emerges as another critical climate change phenomenon with significant health implications. For older adults, whose physiological systems may struggle with rapid adjustments, large swings in temperature within 24 hours can impose considerable stress, particularly on the cardiovascular system, leading to an increased risk of emergency medical interventions.
An ecological study conducted in China specifically investigated the correlation between an increased DTR and emergency room admissions for cardiovascular diseases. The findings were stark: a 1°C increase in the daily temperature range was associated with a 1.46% increase in all cardiovascular diseases for females, including ischemic heart disease and cerebrovascular disease, with these effects manifesting as a 2-day lag. For males, a 1°C increase in DTR corresponded to a 1.13% increase in all cardiovascular diseases, with cerebrovascular disease seeing a 2.13% rise, and effects observed after a 4-day lag.
These results underscore that the variability of temperature, rather than just its absolute value, is a potent stressor. Older individuals, especially those with underlying cardiovascular conditions, may find it challenging to adapt to rapid changes in ambient temperature, leading to physiological strain that can trigger acute cardiac events. Recognizing DTR as a significant health indicator provides crucial data for informing public health advisories and urban planning, particularly in regions prone to such dramatic daily temperature swings.

12. **Temperature Variability and Dementia-Associated Hospitalizations**The impact of a hotter, more volatile world extends profoundly into the realm of cognitive health, revealing a distressing link between temperature fluctuations and the exacerbation of neurological disorders such as dementia. For older adults, who may already be experiencing diminished cognitive function, these environmental stressors can significantly destabilize their well-being, leading to increased rates of hospitalization and further decline.
A prospective cohort study in the USA delved into the nuanced relationship between temperature patterns and dementia-associated hospitalizations. The research uncovered a statistically significant association: an increase in summer mean temperature was linked to a 12% rise in the risk of hospitalization for dementia. This finding alone highlights the vulnerability of cognitively impaired individuals to sustained periods of warmth, which can disrupt thermoregulation, induce dehydration, and worsen existing neurological symptoms.
Even more compelling was the revelation regarding temperature variability. The study found that a mere 0.5°C increase in the variability of summer temperature was associated with a 7% increased risk of dementia-associated hospitalization. This indicates that unpredictable temperature swings, not just absolute heat, pose a serious threat to cognitive stability. These insights underscore the urgent need for targeted interventions, such as ensuring access to climate-controlled environments and enhanced support systems, to protect older adults from the compounding mental health challenges presented by a changing climate.
13. **Strong Winds and Hip Fracture Incidence**While many climate-related health impacts are tied to temperature and air quality, climate change also encompasses altered weather phenomena like strong winds, which can have surprising and direct physical consequences for older adults. For a population already at increased risk of falls and bone fragility, powerful gusts of wind represent a tangible and often underestimated environmental hazard, leading to serious physical injuries that can profoundly impact quality of life and longevity.
An intriguing case-crossover study in Spain explored the relationship between weather conditions and the incidence of hip fractures in two distinct climate regions. The findings revealed a compelling link: in the Mediterranean climate, days characterized by more frequent and/or high-speed winds were associated with a significant 23.3% increased risk of hip fracture incidence. This heightened risk highlights how environmental forces, seemingly distinct from heat or pollution, can directly contribute to physical trauma in vulnerable older populations.
Conversely, in the inland climate region, while wind was still present, the observed difference in hip fracture incidence did not reach statistical significance, suggesting that regional climate characteristics and potentially adaptive behaviors or built environments may modulate this risk. This emphasizes the importance of understanding localized climate impacts and developing region-specific preventative strategies, such as improving urban design to mitigate wind exposure or implementing early warning systems for high-wind events, to safeguard older adults from such direct physical dangers.
14. **The Amplifying Role of Socioeconomic Status, Education Level, and Age Subpopulations**The narrative of climate change’s impact on older adults is not uniform; rather, it is significantly amplified or modulated by a complex interplay of socioeconomic factors, educational attainment, and even distinctions within the older adult demographic itself. These intersecting vulnerabilities create layers of risk, meaning that some older individuals bear a disproportionately heavier burden of climate-related health consequences.
Crucially, low socioeconomic status emerges as a consistent amplifier of adverse health outcomes. Research indicates that poverty is correlated with an increased risk of dementia hospitalization linked to higher winter temperatures and temperature variability. Similarly, the heightened mortality risk associated with ENSO conditions was found to be even greater in families with low per capita income. These findings illustrate how limited resources—whether financial, housing, or healthcare access—profoundly diminish an individual’s capacity to cope with environmental stressors, making adaptation a privilege rather than a given.
Educational attainment also plays a significant role in modulating vulnerability. Studies have shown that the relative risk of respiratory admissions during wildfire smoke waves was notably higher for individuals residing in areas with lower educational levels compared to those in more educated communities. This suggests that access to information, understanding of health risks, and the ability to implement protective measures are vital buffers against climate impacts. Furthermore, the review revealed critical disparities within older age groups: individuals aged 78 years or older faced a 15% increased risk of renal, heat, or respiratory hospitalizations after extreme heat, compared to a 7% increase in the 65–77 age group. Similarly, those aged 85 and over carried a greater burden of temperature-related mortality due to both cold and hot conditions, underscoring that vulnerability escalates with advanced age.
As we navigate the profound challenges of a warming world, it becomes unequivocally clear that climate change is not merely an environmental crisis; it is a profound health crisis, particularly for our older generations. The intricate web of health impacts—from surging mortality rates due to shifting temperature norms and oceanic oscillations, to the subtle erosion of cognitive function, and the unexpected physical dangers posed by strong winds—paints a comprehensive picture of vulnerability. Yet, the story doesn’t end there; socioeconomic disparities and the specific physiological frailties that come with advanced age further amplify these risks, creating a critical urgency for tailored, equitable, and proactive interventions. This systematic review stands as a powerful testament, urging us to acknowledge these interconnected threats and to champion effective strategies for adaptation and mitigation, ensuring that a better quality of life remains attainable for all citizens, especially those most susceptible to the environmental shifts of our time.