A notable increase in highly contagious diseases is currently sweeping across parts of the United States, prompting public health departments to issue alerts and intensify surveillance efforts. From the widespread rise of Hand, Foot, and Mouth Disease (HFMD) predominantly affecting young children to a burgeoning summer wave of COVID-19, the nation is navigating a complex landscape of viral activity.
Adding to the concerns, broader respiratory illness activity, encompassing conditions such as the common cold, influenza, and respiratory syncytial virus (RSV), is now classified as “high” across the country. These interconnected public health challenges underscore the critical importance of vigilance and adherence to established preventative measures.
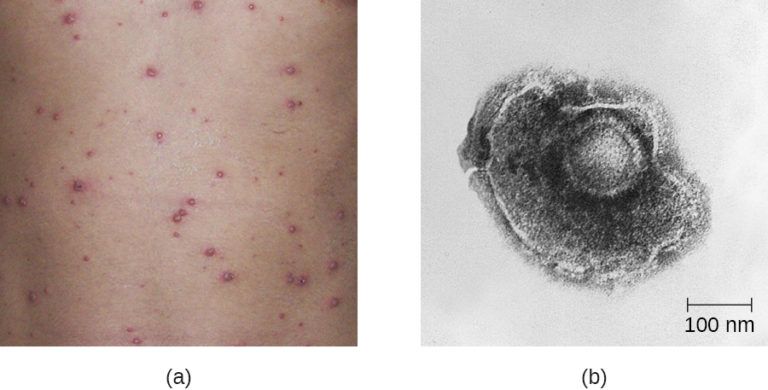
Hand, Foot, and Mouth Disease, a highly contagious viral illness, is most prevalent among children under five years of age. However, health experts emphasize that individuals of all ages are susceptible to infection. The Centers for Disease Control and Prevention (CDC) provides foundational guidance on this common yet impactful disease.
Earlier this year, the Fairfax County Health District in Virginia publicly announced six separate HFMD outbreaks, primarily affecting children four years old and younger. This localized surge provided an early indicator of the escalating transmission patterns observed across the nation.

In a concerning development, the U.S. Virgin Islands Department of Health has confirmed 189 cases of HFMD in St. Thomas. This figure includes a particularly distressing report of a possible fatal case involving a toddler, highlighting the potential for severe outcomes, albeit rare.
In March, the Pan American Health Organization (PAHO) took proactive steps by issuing an alert to its member states. The organization urged them to “strengthen the prevention and control of hand, foot and mouth disease, especially in children, due to their high vulnerability and the risk of serious complications in the central nervous system.”
Dr. Marc Siegel, a senior medical analyst, offered insights into the evolving nature of HFMD. He noted that “The number of cases are increasing (especially type A6) and are spreading to adults with more unusual symptoms, including worse rashes (more widespread) and nail loss.”
HFMD typically manifests with a distinctive set of symptoms. These commonly include blistering sores that appear inside the mouth, accompanied by a rash on the hands and feet. Patients may also experience fever and a sore throat, contributing to the overall discomfort.

The rash associated with HFMD is often described as either raised or flat red spots. These spots possess the potential to develop into blisters, further distinguishing the visual presentation of the illness. Understanding these specific symptoms is crucial for early identification and management.
Tina Q. Tan, M.D., an attending physician at the Ann & Robert H. Lurie Children’s Hospital of Chicago and president of the Infectious Diseases Society of America, observed that HFMD tends to be most common during the warmer months. She stated, “We are seeing more cases at this time,” explaining that it is “a very common infection that is usually mild.”
Transmission of HFMD can occur through several pathways, highlighting its highly contagious nature. Dr. Siegel detailed these routes, which include coughing, sneezing, and contact with runny nose discharge. Direct personal contact such as kissing can also facilitate spread.
Furthermore, sharing utensils, contact with blister fluids, and exposure during diaper changes are significant modes of transmission. Individuals can also inadvertently spread the virus after touching contaminated objects and surfaces, underscoring the importance of environmental hygiene.
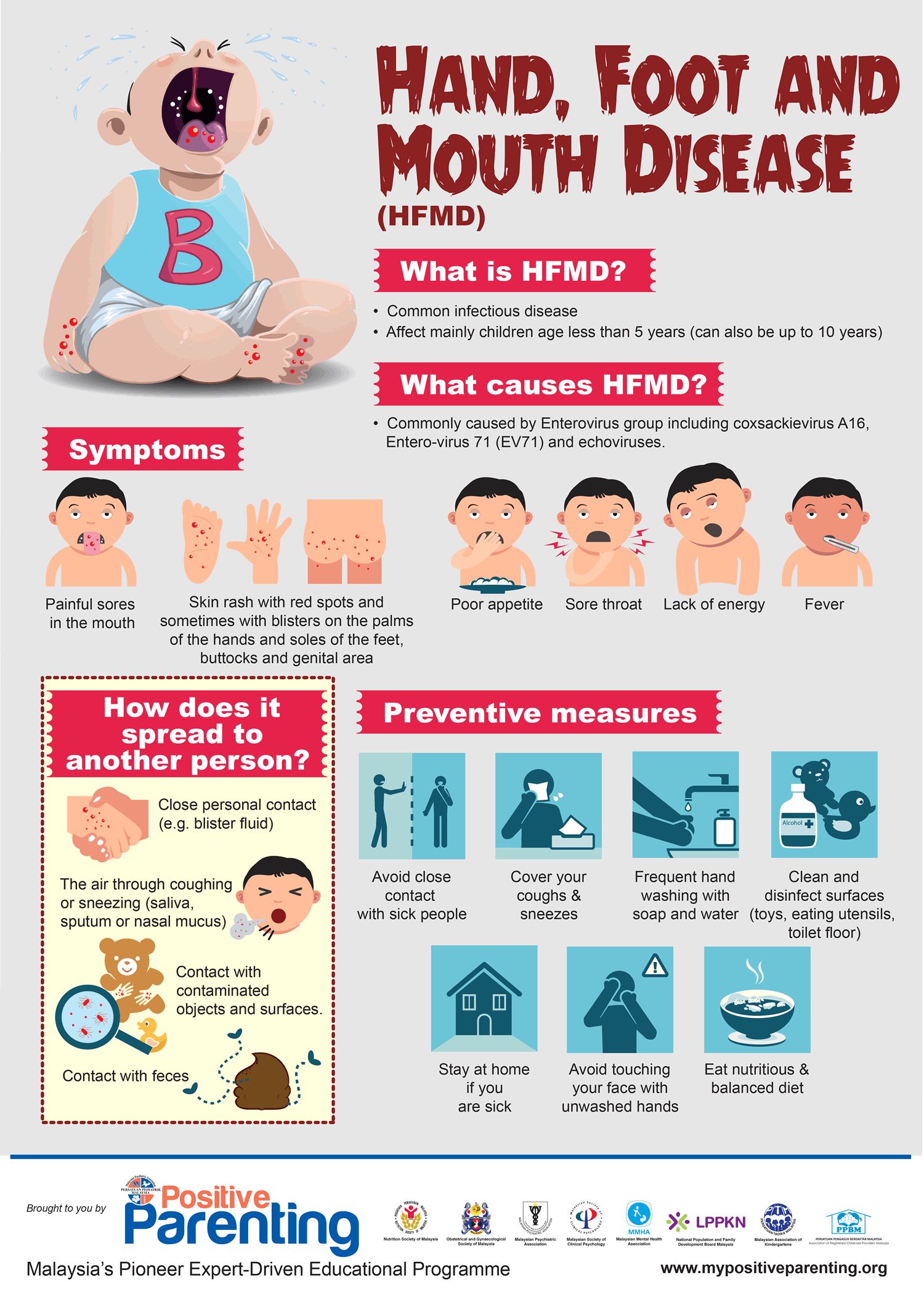
While HFMD is generally considered mild, it remains contagious for several weeks following infection. The period of highest infectivity is particularly concentrated in the first week after the onset of symptoms, necessitating heightened caution during this phase.
Although most individuals experience mild illness and recover without specific treatment within seven to ten days, managing symptoms is key to comfort. Over-the-counter medications can effectively manage pain and fever, providing relief during the course of the illness.
Crucially, the CDC recommends ample fluid intake to prevent dehydration, which can be a common issue, especially in young children with painful mouth lesions. Adequate hydration is vital for recovery and overall well-being during the illness.

While rare, complications from HFMD can be serious. Dehydration remains the most common complication, directly linked to the discomfort caused by painful mouth lesions that can hinder adequate fluid intake. This highlights the importance of monitoring hydration levels.
In rare instances, HFMD can lead to more severe neurological complications. These include viral meningitis, an inflammation of the membranes surrounding the brain and spinal cord, and encephalitis, which is inflammation of the brain itself. Paralysis is also a very rare, but possible, outcome.
Dr. Tan also pointed out that HFMD “can also cause nail loss in those individuals who had involvement of fingers.” This unusual symptom underscores the broader systemic impact the virus can have beyond the typical rash and mouth sores.
Public health experts advise seeking medical care under specific circumstances. Patients or parents should consult a doctor “if they feel they are uncomfortable with the symptoms that they or their child are having and the symptoms are worsening.”
Additional warning signs that necessitate medical attention include an inability to take adequate fluids, a noticeable decrease in urine output, or any observed change in mental status. These indicators suggest potential complications requiring professional assessment.
In settings where children congregate, such as daycares and schools, HFMD is known to spread easily. This characteristic makes these environments particularly vulnerable to rapid outbreaks, impacting routines and requiring swift public health responses.
Guidance on returning to school or daycare is clear: “Infants and children can return to school or daycare when they are feeling better,” Dr. Siegel advised. Dr. Tan concurred, adding that children can return “as long as they have no fever, are feeling well enough to drink and participate in activities, and have no open lesions or copious drooling when they have mouth sores.”
Read more about: The Bedding Bailout: One Sleepover Horror Story That Proves Why Clean Sheets Are the Ultimate Escape Plan

Preventative measures are fundamental in curbing the spread of this highly contagious virus. The CDC strongly recommends frequent handwashing with soap and water, a simple yet highly effective barrier against transmission.
In addition to personal hygiene, cleaning and disinfecting common surfaces and shared items are crucial. Dr. Tan specifically advised attention to doorknobs and toys, which are frequently touched and can harbor the virus. Currently, there is no vaccine available for HFMD in the U.S.
Beyond HFMD, the Centers for Disease Control and Prevention has updated its assessment of overall respiratory illness activity across the United States. The current classification indicates a “high” level of activity for conditions like the common cold, flu, COVID-19, and respiratory syncytial virus.
Read more about: Europe’s Climate Crisis: A Call for Immediate Action and Adaptation
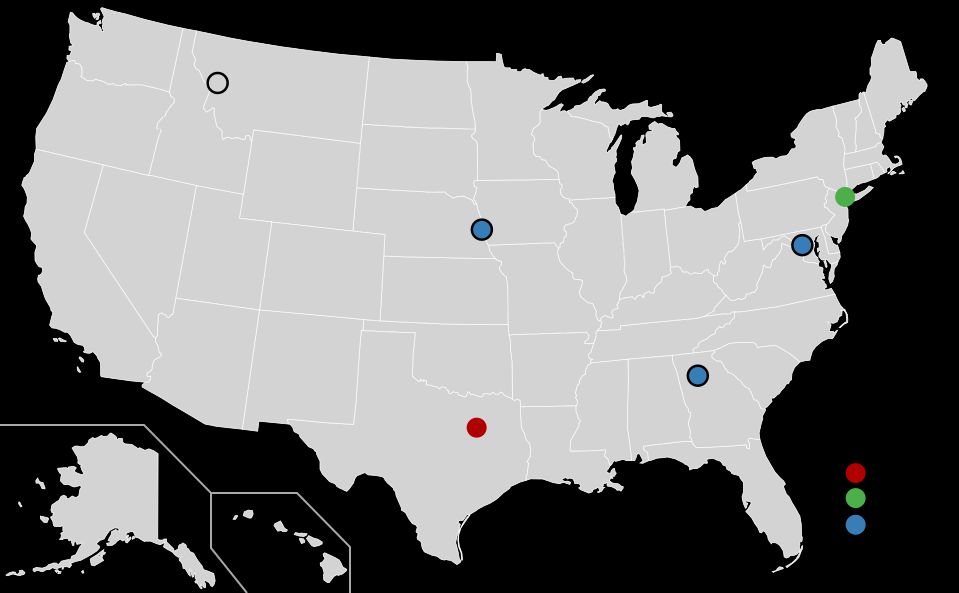
Geographical variations in respiratory virus activity are evident across the nation. New Hampshire is presently experiencing “very high” activity, signaling intense transmission rates within the state. This elevates concerns for its healthcare infrastructure.
Furthermore, eleven states have been categorized as having “high” activity levels. These states include Arizona, Delaware, Georgia, Idaho, Kansas, Kentucky, Louisiana, Oklahoma, Tennessee, Texas, and Wisconsin, indicating significant viral circulation.
Meanwhile, twenty-nine states are currently listed as experiencing “moderate” respiratory illness activity. The remaining states report “low” activity, suggesting a varied national picture of viral prevalence and impact.
Read more about: Unlocking Your Body’s Best Defense: 14 Everyday Foods That Power Up Your Immune System – Will You Give Them a Try?

Both COVID-19 and seasonal flu activity are on an upward trajectory across the country, alongside a rise in RSV cases. This concurrent increase in multiple respiratory pathogens presents a complex challenge for public health officials.
The rising number of people visiting emergency departments specifically for these conditions serves as a clear indicator of the increasing burden. Furthermore, the growing proportion of laboratory tests returning positive for one of the three conditions reinforces the trend of escalating transmission.
According to CDC estimates based on data available through the week ending December 21, the current flu season has already accounted for a significant toll. There have been at least 3.1 million illnesses attributed to influenza, underscoring its continued impact.
Read more about: The Great American Economic Divide: Unpacking Public Frustration Amidst Official Growth Claims

Furthermore, the flu has led to an estimated 37,000 hospitalizations and approximately 1,500 deaths so far this season. These figures highlight the severe health consequences that influenza continues to pose to the population.
In a somber update, five pediatric deaths were reported during the week of December 21 alone, bringing the total number of pediatric flu fatalities for the 2024-25 season to nine. This emphasizes the vulnerability of younger populations to severe outcomes.
The presence of the COVID-19 virus, as detected in wastewater surveillance, is also reportedly increasing. This environmental monitoring provides an early signal of rising community transmission, often preceding clinical case upticks.
Mirroring this trend, the number of emergency department visits for COVID-19 is on the rise, as are laboratory test positivity rates. These data points collectively indicate a growing prevalence of the virus across various communities.

In a statement, the CDC predicted, “Based on CDC modeled estimates of epidemic growth, we predict COVID-19 illness will continue to increase in the coming weeks as it usually does in the winter.” This foresees a sustained challenge into the colder months.
For RSV, the CDC has reported increases in both emergency department visits and hospitalizations among children. Concurrently, hospitalizations among older adults in some areas are also increasing, indicating broader impact across age groups.
A summer wave of COVID-19 appears to be actively sweeping across the United States. Current data strongly indicate that cases are on the rise in a majority of the country, accompanied by an uptick in emergency room visits across all age demographics.
This recent surge in transmission is primarily fueled by the emergence of highly contagious new variants. These variants have evolved with enhanced abilities to evade pre-existing immunity, leading to a growing number of Americans experiencing symptoms.
As of July 29, forecasting models from the U.S. Centers for Disease Control and Prevention indicate that COVID-19 infections are either growing or likely growing in 40 states. Conversely, zero states are reporting a decline in infections.
Meanwhile, in nine states, the infection rates are currently assessed as unchanged, reflecting a plateau in their epidemic trends. The most significant increases in transmission are currently observed across the South, Mid-Atlantic, Northeast, and Midwest regions of the country.
While the CDC classifies the national level of COVID viral activity in wastewater as “low,” this masks important regional disparities. At least 10 states reported “high” or “very high” levels as of July 12, indicating concentrated viral loads in specific areas.
Among the states particularly affected by these elevated wastewater levels are California, Florida, and Texas. These regions are experiencing a heightened presence of the SARS-CoV-2 virus, which can serve as an early warning for potential outbreaks.
Read more about: Unmasking Invisible Illness: A Comprehensive Guide to Dysautonomia, POTS, and Related Conditions
Dr. Albert Ko, a professor of public health, epidemiology, and medicine at Yale School of Public Health, has noted this escalating trend. He stated, “We are seeing an increase in COVID-19 with higher SARS-CoV-2 virus activity in wastewater and small rise in COVID-19 hospitalizations.”
Experts underscore that a current scarcity of comprehensive data is impeding real-time tracking of COVID-19. Despite this limitation, clear indicators suggest that transmission is on an upward trajectory, with expectations for continued case increases.
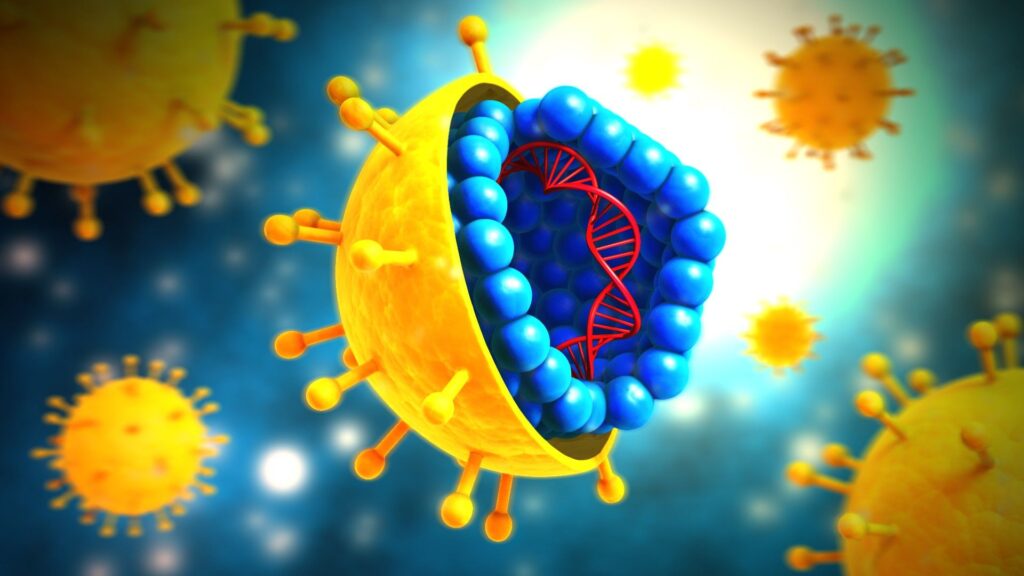
The virus responsible for COVID-19, SARS-CoV-2, continues its relentless process of mutation. This evolution gives rise to new, highly transmissible variants that have developed improved mechanisms for evading the body’s existing immunity, whether from vaccination or previous infection.
Among the variants, NB.1.8.1, commonly referred to as “Nimbus,” has emerged as the dominant strain in the U.S. As of June 21, it accounted for 43% of cases. Anecdotal reports suggest it can cause a painful “razor blade throat.”
Read more about: From Nuclear Engines to Horse Heads: 16 Wild Car Innovations That Failed

However, a newer variant, XFG, also known by the cloud-themed nickname “Stratus,” is rapidly gaining ground. It is spreading quickly worldwide and now represents an increasing proportion of cases in the U.S., making it the third most prevalent strain nationally.
Dr. Ko explains that Stratus is a recombinant variant, meaning it is a hybrid of two existing COVID lineages: LF.7 and LP.8.1.2, both of which are Omicron sub-variants. He noted that it “has a mixture of genetic material from several prior variants, and may be able to better bind to human cells.”
XFG shares structural similarities with NB.1.8.1 but possesses additional changes in its spike protein. These modifications may influence its capacity to evade antibodies generated from vaccination or prior infection, potentially impacting immune response.
Dr. William Schaffner, a professor of infectious diseases at Vanderbilt University Medical Center, reassured the public by stating, “All these new variants are cousins in the same omicron family, (it’s) not some brand new, serious variant.”

The World Health Organization (WHO) has classified XFG as a “variant under monitoring,” assigning it a “low” public health risk. Crucially, there is currently no evidence to suggest that the Stratus variant causes more severe illness compared to its predecessors.
Stratus has already been detected in at least 38 countries globally, indicating its significant international spread. Within the United States, sequences uploaded to the Global Initiative on Sharing All Influenza Data (GISAID) database show its presence in at least 28 states.
For the two-week period ending June 21, XFG comprised 14% of cases in the U.S., trailing only the dominant NB.1.8.1 variant and LP.8.1. However, a four-week delay in publishing new variant proportion data from the CDC suggests these numbers are subject to change.
Dr. Schaffner also discussed the typical pattern of COVID-19 waves. He explained, “Over the past four years, there have been two waves of COVID each year. It’s like a two-hump camel. There’s the summer wave that abates in the fall, and then the winter wave.”
Read more about: Silence the City: How Electric Vehicles are Reducing Urban Noise Pollution

Michael Hoerger, Ph.D., an associate professor at Tulane University School of Medicine, further contextualized the timing of the current surge. He observed, “Every year (since 2020) around Independence Day, we are either already at very high transmission or transmission is really starting to pick up. To me, the situation we’re in is not very surprising.”
COVID-19 activity characteristically intensifies in mid-summer, a period marked by peak travel and increased indoor gatherings, often driven by the use of air conditioning. This seasonal pattern is consistent with previous years.
Historically, the summer wave in the U.S. typically reaches its peak in late July or August. However, viral activity can persist well into September, extending the period of elevated transmission and public health concern.
As immunity levels from prior infections and vaccinations wane, and as new mutated variants like Nimbus and Stratus continue to circulate, experts caution that a substantial portion of the American population will likely remain susceptible to infection this summer.
While the exact scale of this wave remains uncertain, Dr. Schaffner noted, “How large this (wave) will be remains to be determined.” Predictions for the summer 2025 COVID wave vary, with average, larger, or smaller outcomes all considered possibilities by experts like Hoerger.
As of July 26, the weekly test positivity rate stood at 6.5%, representing an increase of approximately 1.6% from the preceding week. While this signifies a rise, it remains considerably lower than the roughly 18% test positivity rate observed during the peak of last summer’s wave.

Hoerger highlighted concerns regarding the current state of data quality. He asserted, “The data quality is pretty poor at the moment. That makes it tougher to know what’s going on. … The situation could be a lot worse than what people are seeing.”
WastewaterSCAN, a system that monitors disease levels through municipal wastewater systems, reports that national COVID levels are currently categorized as “high.” This independent monitoring offers another crucial perspective on community transmission.
Hoerger, who directs the Pandemic Mitigation Collective, utilizes the PMC COVID forecasting model. This model estimated an average of 406,000 new daily infections in the U.S. as of July 28, providing a broad assessment of the current disease burden.
While the full trajectory of this summer’s COVID-19 wave is yet to unfold, Dr. Ko anticipates that “it’s unlikely that it will be as large as the annual winter waves of COVID-19.” This offers a degree of measured optimism about the summer’s outlook.
Current COVID-19 cases are most prevalent in the West and South, although experts caution that this geographical distribution may shift as the summer wave progresses. The dynamic nature of viral spread necessitates continuous monitoring.
As of July 29, the CDC’s COVID-19 epidemic trend forecasting model estimates that infections are growing or likely growing in 40 states. This broad geographic spread includes states such as Connecticut, Delaware, Florida, Georgia, and Indiana.
Additional states experiencing growth or likely growth include Kentucky, Louisiana, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, New Jersey, New York, North Carolina, Ohio, Oklahoma, Oregon, and Pennsylvania.
Read more about: Texas’s Shifting Sands of Power: Unpacking the Complex Forces Shaping the Lone Star State’s Political Destiny

The list continues with South Carolina, Tennessee, Texas, Utah, Virginia, Washington, and Wisconsin, collectively illustrating a widespread increase in COVID-19 activity across diverse regions of the U.S.
Wastewater surveillance data from the CDC as of July 29 also identified states with the highest levels of SARS-CoV-2. These include Alabama, Alaska, California, Delaware, Florida, Hawaii, Kentucky, Louisiana, and Texas, reinforcing the areas of higher concern.
Symptoms associated with the Stratus and Nimbus variants of COVID-19 appear consistent with those observed in recent Omicron strains. This suggests a predictable symptom profile for many affected individuals.
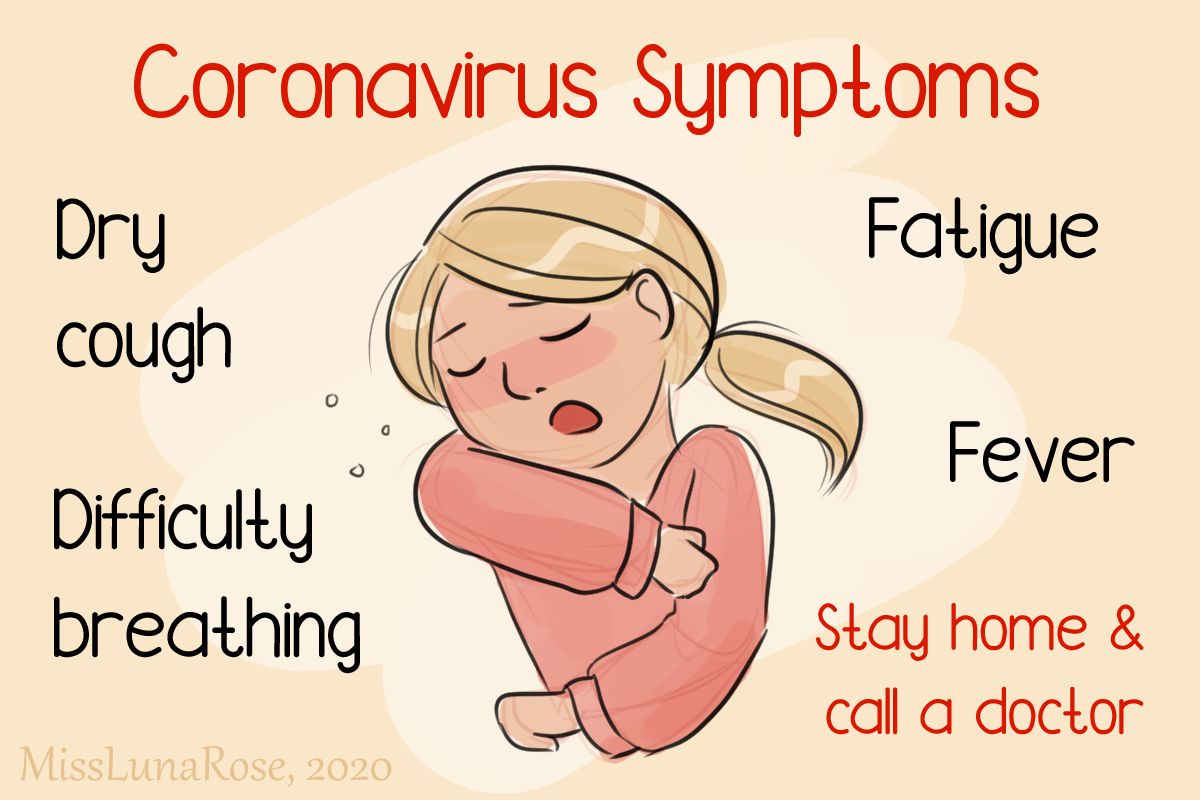
Common COVID-19 symptoms reported in 2025 encompass a range of manifestations. These include a sore throat, often a prominent early sign, along with fever or chills, and a persistent cough.
Other frequently reported symptoms include shortness of breath, headache, and muscle aches. Congestion or a runny nose, fatigue, and a new loss of sense of smell or taste also remain common indicators of infection.
Additionally, some individuals may experience gastrointestinal symptoms such as nausea or vomiting, and diarrhea. The array of symptoms underscores the varied presentation of the illness from person to person.
Read more about: Embrace Spring: Why Starting a Home Garden Will Transform Your Life, Health, and Family Connections

A sore throat has been consistently documented as a sign of COVID-19. Recently, anecdotally, a specific manifestation associated with Nimbus, dubbed “razor blade throat,” has gained traction online for its reported severity.
Dr. Schaffner noted that this “razor-sore throat is more on the basis of anecdotes that careful clinical study,” cautioning against over-reliance on unverified reports. He emphasized that COVID-19 symptoms, and their severity, can vary considerably among individuals.
Hoerger reiterated the importance of testing, explaining that “The symptoms of COVID could look like a lot of different things.” Early and accurate testing is crucial for appropriate diagnosis and subsequent management of the illness.

Upon testing positive for COVID-19, prompt treatment with antiviral medications, such as Paxlovid, is available. This treatment is particularly vital for high-risk groups, as advised by Dr. Schaffner.
These high-risk categories include individuals over the age of 65, those who are immunocompromised, and people with various underlying health conditions. Timely access to antivirals can significantly reduce the risk of severe illness and complications.
Vaccination remains the most effective strategy for preventing severe illness and mitigating complications arising from COVID-19. Current vaccines are expected to retain their efficacy against both the XFG (Stratus) and NB.1.8.1 (Nimbus) variants, as affirmed by the WHO.
The 2024-2025 COVID-19 vaccines, which were released last fall in the U.S., continue to be available and are recommended for most adults. These updated formulations are critical for maintaining population-level immunity.
Read more about: You Won’t Believe These 13 Celebrities Are Working Regular Jobs Now

Hoerger strongly advised, “If somebody hasn’t been vaccinated in about a year, they should definitely go and get it, because they may need it for this wave.” This emphasizes the importance of staying current with vaccinations.
High-risk individuals who received their vaccination last fall or winter may benefit from an additional dose to bolster their protection. Dr. Schaffner urged, “If you’re high-risk, please get your COVID vaccine to carry you through the summer.”
Looking ahead, the updated 2025-2026 COVID vaccines, which are designed to target the LP.8.1 lineage, are anticipated to be released this fall. These new vaccines aim to provide even more tailored protection against circulating strains.
However, recent adjustments to vaccination guidelines may inadvertently make it more challenging for certain demographic groups to receive the shot. This includes pregnant women and children, whose access might be affected by these updated protocols.

For any questions or concerns regarding COVID-19 vaccination, individuals are encouraged to consult their healthcare provider. A doctor can offer personalized advice based on individual health status and risk factors.
In addition to the flu, CDC data indicates that emergency department visits and hospitalizations for RSV are increasing among children. Concurrently, hospitalizations due to RSV are also on the rise among older adults in certain regions.
Despite the availability of vaccines for both flu and COVID-19 for children and adults, and RSV vaccines for specific adult groups, vaccination coverage nationwide remains low. This gap in protection leaves many vulnerable.
Read more about: Inside Marjorie Taylor Greene’s Wide-Ranging Policy Interventions: Census, Vaccine Clashes, and Legislative Ambitions

Public health officials utilize various tools to track and interpret epidemic trends, including the time-varying reproductive number, denoted as R_t. This measure of transmission is derived from data on incident emergency department visits, offering a dynamic view of disease spread.
R_t is defined as the average number of new infections caused by each infectious person at a particular time. It accounts for current population susceptibility, the impact of public health interventions, and evolving behavior patterns within the population.
An R_t value greater than 1 indicates that infections are currently growing, as, on average, each infected person is causing more than one new infection. Conversely, an R_t value less than 1 suggests that infections are declining.
Read more about: Boston’s Unconventional Blueprint: Exploring the Quirks and Hidden Lore of a City Forged by Time

This metric serves as a leading indicator, providing an early signal of potential increases or decreases in subsequent cases, hospitalizations, or deaths. This is because transmission events precede clinical confirmations or adverse outcomes.
The uncertainty range surrounding each R_t estimate helps determine the probability of infection growth. For instance, if 75% of the uncertainty range falls above 1, there is a 75% chance that infections are growing in that specific location.
The model used to generate R_t estimates tends to produce values nearer to 1 with wider credible intervals when data are sparse. This reflects the inherent uncertainty in accurately determining the true epidemic trend during periods of limited data.
Read more about: Scoop Up Success: How Digital Loyalty Programs Are Revolutionizing Ice Cream Shops for Year-Round Profitability
R_t estimates can tell whether an epidemic trend is growing, declining, or not changing, providing an additional tool for public health practitioners to prepare and respond effectively to disease outbreaks.
However, it is crucial to understand what R_t cannot convey. It does not directly reflect the underlying burden of disease. An R_t value less than 1, while indicating declining infections, does not necessarily mean that transmission is low.
Therefore, R_t should be interpreted in conjunction with other surveillance metrics, such as the percentage of emergency department visits, to gain a more complete understanding of the disease burden and public health landscape.

The reliability of R_t estimates can be affected by various factors. They are sensitive to assumptions about the generation interval distribution and may be over- or underestimated if the proportion of infections resulting in emergency department visits changes abruptly.
Such changes can be influenced by shifts in clinical severity, alterations in the use of clinical testing, or modifications in reporting practices. These caveats underscore the importance of expert interpretation of R_t data.
As the nation navigates this complex period of heightened viral activity, the collective commitment to public health measures becomes more critical than ever. From diligent hand hygiene and surface disinfection to staying current with recommended vaccinations, individual actions contribute significantly to community health.

Remaining informed, consulting healthcare providers when symptoms arise, and adhering to public health guidance are essential steps toward mitigating the impact of these surging illnesses. The shared endeavor of public health safeguards the well-being of every community, reflecting a deep responsibility to one another in these times of evolving health challenges.
Read more about: Unveiling the Astonishingly Absurd: Some Bizarre Bits of 19th-Century Advice That Shaped Victorian Girls
The ongoing vigilance, informed by expert insights and robust data, positions communities to adapt and respond effectively to the dynamic nature of infectious diseases. This collaborative approach, rooted in awareness and proactive measures, remains the beacon of public health resilience.



