
When we consider serious heart trouble, the image that frequently comes to mind is the dramatic scene from Hollywood films: a person clutching their chest in agonizing pain before collapsing. This vivid portrayal, however, often overlooks a critical reality, especially for women over 50: heart attacks can manifest subtly, silently, and without the classic, unmistakable symptoms. These ‘silent heart attacks’ are just as dangerous, yet their lack of overt drama means they often go unrecognized, delaying crucial medical attention and potentially leading to severe, irreversible heart damage.
Indeed, findings reveal that women often wait longer than men to seek medical help for heart attacks, largely because they fail to recognize these sneaky, non-traditional symptoms. For women over 50, the challenge is compounded by hormonal shifts after menopause, which increase the risk of coronary artery disease and can alter symptom presentation. Unlike men, who predominantly experience chest pain, women may encounter a range of subtle signs that are easily mistaken for stress, aging, or other common ailments, further contributing to higher misdiagnosis rates.
Understanding these hidden warning signs and risk factors is not merely beneficial; it is absolutely crucial for early detection and prevention. This comprehensive guide aims to shed light on 13 such subtle, often-overlooked indicators, empowering women over 50 to recognize these critical signals and advocate for their heart health. By becoming aware of these less obvious signs, we can collectively work towards earlier diagnosis and better outcomes in the fight against heart disease, a condition that tragically claims the lives of 1 in 3 women, many of whom remain unaware of their personal risk.

1. **Unexplained Fatigue and Weakness**Excessive fatigue is a significant and often disregarded symptom that can signal a silent heart attack in women over 50. This profound tiredness frequently appears without the characteristic chest pain or any other clear, identifiable reasons. Women might find themselves struggling with simple, routine tasks, such as climbing a flight of stairs or performing light housework, even after they believe they have had sufficient rest.
Hormonal changes following menopause significantly elevate the risk of coronary artery disease, a condition that directly impacts the flow of blood to the heart muscle. The fatigue associated with these underlying cardiac issues is unique to each individual, but it is notably more prevalent in women than in men, often presenting as a pervasive lack of energy that does not improve with rest.
It is critically important not to dismiss this sudden or persistent weakness as a normal, unavoidable part of the aging process. Such symptoms could very well point to serious cardiovascular problems, including conditions like a blood clot forming or existing damage to the heart itself. Prompt medical evaluation is warranted when unexplained fatigue becomes a noticeable and persistent concern.
Ignoring persistent and profound fatigue can delay the diagnosis of silent heart disease. When the heart struggles to pump oxygenated blood efficiently, the entire body receives less vital oxygen, leading to this pervasive exhaustion. Recognizing this subtle sign early can be a key step in preventing further complications and protecting overall heart health.
Read more about: Listen Up: 14 Critical Signs Your Body Is Quietly Signaling Nutrient Deficiencies

2. **Shortness of Breath (Unusual or Sudden)**Shortness of breath, particularly when it occurs unexpectedly or with minimal exertion, can be a critical signal of a silent heart attack or underlying coronary artery disease in women over 50. This symptom may manifest even during light activities, such as a leisurely walk or while ascending a short flight of stairs. Sudden breathlessness that lacks a clear, discernible cause should never be overlooked, especially if it is accompanied by other indicators like unexplained fatigue or a feeling of chest discomfort.
This particular symptom often arises due to a reduction in circulation within the cardiovascular system. When blood vessels are narrowed or blocked by high cholesterol levels, plaque buildup, or the presence of blood clots, the heart is forced to work harder to adequately circulate blood, which in turn makes breathing more difficult. The body’s demand for oxygen cannot be met efficiently, leading to the sensation of breathlessness.
For women over 50, this symptom takes on added significance due to the unique physiological changes that occur with age and menopause. The cardiovascular system may become less resilient, making it more susceptible to such circulatory challenges. Consequently, any uncharacteristic difficulty in breathing, especially if it is recurrent or progressive, warrants immediate medical attention.
Regular medical check-ups, including an electrocardiogram (EKG), can be instrumental in diagnosing potential heart issues early. Furthermore, adopting and maintaining a heart-healthy diet, rich in fruits and vegetables, plays a vital role in supporting cardiovascular function and mitigating the risks associated with reduced blood flow and strained breathing.
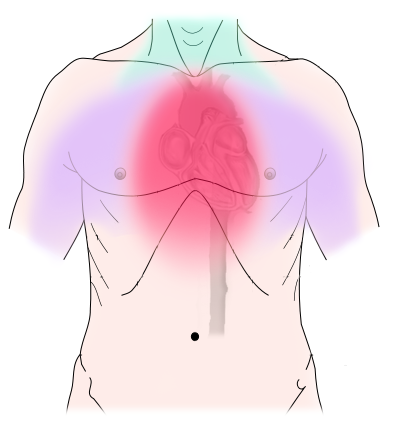
3. **Mild Chest Discomfort or Pressure**Unlike the intense, crushing chest pain typically associated with a dramatic heart attack, a silent heart attack in women over 50 may present as mild chest discomfort or pressure. This sensation can manifest as a subtle tightness, a feeling of fullness, or a squeezing sensation in the chest area. Crucially, this discomfort is often not localized to the chest alone; it can subtly spread to other areas such as the jaw, neck, shoulder, or arm, making it easy to confuse with other less serious conditions.
Many women unfortunately mistake this mild chest pressure for common ailments like heartburn, indigestion, or even a simple muscle strain. Because the pain is not sharp or excruciating, it is frequently dismissed or attributed to non-cardiac causes, delaying necessary medical evaluation. This subtlety is precisely what makes it a ‘silent’ sign, obscuring its true, potentially life-threatening origin.
Even a mild, persistent pressure in the chest area, particularly if it lasts for several minutes or intensifies during physical activity like exercise, could be a critical indicator of coronary artery disease or the formation of a blood clot within the heart’s arteries. The heart’s arteries, when narrowed or blocked, struggle to supply oxygen-rich blood, leading to this distinctive discomfort.
For women over 50, vigilant attention to such symptoms is paramount. Early detection of even mild chest discomfort can be pivotal in preventing further heart damage and significantly lowering the risk factors for more severe cardiovascular events, such as a myocardial infarction. Seeking prompt medical help for these subtle but persistent feelings of pressure is a proactive step towards safeguarding heart health.
Read more about: Say Goodbye to Sciatica: 11 Empowering Exercises to Relieve Nerve Pain, Backed by Physical Therapists
4. **Pain in the Neck, Jaw, or Upper Back**Pain that manifests in the neck, jaw, or upper back can serve as a stealthy, yet critical, signal of a silent heart attack, particularly in women over 50. Unlike the more recognized chest pain, women might experience discomfort in these areas without any severe or noticeable pain in the chest itself. This referred pain often radiates from the heart to nearby anatomical regions, a phenomenon that occurs when the brain misinterprets signals originating from the heart as coming from another part of the body. This can be due to blocked blood vessels or coronary artery spasms.
Jaw pain, in particular, is a common presentation that is easily confused with dental issues or temporomandibular joint (TMJ) problems. Similarly, discomfort in the upper back or neck might be dismissed as muscle strain, poor posture, or stress-related tension. These assumptions, while seemingly logical, can unfortunately lead to critical delays in recognizing a cardiac event.
The underlying mechanism for these symptoms is that when blood flow is restricted by a blood clot or plaque buildup in the coronary arteries, oxygen cannot adequately reach certain parts of the body. The pain tends to feel more like a pressure, heaviness, or a dull ache rather than a sharp, localized pain. Cardiology experts emphasize that ‘silent signs like upper backaches should never be ignored,’ underscoring the potential severity of these seemingly innocuous discomforts.
It is essential for women over 50 to be acutely aware that persistent or recurrent discomfort in their jaw, neck, or upper back, especially if it occurs with exertion and improves with rest, warrants immediate medical investigation. This pattern of pain is often a direct sign of blockages within the heart arteries and should not be attributed solely to musculoskeletal issues without a thorough cardiac evaluation.
Read more about: Burt Reynolds, Enduring Icon of Film and Television, Dies at 82

5. **Nausea and Dizziness (and Flu-like Symptoms)**Discomfort in the neck, jaw, or back is frequently accompanied by symptoms such as nausea and dizziness in women who are experiencing silent heart issues. A sudden onset of a queasy stomach, occurring without an apparent reason, should raise a red flag. Similarly, experiencing light-headedness or dizziness can make it challenging to maintain balance or concentrate, indicating a potential underlying problem. These symptoms often get mistakenly attributed to indigestion, a stomach bug, or general malaise, especially since they can mimic common flu-like symptoms.
These signs might surface during periods of mild physical activity, or even while a woman is at rest, highlighting their insidious nature. Silent myocardial infarction symptoms, while subtle, are concerning because they directly signal reduced blood flow to the heart. This reduction in blood supply can lead to possible damage in the heart muscle or the walls of the arteries, even in the absence of traditional, severe chest pain.
For women, particularly those over 50, these flu-like symptoms, including nausea and vomiting, are often more common presentations of heart disease than in men. Dr. Steinbaum notes that women tend to exhibit a higher pain threshold and are accustomed to various monthly discomforts, which can unfortunately lead them to put themselves last and be more reluctant to seek treatment for symptoms they perceive as minor.
Therefore, if you experience persistent nausea, dizziness, or a general feeling of being unwell akin to the flu, especially if these symptoms are new or occur in conjunction with other subtle discomforts, it is imperative to consult your healthcare professional. Prompt evaluation can differentiate between minor ailments and potentially life-threatening cardiac events, ensuring timely intervention.
6. **Heart Palpitations (with or without Dizziness)**Heart palpitations, characterized by a feeling of a rapid, fluttering, or pounding heart, represent a symptom that is frequently disregarded, yet it can be a significant indicator of heart disease, especially in women over 50. These sensations can occur with or without accompanying dizziness and may be a sign of an abnormal heart rhythm, which demands medical attention. The context describes this as a ‘sneaky’ symptom for a very specific reason.
Cardiologist Meghana Rao Brito, specializing in cardiovascular disease in women, emphasizes that ‘A symptom that is often disregarded is frequent palpitations with or without dizziness, which can be due to an abnormal heart rhythm.’ This highlights the potential seriousness of these often-dismissed sensations. When the heart’s electrical signals are disrupted, even temporarily, it can lead to inefficient pumping and potentially serious complications.
Dr. Steinbaum further explains the complexity of palpitations in women over 50: ‘They’re a really common symptom of perimenopause and menopause.’ The fluctuating and declining levels of estrogen and progesterone during these periods can directly impact the electrical signals within the heart, causing these sensations. This hormonal link often leads women to attribute palpitations solely to menopausal changes, inadvertently overlooking their potential cardiac origin.
Given this duality, it becomes crucial to seek medical advice: ‘So palpitations could mean nothing — or they could mean something. It’s worth getting checked out by your doctor.’ This professional guidance is essential to ascertain whether the palpitations are benign hormonal fluctuations or a more serious sign of underlying heart disease that requires intervention to prevent further complications.
7. **Chronic Headaches (especially with Aura)**Chronic headaches, particularly severe migraines or those accompanied by visual changes, can be a subtle yet crucial sign of heart disease, especially in women. The connection between persistent headaches and cardiovascular health often stems from high blood pressure, a primary risk factor for heart disease. When blood pressure remains elevated over time, it can trigger frequent and intense headaches, serving as a warning sign that the cardiovascular system is under strain.
Dr. Steinbaum advises, ‘If you have chronic migraines or experience visual changes, that’s a sign to see your doctor.’ This recommendation underscores the importance of not dismissing such headaches as mere discomfort. A study published in JAMA reinforced this concern, revealing that women who experienced chronic migraines, particularly those with aura (sensory disturbances before or during the headache), faced an increased risk of heart disease. This scientific evidence links what might seem like a neurological symptom directly to cardiac health.
The mechanism behind this connection involves the impact of sustained high blood pressure on blood vessels throughout the body, including those supplying the brain and heart. Chronic vascular stress can contribute to inflammation and damage to the arteries, heightening the risk of coronary artery disease, stroke, and other cardiovascular events. The presence of aura with migraines is thought to indicate a more significant vascular component, further linking these headaches to cardiac vulnerability.
Therefore, for women over 50 experiencing new onset of chronic, severe headaches or migraines, especially with visual disturbances, it is imperative to undergo a thorough medical evaluation. This assessment should go beyond simply addressing headache symptoms and include a comprehensive check of cardiovascular health to identify and manage potential underlying heart disease risks, ensuring a proactive approach to well-being.

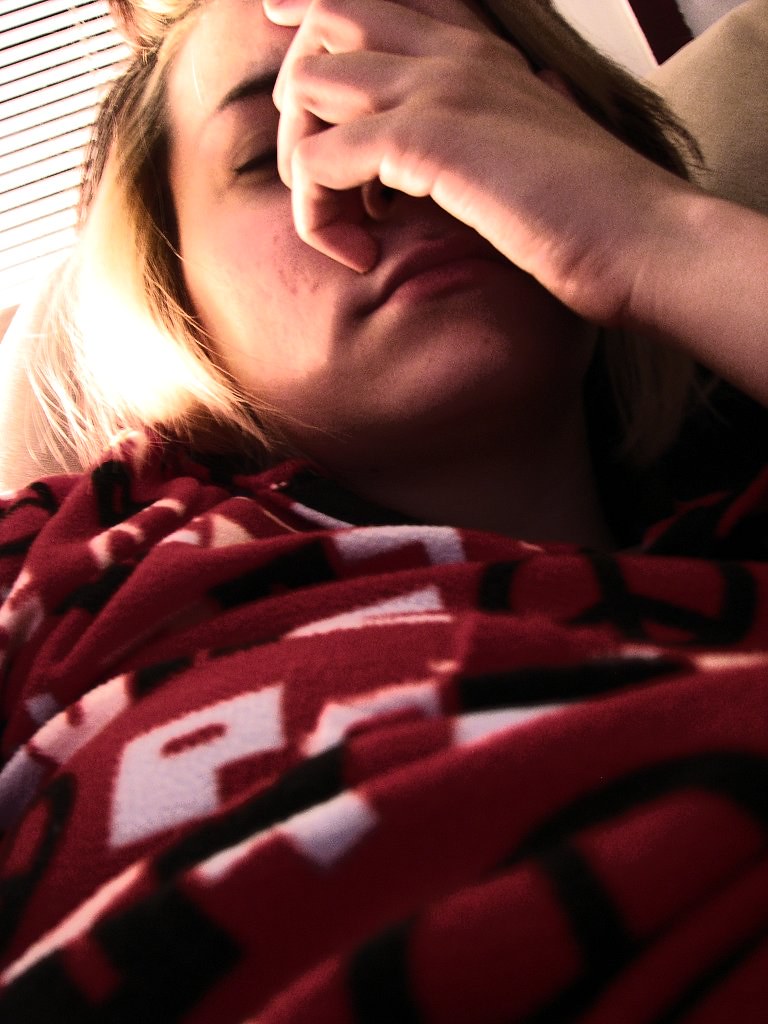
8. **Sleep Apnea and Disturbances**Sleep is fundamental to our overall health, serving as a critical recovery period where our cells undergo restoration. However, when this vital process is disrupted by conditions like sleep apnea or general sleep disturbances, it can have significant implications for cardiovascular health, especially in women over 50. Poor sleep quality is explicitly listed as a major risk factor for heart disease, contributing to chronic inflammation that can detrimentally hamper cardiovascular well-being over time.
Dr. Steinbaum highlights that “Sleep apnea is one of the biggest issues that leads to all types of heart disease, such as coronary artery disease, heart attack, stroke or atrial fibrillation.” This statement underscores the profound and far-reaching impact of disrupted breathing during sleep on the entire cardiovascular system. The repeated pauses in breathing, known as apneic events, cause intermittent drops in oxygen levels throughout the night, placing immense stress on the heart and leading to increased blood pressure and systemic inflammation.
Beyond specific conditions like sleep apnea, general sleep disturbances also warrant careful attention from healthcare professionals and patients alike. Women over 50 may frequently experience difficulty falling or staying asleep, which, rather than being a benign nuisance, can be a subtle indicator of underlying heart issues. These disturbances are sometimes directly linked to reduced oxygen levels in the body, which can be caused by blocked blood vessels and inefficient blood flow, a direct consequence of developing heart disease. Persistent or unexplained changes in sleep habits, therefore, should always be closely monitored and discussed with a doctor.
Chronic lack of restorative sleep not only elevates the risk of high blood pressure but also significantly contributes to the progression of coronary artery disease. When the heart struggles to pump oxygenated blood efficiently, particularly during crucial resting periods, disrupted sleep patterns can become a noticeable and persistent symptom. Recognizing these sleep-related signs early is crucial, as they might point to serious cardiovascular issues like a silent myocardial infarction that require timely medical evaluation and intervention to prevent further damage. It’s a vital clue that the body is under stress, even if other more dramatic heart symptoms are absent.
Read more about: 12 Critical Warning Signs of Sleep Apnea You Can’t Afford to Ignore: A Comprehensive Guide to Understanding and Addressing This Silent Threat

9. **Swelling in the Legs, Feet, or Ankles**Swelling, particularly in the legs, feet, or ankles, can be a telling, yet often overlooked, sign of silent heart disease in women over 50. This symptom, medically known as edema, frequently signals fluid retention within the body’s tissues. Such fluid buildup is often a direct result of the heart’s diminished ability to pump blood efficiently, leading to poor circulation throughout the body and a noticeable accumulation in the lower extremities.
The appearance of persistent or increasing swelling in the lower extremities can be a critical indicator that the cardiovascular system is under significant strain. When the heart is weakened or struggling to pump blood effectively, blood flow can slow, causing fluid to back up in the veins and subsequently leak into surrounding tissues. This accumulation becomes visible as swelling and can be significantly exacerbated by conditions like high blood pressure, which is a key risk factor for heart disease and puts additional strain on delicate blood vessels.
It is imperative that women experiencing such swelling do not dismiss it as a mere consequence of aging, prolonged standing, or simple fatigue. Instead, it should prompt urgent investigation for other potential signs of coronary artery disease or, more critically, the early stages of heart failure. Cardiologist Meghana Rao Brito, specializing in cardiovascular disease in women, explicitly notes that “A buildup of fluid in the ankles, legs or abdomen is another symptom,” underscoring its significant role as a systemic indicator of cardiac distress.
Monitoring your heart health through regular medical checks, including diagnostic tools like an electrocardiogram (EKG), can be instrumental in helping healthcare professionals identify underlying issues early on. Addressing fluid retention and its cardiac origins promptly is vital for preventing severe outcomes and safeguarding overall cardiovascular function. Recognizing this seemingly benign symptom as a potential crucial call for immediate medical action can make a profound difference in long-term heart health.
Read more about: A Heart Surgeon and Survivor’s Vital Warning: 10 Heart Symptoms You Must Never Ignore

10. **Persistent Coughing, Especially While Lying Flat**A persistent cough, particularly one that significantly worsens when lying flat, is a significant systemic indicator of heart disease that women over 50 should never ignore. This symptom, often accompanied by increased difficulty breathing in a supine position, can be a direct manifestation of fluid buildup within the lungs, a condition medically termed pulmonary edema. This critical situation arises when a weakened heart muscle struggles to effectively pump blood forward, causing fluid to back up and collect in the delicate lung tissues.
Many individuals may mistakenly attribute such a cough to a common cold, seasonal allergies, or chronic bronchitis, delaying the necessary cardiac evaluation. However, when a cough is persistent, often dry or producing pink-tinged sputum, and noticeably intensifies upon reclining, it strongly signals a deeper problem beyond typical respiratory ailments. Dr. Rao Brito clarifies this, stating, “Difficulty breathing or coughing while lying flat can also be a sign of fluid buildup in the setting of a weak heart muscle.” This direct connection highlights a critical aspect of heart failure where the heart’s inefficiency leads to detrimental fluid congestion in the lungs.
The underlying mechanism for this symptom involves the heart’s inability to maintain adequate forward circulation, leading to increased pressure in the blood vessels surrounding the lungs. This elevated pressure forces fluid out of the capillaries and into the air sacs, triggering a reflexive cough as the body attempts to clear the accumulating fluid. This particular presentation of coughing, often described as a ‘cardiac cough,’ is therefore a strong physiological warning sign that the heart muscle may be significantly compromised and unable to handle its workload.
Furthermore, the context provides an important insight that “research in The American Journal of Medicine shows that chronic lung infections can weaken the heart, leading to heart disease.” This underscores the complex and often reciprocal interplay between respiratory and cardiovascular health. For women over 50, distinguishing a heart-related cough from other causes is paramount, necessitating prompt medical evaluation to ascertain the underlying cardiac health and prevent further complications from an undiagnosed and progressive heart condition. Early recognition can prevent irreversible damage.
Read more about: Navigating the Shifting Sands: Why 9 Beloved Fast-Casual Chains Are Facing Customer Dissatisfaction and What It Means for the Industry’s Future

11. **Digestive Discomfort or Abdominal Pain**Digestive discomfort or unexplained abdominal pain can be a subtle yet crucial signal of silent heart disease in women over 50, frequently leading to misdiagnosis due to its striking resemblance to common gastrointestinal issues. Women often describe these sensations as persistent indigestion, a feeling of bloating, uncomfortable fullness, or even a burning sensation in the stomach area. These symptoms are easily dismissed by both patients and sometimes healthcare providers, especially since they can mimic familiar digestive problems like acid reflux or irritable bowel syndrome.
The insidious nature of these symptoms means that women with underlying coronary artery disease might experience such pain after consuming fatty or spicy foods, mistakenly attributing it to food intolerance or a routine upset stomach. This critical confusion can unfortunately delay vital medical evaluation, as cardiac symptoms are not typically associated with the digestive tract. The context notes that silent heart attacks may also trigger nausea and vomiting alongside this abdominal discomfort, further contributing to the misperception of a simple stomach bug, food poisoning, or general malaise.
These seemingly innocuous digestive complaints arise from reduced blood flow to the heart, which in turn can affect other organs and systems, including those in the abdominal region. When blood flow is compromised by blocked arteries or the formation of blood clots, the body’s systems do not receive adequate oxygen and nutrients, leading to a cascade of symptomatic responses. The pain might not be sharp or localized but rather a diffuse, uncomfortable sensation across the upper or central abdomen, sometimes radiating to the back.
It is paramount for women over 50 to take persistent or recurrent abdominal discomfort seriously, particularly if it’s accompanied by other subtle signs like unexplained fatigue, shortness of breath, or discomfort in the jaw or back. Ignoring these symptoms could delay a critical cardiac diagnosis, potentially leading to significant and irreversible heart damage. Consulting cardiology experts for advice is essential to differentiate between minor ailments and potentially life-threatening cardiac events, ensuring timely and appropriate intervention and safeguarding long-term heart health.
Read more about: Beyond the Spotlight: Unraveling the Alleged Tragic Autopsy Details of Elvis Presley’s Final Days

12. **Rapid or Irregular Heart Rates**While heart palpitations, characterized by a rapid, fluttering, or pounding sensation in the chest, were discussed previously as a frequently disregarded symptom, a distinct and equally critical sign of silent heart disease in women over 50 involves broader “changes in heart rate or rhythm.” This goes beyond just the subjective sensation of a palpitation, focusing on objectively rapid or irregular heart rates that can directly signal a silent myocardial infarction or underlying coronary artery disease, thus demanding thorough and immediate medical attention.
Women over 50 might notice their pulse racing unexpectedly fast, or beating in an erratic pattern, even when at rest or during light physical activity such as a leisurely walk, without any apparent precipitating cause. This sudden and sustained change in heart rhythm, often distinct from hormonally-driven perimenopausal palpitations, “could hint at coronary artery disease,” as the body reacts to inefficient heart function or electrical instability. Such persistent irregularities can signify that the heart’s electrical system is compromised or that it is struggling to pump effectively against increased resistance.
The physiological basis for these rhythm changes often relates directly to narrowed blood vessels caused by atherosclerotic plaques. These fatty plaques reduce the flow of oxygen-rich blood to the heart muscle, forcing the heart to work harder and potentially leading to electrical instability within its chambers. Such disruptions significantly increase the risks for dangerous blood clots and progressive heart damage, even in the absence of traditional severe chest pain, making them particularly insidious.
Regular medical checks, including an electrocardiogram (EKG), are instrumental in detecting these subtle yet serious changes in heart rhythm early. This proactive diagnostic approach allows healthcare professionals to accurately differentiate between benign fluctuations and critical indicators of cardiovascular compromise, such as arrhythmias signaling underlying disease. Recognizing and acting upon persistent rapid or irregular heart rates is a vital step in preventing advanced heart disease and ensuring timely intervention, which can be life-saving.
Read more about: Chisinau: Unveiling the Enduring Spirit of Moldova’s Verdant Capital

13. **Unexplained Rapid Weight Gain**Unexplained rapid weight gain, particularly when clearly attributed to excess water retention, serves as a crucial yet often overlooked early warning sign of potential heart failure in women over 50. This symptom is a direct physiological reflection of the heart’s compromised ability to efficiently circulate blood throughout the body, leading to a systemic accumulation of fluid within the body’s tissues. It is important to note that this is not merely a general increase in fat, but a sudden and noticeable jump on the scale caused by retained water, often indicating a significant bodily change.
When the heart struggles to pump effectively, fluid can back up into the veins and subsequently leak into surrounding tissues, particularly in dependent areas such as the legs, ankles, and abdomen, and can even affect the lungs. This phenomenon, known as edema, can lead to a significant and rapid increase in body weight over a relatively short period, sometimes several pounds in just a few days. The context explicitly highlights that “Some women experience rapid weight gain from excess water retention” as a specific and concerning indicator of potential heart failure.
It is absolutely vital for women to distinguish this specific type of weight gain from general weight fluctuations or increases due to dietary changes or reduced physical activity. Unexplained rapid weight gain, especially if it occurs alongside other concerning symptoms like increasing shortness of breath, persistent coughing, or swelling in the extremities, warrants immediate and thorough medical investigation. It strongly suggests that the body is retaining fluid because the heart is not effectively moving blood forward as it should.
This symptom should prompt a comprehensive evaluation of cardiovascular health, as it can indicate significant cardiac dysfunction that requires urgent attention. Early recognition and meticulous management of fluid overload are essential in preventing the progression of heart failure and its associated severe complications. Consulting a healthcare professional promptly can help determine the precise cause of the weight gain and initiate appropriate, timely treatment to safeguard long-term heart health and improve quality of life.
As we navigate the complexities of heart health in women over 50, it becomes abundantly clear that vigilance and informed action are our most powerful allies. The journey through these 13 crucial, often silent, indicators underscores a profound truth: our bodies communicate in myriad ways, and listening intently can be life-saving. From subtle changes in sleep patterns to unexplained swelling or sudden shifts in heart rhythm, each symptom offers a piece of the puzzle, inviting us to look beyond the obvious and embrace a proactive stance toward our well-being.
Read more about: Understanding Water Damage: The 10 Vehicles That Survive Floods and the Ones That Fail in Light Rain, Causing Costly Electrical Gremlins
Empowering ourselves with this knowledge transforms potential vulnerabilities into opportunities for early detection and intervention. Remember, these signs are not mere inconveniences; they are vital messages from your heart, urging you to seek professional guidance and prioritize your health. By understanding and advocating for these unique presentations of heart disease in women, we can collectively strive towards a future where fewer silent heart attacks go unnoticed, leading to healthier, longer lives for women everywhere. Your heart’s story is yours to protect—listen closely, act decisively, and champion your own health journey.




