
Many women will encounter ovarian cysts at some point in their lives, these fluid-filled sacs often developing without causing any noticeable symptoms and frequently resolving on their own. However, in certain instances, these cysts can lead to significant discomfort and other health concerns, making an informed understanding of their nature and potential impact crucial for proactive health management.
Remarkably, a 2019 MRI study highlighted a significant connection, revealing that 44.5% of patients experiencing non-spinal lower back pain had ovarian findings. This statistic underscores that while most cysts are benign and small, larger ones possess the capacity to press on surrounding organs and nerves, thereby causing discomfort that can radiate to areas such as the lower back.
This in-depth exploration aims to shed light on ovarian cysts, their various forms, and the intricate ways they can manifest, particularly focusing on the often-overlooked link to lower back pain. By understanding the common symptoms, diagnostic methods, and available treatment pathways, individuals can feel more empowered to make timely and informed decisions regarding their reproductive health and overall well-being.

1. **What Are Ovarian Cysts?**Ovarian cysts are essentially fluid or solid sacs that develop either on or within the ovaries. These formations are quite common and frequently occur as a natural part of the menstrual cycle. While the majority of these cysts are harmless and tend to disappear without intervention, some may necessitate medical attention due to their size, persistence, or the symptoms they produce.
Understanding these structures is the first step toward recognizing potential issues. They are a common gynecological finding and are often discovered incidentally during routine examinations or imaging tests. The presence of a cyst does not automatically imply a severe problem, but it does warrant awareness and, in some cases, monitoring by a healthcare professional.
During ovulation, a follicle on the ovary ruptures to release an egg. If this process is disrupted, a cyst can form. Depending on how and when they form, ovarian cysts are broadly categorized into two main types: functional cysts, which are linked to the menstrual cycle, and non-functional cysts, which are not directly tied to it. Each type has distinct characteristics and potential implications.

2. **Functional Cysts**Functional cysts represent the most prevalent type of ovarian cyst. These cysts are intrinsically linked to the normal process of ovulation and are generally benign, meaning they are non-cancerous. They typically form during the menstrual cycle and are usually temporary, often resolving without any medical intervention within a few cycles.
There are two primary sub-types of functional cysts that are frequently observed: follicular cysts and corpus luteum cysts. Both originate from the regular ovarian activity during a woman’s reproductive years, highlighting their physiological basis rather than an abnormal pathological process. Around 70% to 80% of follicular cysts, for example, resolve on their own.
Follicular cysts develop when the follicle that holds a developing egg fails to rupture and release the egg. Instead, it continues to grow, becoming a cyst. Corpus luteum cysts, on the other hand, form after the egg has been released; in this scenario, the follicle seals itself off and fluid accumulates inside, forming a cyst. Both types are generally considered harmless and often resolve within two to three menstrual cycles.
Read more about: Unlock Your Morning: Physical Therapists Reveal 12 Simple Stretches to Conquer Low

3. How do ovarian cysts cause back pain? Lower back discomfort is a common symptom that may be caused by various health conditions, and ovarian cysts are a notable but sometimes easily overlooked trigger. Although many ovarian cysts are small and harmless, larger ones can exert tremendous pressure on the surrounding organs and tissues, causing pain that radiates to the lower back.
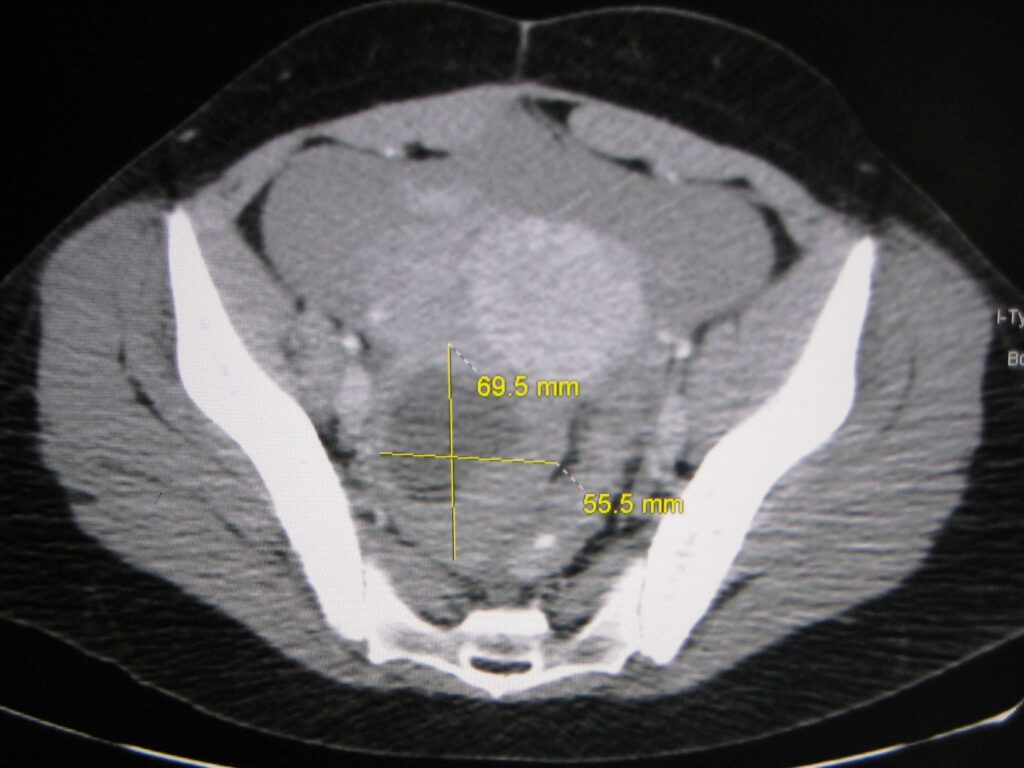
Specifically, when an ovarian cyst grows larger than 5 cm, its increased size can begin to press against sensitive pelvic nerves or the bladder. This persistent pressure often manifests as a dull, aching pain in the lower back. This referred pain is a crucial indicator that a cyst may be growing to a size that requires medical attention.
It is important to differentiate between chronic and acute pain in this context. Chronic discomfort from ovarian cysts is typically a result of persistent pressure on surrounding structures, while acute, sharp, and severe pain may signal a more urgent issue, such as a ruptured cyst or ovarian torsion. According to Dr. Kushner’s findings, 45% of cyst-related cases involve back pain, underscoring its prevalence as a symptom.
Read more about: Unlock Your Morning: Physical Therapists Reveal 12 Simple Stretches to Conquer Lower Back Pain for Good

4. **Common Symptoms Associated with Back Pain from Ovarian Cysts**When ovarian cysts are responsible for lower back pain, this discomfort is often not an isolated symptom. It typically appears alongside a constellation of other signs that collectively point towards an ovarian origin. Recognizing these accompanying symptoms can provide crucial clues for individuals and their healthcare providers in diagnosing the underlying issue.
One of the frequently reported co-occurring symptoms is a sensation of pelvic fullness or pressure. This feeling is often described as a heaviness in the lower abdominal or pelvic region, resulting from the cyst’s physical presence and its compression of internal organs. This pressure can be constant or intermittent, depending on the cyst’s size and position.
Bloating, characterized by swelling or discomfort in the lower abdomen, is another common companion to cyst-related back pain. This symptom can be due to fluid retention or the sheer volume occupied by a larger cyst within the abdominal cavity. It can often mimic other conditions, such as irritable bowel syndrome (IBS), making accurate diagnosis important.
Urinary urgency, defined as a frequent need to urinate or difficulty completely emptying the bladder, can also arise. This occurs when an enlarged cyst presses directly on the bladder, irritating it and reducing its functional capacity. Similarly, bowel issues like constipation can develop if the cyst exerts pressure on the intestines, impeding normal bowel movements.

5. **Types of Ovarian Cysts That May Cause Back Pain**While any sufficiently large ovarian cyst has the potential to cause back pain, certain types are more frequently implicated due to their growth patterns, composition, or association with other conditions. Understanding these specific types can help in identifying those that warrant closer observation and prompt medical evaluation.
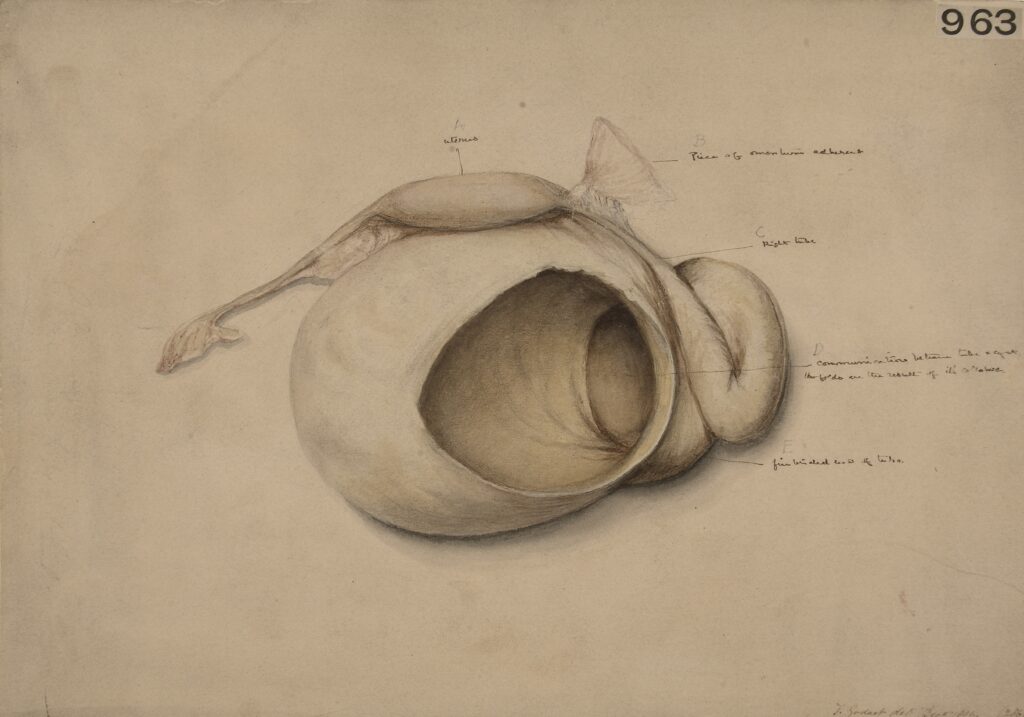
Among these, dermoid cysts are notable contributors. These congenital cysts, which contain tissues such as hair, skin, or sometimes even teeth, grow slowly but can eventually reach a size where they press on pelvic nerves or other organs. This compression can lead to radiating pain that is often felt in the lower back.
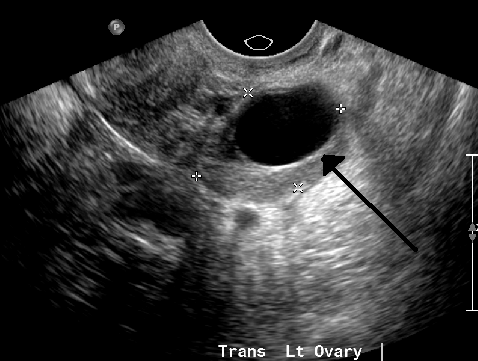
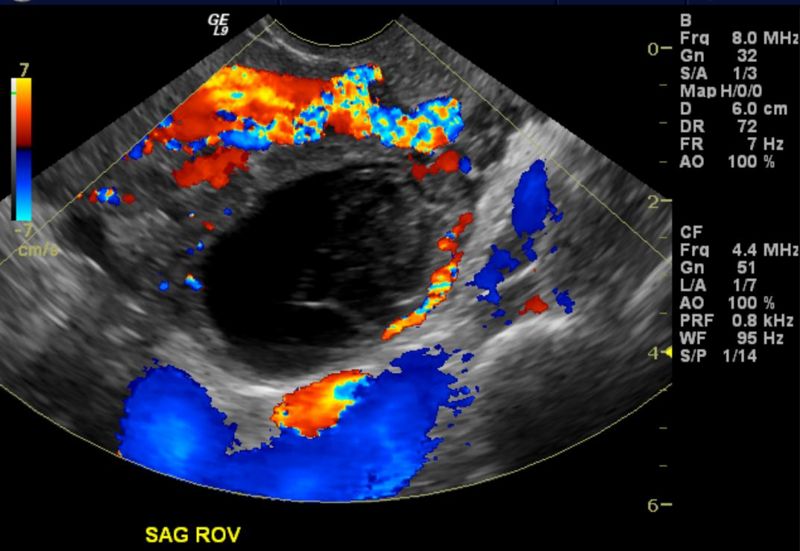
Dermoid cysts, though rare and typically noncancerous, are unique due to their varied tissue content. Their progressive expansion over time means that even if initially asymptomatic, they can eventually exert enough pressure to cause significant discomfort. Diagnostic imaging, such as ultrasounds or MRIs, is essential for confirming their presence and monitoring their growth.
Endometriomas, also known as “chocolate cysts,” are another type strongly linked to back pain, particularly because they are a manifestation of endometriosis. These cysts form when endometrial tissue grows within the ovary, leading to cyclical bleeding and inflammation inside the cyst. Over time, these repeated bleeding episodes cause the cysts to grow, increasing the likelihood of pressure-related discomfort, including lower back pain.
While endometriomas are benign, they can be quite painful and complex to manage, often indicating a more severe stage of endometriosis. Early detection through imaging is critical not only for alleviating symptoms but also for preventing potential complications, which may include impacts on fertility. The cyclical nature of the pain they cause can also be a distinguishing characteristic.
6. **Symptoms of Ovarian Cysts Beyond Back Pain**While lower back discomfort is a prominent concern, ovarian cysts can manifest through a wider array of symptoms that significantly impact a woman’s daily life. These signs often vary considerably, influenced by the cyst’s size, its specific type, and its precise location within the pelvic cavity. Recognizing this broader spectrum of symptoms is crucial for individuals to seek timely medical attention and ensure an accurate diagnosis.
One of the most frequent symptoms is persistent pelvic pain, which can present as a dull ache or, at times, a sharper, more intense sensation. This discomfort is typically localized to one side of the lower abdomen and can notably intensify during menstruation. Larger cysts can also exert considerable pressure on surrounding organs, leading to a distinct sensation of heaviness or fullness within the pelvic region due to the cyst’s physical presence.
Bloating, characterized by abdominal swelling or discomfort in the lower abdomen, is another common indicator that often mimics conditions like irritable bowel syndrome (IBS). This symptom can arise from fluid retention or the sheer physical volume that a significant cyst occupies within the abdominal cavity. Distinguishing cyst-related bloating from other causes requires careful evaluation.
Beyond general discomfort, ovarian cysts can also interfere with normal urinary and bowel functions, creating additional challenges. Urinary urgency or increased frequency, alongside difficulty emptying the bladder, may develop when a cyst presses directly against the bladder, irritating it and reducing its functional capacity.
Similarly, bowel issues, such as constipation, can emerge if an enlarged cyst compresses the rectum or intestines. This physical obstruction can impede the smooth passage of waste through the digestive tract, resulting in discomfort and irregular bowel habits. Differentiating these symptoms from those of other conditions like urinary tract infections or kidney stones is vital for accurate treatment.
Read more about: Unlock Your Morning: Physical Therapists Reveal 12 Simple Stretches to Conquer Lower Back Pain for Good
7. **Broader Causes of Ovarian Cysts Beyond Functional/Non-Functional**While functional and non-functional cysts represent common classifications, several underlying medical conditions can also contribute to the development of ovarian cysts, or cause existing ones to behave abnormally and become painful. Understanding these broader causes is essential for a comprehensive diagnostic approach and tailoring effective management strategies. These conditions not only trigger cyst formation but can also significantly impact fertility and hormone regulation.
Pelvic infections, for instance, can sometimes lead to the development of ovarian cysts, especially abscesses within the pelvis. An infected cyst carries an elevated risk of rupturing, which could potentially trigger sepsis—a severe, life-threatening immune response to harmful bacteria entering the bloodstream. Patients diagnosed with an infected ovarian cyst frequently require hospitalization and surgical intervention to drain and remove the infection, underscoring the seriousness of such complications.
Endometriosis is another significant cause of a specific type of ovarian cyst known as an endometrioma, or “chocolate cyst.” This condition involves the growth of endometrial tissue—the tissue that normally lines the uterus—outside of the uterine cavity. When this tissue grows within the ovary, it forms blood-filled cysts that can lead to acute pelvic pain and, unfortunately, can also affect fertility. The presence of endometriomas often indicates a more advanced stage of endometriosis, necessitating prompt medical attention for removal and management.
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder characterized by the presence of numerous small, harmless cysts that develop across the ovaries. These cysts, which typically contain undeveloped eggs that the body fails to release during menstruation, contribute directly to the irregular periods commonly experienced by women with PCOS. Beyond cysts, individuals with PCOS often exhibit elevated levels of androgen hormones, which can manifest as excess body hair or more frequent acne breakouts.
Understanding these multifaceted origins provides a clearer picture of why ovarian cysts can develop and become problematic. It emphasizes that while some cysts are a natural part of the menstrual cycle, others may signal underlying health issues that require specific medical diagnosis and intervention. A thorough evaluation by a healthcare provider can help discern the root cause and guide the most appropriate course of action.
8. **Factors Triggering Significant Ovarian Cyst Pain**While many ovarian cysts remain asymptomatic or cause only mild discomfort, certain factors can escalate their impact, leading to significant and even severe pain. Identifying these triggers is crucial for understanding when a cyst requires more urgent medical attention and intervention. The intensity and nature of the pain often provide important clues regarding the cyst’s behavior and potential complications.
One primary factor is the cyst’s sheer size and the pressure it exerts on surrounding structures. When cysts grow larger than 10 cm, their increased mass can begin to compress nearby organs and tissues, including sensitive pelvic nerves like the sciatic nerves or the ureters. This persistent compression often results in pain that radiates into the lower back, potentially becoming chronic and debilitating.
This significant pressure can also lead to secondary complications, such as urinary retention if the bladder is heavily compressed, or chronic constipation if the intestines are affected. Monitoring symptoms like persistent pelvic fullness or bloating can help identify problematic cysts early. Early detection through advanced imaging techniques, such as MRI, is often crucial in preventing these more severe, long-term issues.
A more acute and severe form of pain arises when a cyst ruptures. This occurs when the cyst bursts, releasing its contents—which may include fluid or blood—into the abdominal cavity. A ruptured cyst typically causes sudden, sharp pain in the lower abdomen or back, often accompanied by alarming symptoms such as dizziness, fever, or nausea. Such an event mimics other emergency conditions like appendicitis or ectopic pregnancy, demanding immediate medical attention.
Ovarian torsion is another serious complication where a cyst’s presence causes the ovary itself to twist around its supporting ligaments. This twisting can cut off the blood supply to the ovary, leading to intense, sudden pain. If not addressed promptly, ovarian torsion can result in tissue damage or loss of the ovary. Both ruptured cysts and ovarian torsion represent medical emergencies, underscoring the importance of swift diagnosis and potential surgical intervention.
9. **Home Remedies for Managing Ovarian Cyst Discomfort**For mild to moderate ovarian cyst discomfort, home remedies can offer temporary relief while awaiting medical evaluation or as part of a conservative management plan. It is important to remember that these strategies are aimed at symptom alleviation and do not replace professional medical treatment, especially for persistent or severe symptoms. These approaches can significantly improve comfort levels.
Over-the-counter (OTC) pain relief medications are often the first line of defense against discomfort. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen are particularly effective, reducing both pain and cyst-associated inflammation. A typical dosage might be 400 mg every six to eight hours as needed, but always follow package instructions or a healthcare provider’s advice.
While using pain relievers, it is also advisable to avoid strenuous activities like heavy lifting or intense exercise. Such activities can potentially increase abdominal pressure, which might heighten the risk of cyst rupture. Instead, opting for gentle movements such as walking or light stretching can maintain mobility without placing undue stress on the body, promoting a sense of well-being.
Applying heat therapy to the affected area is another widely recommended home remedy for easing discomfort. Placing a heating pad or a warm compress on the lower back or abdomen for approximately 15 to 20 minutes hourly can significantly improve blood flow to the region and help relax tense muscles. This warmth is particularly effective in soothing the dull, achy pain commonly associated with ovarian cysts.
Incorporating gentle yoga poses, such as child’s pose or cat-cow, can further aid in alleviating tension and promoting relaxation without overstraining the body. These stretches are designed to gently open the hip and pelvic areas, potentially easing some of the pressure-related discomfort. Always ensure that any physical activity, including stretching, is comfortable and does not exacerbate the pain.
10. **Comprehensive Medical Treatment Options for Ovarian Cysts**When ovarian cysts cause persistent discomfort, grow significantly, or present a risk of complications, medical intervention becomes necessary. Treatment approaches are highly individualized, depending on factors like cyst size, type, symptom severity, and the patient’s overall health. A collaborative discussion with a healthcare provider is essential to determine the most appropriate action.
For small, asymptomatic cysts, a common initial strategy is “watchful waiting.” This conservative approach involves regularly monitoring the cyst through periodic ultrasounds, typically every three months, to track any changes in size or characteristics. Given that most functional cysts resolve spontaneously within a few menstrual cycles, watchful waiting allows natural healing while ensuring no concerning developments are overlooked. During this period, over-the-counter pain relievers can be used for any mild discomfort, and avoiding strenuous activities can help minimize complication risks.
Hormonal treatments, notably birth control pills, offer an effective method for managing and preventing the formation of new functional cysts. Combined oral contraceptives work by suppressing ovulation, which directly reduces the likelihood of functional cysts developing. For endometriomas, GnRH agonists may be prescribed to manage symptoms by inducing a temporary menopausal state, shrinking endometrial tissue. These hormonal therapies regulate the menstrual cycle and mitigate cyst-related issues.
When cysts are large, persist over several cycles, or cause significant pain and other complications, surgical removal may be recommended. The two primary surgical procedures are laparoscopy, a minimally invasive outpatient procedure with quicker recovery, and laparotomy, an open abdominal surgery for complex cases or suspected malignancy. For younger patients or those planning future pregnancies, a cystectomy removes only the cyst while preserving ovarian tissue.
In severe instances, an oophorectomy, the removal of the affected ovary, might be required, particularly if the cyst is very large, recurrent, or cancerous. Recovery times vary significantly depending on the type of surgery performed, with laparoscopy typically allowing for a quicker return to daily activities compared to a laparotomy.
11. **Recognizing When to Seek Immediate Medical Attention**While many ovarian cysts resolve without incident, recognizing warning signs that necessitate immediate medical attention is critically important. Delaying care can lead to severe complications, underscoring the importance of timely intervention. Understanding these urgent indicators can make a profound difference in health outcomes and overall well-being.
A ruptured cyst often presents with a sudden onset of sharp, intense pain localized in the lower abdomen or back. This acute pain may be accompanied by other concerning symptoms such as dizziness, fever, or persistent nausea and vomiting. If any of these symptoms appear rapidly, it is imperative to seek emergency medical care without delay, as a ruptured cyst can lead to internal bleeding or infection.
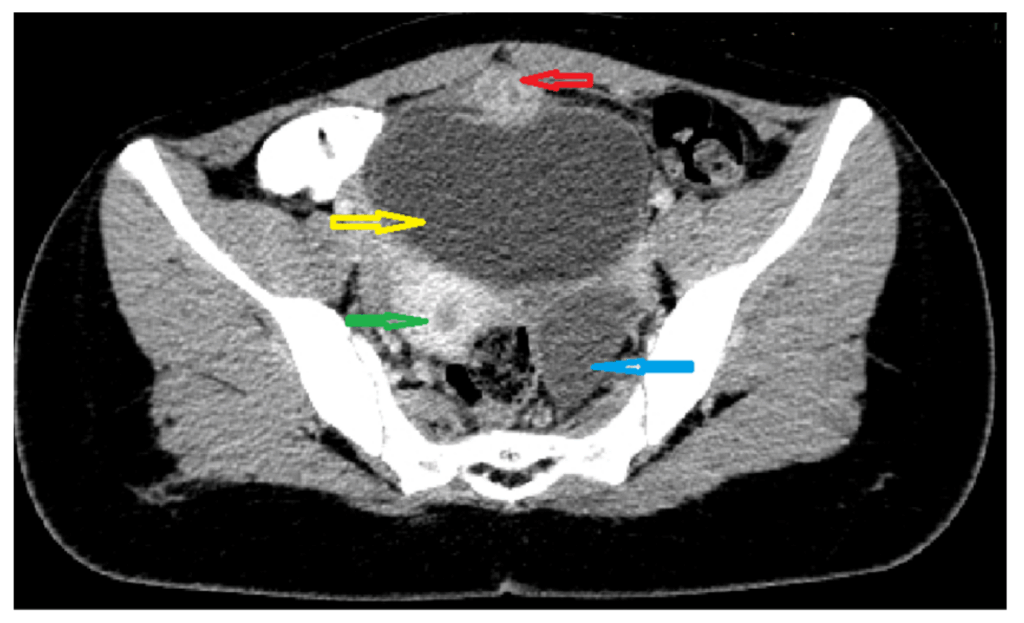
Upon presentation to a medical facility, diagnostic steps typically include a pelvic exam and ultrasound to confirm the rupture and assess any associated bleeding. In certain cases, a CT scan may also be utilized to gain a more detailed view of the abdominal cavity. For postmenopausal patients, a CA-125 blood test might be conducted to rule out potential malignancy, given that symptoms can sometimes overlap.
Beyond a ruptured cyst, several other symptoms signal a medical emergency. These include a fever above 38°C (100.4°F), severe vaginal bleeding heavier than a typical menstrual period, or symptoms indicative of hypotension, such as lightheadedness, weakness, or fainting. Internal bleeding, a serious complication, may manifest as unusually pale skin, a rapid heart rate (tachycardia), or episodes of syncope (fainting).
For situations where such severe symptoms are experienced, immediate emergency medical services should be contacted without hesitation. While less severe symptoms warrant scheduling an appointment with a general practitioner, the presence of sudden, incapacitating pain accompanied by vomiting or fainting necessitates an immediate visit to the emergency room. Rapid response to these critical indicators is crucial for preventing life-threatening outcomes and preserving reproductive health.
Read more about: Beyond the Cough: 14 Critical Lung Infection Warning Signs You Should Never Ignore, Including Unexpected Clues on Your Fingernails
Navigating the landscape of ovarian cysts can feel daunting, yet armed with knowledge and a proactive approach, women can confidently manage their health. While these fluid-filled sacs are often benign and transient, recognizing the nuances of their presentation—from the subtle ache in the lower back to more urgent indicators—empowers us all. This journey of understanding reinforces the profound connection between our bodies’ signals and the importance of professional guidance. Embrace this knowledge, champion your well-being, and remember that informed vigilance is your greatest ally in maintaining optimal reproductive health, ensuring a future where you can thrive beyond the bloat and discomfort.


