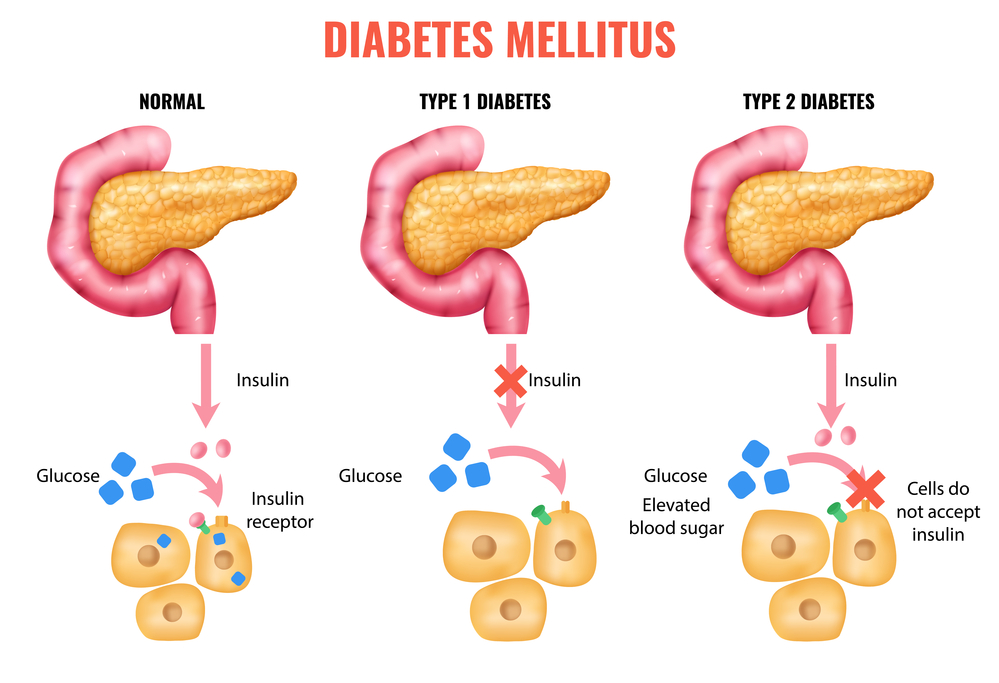
It’s well known that diabetes raises your blood sugar levels, but this chronic health condition also dramatically increases your risk for a variety of serious eye diseases that can unfortunately lead to blindness. As Johns Hopkins diabetes expert Rita Rastogi Kalyani, M.D., M.H.S., succinctly puts it, “Elevated blood sugar levels can damage blood vessels in the retina—the area at the back of the eye that sends signals to your brain.” This fundamental damage, known as diabetic retinopathy, can silently begin its insidious work years before you ever notice the slightest change in your vision, making early awareness and proactive monitoring absolutely critical for preserving your eyesight.
Indeed, diabetic retinopathy stands as the leading cause of new cases of reversible blindness in the United States, a stark reality that underscores the profound impact diabetes can have on ocular health. The National Institutes of Health’s National Eye Institute reports that a staggering 40 percent of people with diabetes already have some degree of retinopathy. Beyond this, diabetes escalates your risk for cataracts—a condition that causes the clear lens of the eye to become cloudy, blocking out light—by a significant 60 percent, and it raises your odds for developing glaucoma—pressure that damages the optic nerve—by a concerning 40 percent. These aren’t just statistics; they represent potential challenges to your daily life, from reading to driving, and truly emphasize the need to understand these conditions.
Navigating the complexities of diabetes means understanding all its potential ramifications, and vision health is undoubtedly a cornerstone of that understanding. Many people are unaware of these specific ocular risks, which creates a critical “knowledge gap” that could increase the risk of blindness if early eye checks and vision-protecting treatments are missed, according to a recent Johns Hopkins study. This article aims to bridge that gap, shedding light on the essential diabetes-related eye indicators you should never ignore. We’ll explore some of the most common and serious eye conditions associated with diabetes, detail the initial, often temporary, vision changes you might experience, and empower you with the knowledge to recognize these signs and protect your precious sight.

1. **Diabetic Retinopathy (DR): The Leading Cause of Vision Loss**Diabetic retinopathy (DR) is arguably the most recognized and impactful eye complication of diabetes, holding the unfortunate title of the leading cause of blindness in working-age adults. This condition arises when persistently high blood sugar levels wreak havoc on the delicate blood vessels situated within the retina, which is a crucial part of your eye responsible for sending visual signals to your brain. When these blood vessels are compromised, they can swell and leak fluid, leading to blurry vision and other severe impairments. It’s important to understand that DR typically affects both eyes, signifying a systemic impact of diabetes on your visual system.
Anyone living with type 1, type 2, or gestational diabetes (diabetes experienced during pregnancy) is susceptible to developing DR. The duration of your diabetes diagnosis plays a significant role, with the likelihood of developing DR increasing the longer you have the condition. Beyond the foundational presence of diabetes, several other factors can significantly elevate your risk. These include poorly controlled high blood sugar, elevated blood pressure, and high cholesterol levels, all of which contribute to vascular damage throughout the body, including the eyes. Smoking is another powerful risk factor, as it further compromises blood vessel health and accelerates damage. Furthermore, certain demographic groups, specifically African American, Hispanic/Latino, or American Indian or Alaska Native individuals, face an increased predisposition to developing DR, highlighting the complex interplay of genetics and environmental factors.
Diabetic retinopathy progresses through distinct stages, each carrying its own set of visual implications. The initial phase is known as the early stage, or nonproliferative DR. During this stage, the blood vessels within the retina begin to weaken and develop bulges, forming tiny pouches that are medically referred to as microaneurysms. These pouches are prone to leaking fluid, and if this leakage occurs in a specific part of the retina called the macula, it can cause significant swelling and distortion of your vision. This critical swelling is known as macular edema, and it stands as the most common cause of blindness among individuals with DR, affecting approximately half of all people diagnosed with the condition. Early detection in this stage is vital because the damage can begin silently, long before noticeable symptoms emerge, emphasizing the importance of regular eye exams even when your vision seems fine.
The condition can escalate to an advanced stage, referred to as proliferative DR (PDR), which marks a more severe progression of the disease. In this advanced phase, the retina attempts to compensate for the damaged and blocked blood vessels by growing new ones. However, these newly formed blood vessels are often fragile, abnormal, and highly prone to bleeding. When minor bleeding occurs, you might notice small, dark spots or floaters in your vision, which can be unsettling. Should more substantial bleeding take place, it can lead to a vitreous hemorrhage, causing your vision to be partially or even completely blocked. This stage represents a critical juncture where the potential for severe, irreversible vision loss significantly increases, making prompt and aggressive treatment essential to prevent further deterioration and protect the remaining sight.

2. **Diabetic Macular Edema (DME): The Swelling Threat to Your Central Vision**Diabetic Macular Edema (DME) is a serious complication often associated with diabetic retinopathy, representing a direct and significant threat to your central vision. The macula is a small but incredibly vital part of your retina, responsible for your sharp, detailed central vision—the kind you use for reading, recognizing faces, and performing any task that requires fine visual acuity. When the damaged blood vessels in the retina, a hallmark of diabetic retinopathy, begin to leak fluid into the macula, it causes this crucial area to swell. This swelling is precisely what we define as macular edema, and it can profoundly distort and blur your vision, making everyday activities incredibly challenging.
As noted by Rita Rastogi Kalyani, M.D., M.H.S., “Elevated blood sugar levels can damage blood vessels in the retina… This damage, called diabetic retinopathy, can begin years before you notice vision changes.” This initial damage often sets the stage for DME. The development of macular edema is particularly concerning because it is the most common cause of blindness in people already suffering from diabetic retinopathy. Approximately half of all individuals who develop DR will, at some point, also experience macular edema. This highlights the intertwined nature of these conditions and the added urgency of managing diabetes to protect both peripheral and central vision.
The symptoms of DME often overlap with those of diabetic retinopathy, making early diagnosis through a comprehensive eye exam paramount. While you may not notice symptoms in the very early stages, as the macula swells, you might experience blurry vision, spots or dark shapes floating in your vision, difficulty distinguishing colors, or even dark or empty areas in your overall visual field. The insidious nature of DME, like DR, means it can progress silently before noticeable symptoms become alarming. This makes routine, dilated eye exams an indispensable tool, allowing your doctor to identify signs of fluid leakage or swelling in the macula before permanent damage takes hold. Early detection provides the best opportunity for effective treatment to repair damage and prevent profound vision loss.

3. **Cataracts and Diabetes: Why Your Lens Might Cloud Sooner**A cataract is fundamentally the clouding of the eye’s normally clear lens. While it’s a natural part of aging for everyone, people living with diabetes face a significantly higher risk of developing cataracts, and often at a much younger age than their non-diabetic counterparts. This accelerated development isn’t just a coincidence; it’s a direct consequence of the metabolic changes brought about by diabetes. One primary reason for this heightened risk is that persistently high blood sugar levels can lead to the accumulation of deposits within the lens of the eye, causing it to become progressively cloudy and obstruct the passage of light, leading to blurry or hazy vision.
In fact, diabetes increases your risk for cataracts by a substantial 60 percent. This statistic alone underscores the importance of considering cataracts as another serious eye complication of diabetes. Beyond high blood sugar, other risk factors can further contribute to cataract development in people with diabetes. These include high blood pressure, obesity, prolonged exposure to sunlight without adequate protection, and smoking. Each of these factors, especially when combined with diabetes, creates an environment conducive to earlier and more severe lens opacification, emphasizing the holistic nature of diabetes management in protecting overall eye health.
Symptoms of cataracts, particularly in their early stages, can be subtle and easily overlooked. However, as the clouding progresses, you might notice a gradual blurring or dimming of your vision, making everything appear hazy or less vibrant. You may also experience increased sensitivity to light and glare, especially from headlights at night, or difficulty seeing in low light conditions. Colors might seem faded, and you might even experience double vision in one eye. While surgery is the only definitive way to treat cataracts by replacing the cloudy lens with an artificial one, it’s usually not required immediately unless the vision loss begins to significantly interfere with your daily activities. In the interim, simple adjustments like using brighter lights at home and wearing anti-glare sunglasses outdoors can provide some relief, but a conversation with your eye doctor is crucial to determine the best course of action and timing for treatment. Most people experience significantly improved vision after successful cataract surgery.

4. **Glaucoma: The Silent Pressure Damaging Your Optic Nerve**Glaucoma refers to a group of complex eye diseases that share a common, devastating outcome: damage to the optic nerve. This damage most frequently occurs due to excessively high pressure inside the eye, known as intraocular pressure (IOP). What makes glaucoma particularly insidious is its silent progression; many types of glaucoma exhibit no noticeable symptoms in their early stages, allowing vision loss to occur slowly and often imperceptibly over time. This lack of early warning signs makes regular eye exams exceptionally critical for individuals at risk, especially those with diabetes.
People with diabetes are unfortunately twice as likely to develop open-angle glaucoma, which is the most common form of this disease. This increased susceptibility highlights yet another way diabetes compromises ocular health. Beyond diabetes, there are several other significant risk factors for open-angle glaucoma, including having a family history of the condition, being over the age of 60, and belonging to certain ethnic groups such as African American, Asian, or Hispanic/Latino persons. These factors, combined with diabetes, elevate the need for vigilant screening and monitoring to catch the disease before irreversible vision loss occurs. The insidious nature of glaucoma means that by the time you notice vision changes, some permanent damage to the optic nerve may have already taken place.
Diabetes can also lead to a more aggressive and challenging form of glaucoma called neovascular glaucoma. This specific type sometimes develops as a complication of advanced diabetic retinopathy, when new and abnormal blood vessels—a consequence of severe retinal ischemia—begin to grow on the iris, which is the colored part of the eye. These fragile new vessels can obstruct the natural flow of fluid out of the eye, causing a rapid and significant increase in intraocular pressure. This form of glaucoma can be particularly damaging and harder to manage, underscoring the severe repercussions of uncontrolled diabetes on the intricate vascular system of the eye. Early and aggressive management of diabetic retinopathy is crucial to prevent the development of such severe complications.
While there is currently no known way to completely prevent glaucoma, the good news is that timely treatment can be highly effective in preventing it from worsening and preserving remaining vision. This is precisely why catching glaucoma early is so incredibly important. Treatment options typically include a range of approaches such as specific eye drops or oral medicines to lower eye pressure, various laser treatments, and in some cases, surgical procedures to improve fluid drainage or reduce fluid production. Discussing the most suitable treatment choices with your eye doctor is essential for developing a personalized management plan aimed at stabilizing intraocular pressure and protecting the optic nerve from further damage, thereby safeguarding your vision as much as possible.

5. **Temporary Vision Changes: Understanding the Initial Blurriness at Diagnosis**For many individuals, vision changes can be one of the surprising initial indicators of diabetes or a clear sign whenever blood sugar levels become poorly controlled. These fluctuations in vision are often temporary, but they can be quite alarming, particularly for those who are not yet familiar with the profound effects that high blood sugar can have on the intricate mechanisms of the eyes. Understanding these early, transient shifts in vision is crucial for newly diagnosed individuals or those experiencing periods of glycemic instability, as it helps differentiate them from more permanent, damaging eye diseases like retinopathy or glaucoma.
One of the most common early changes people notice is a distinct blurriness in their vision. This phenomenon is directly caused by the fluctuating nature of blood sugar levels, which have a tangible impact on the shape and function of the eye’s lens. When blood sugar levels are elevated, the lens in the eye tends to swell due to fluid shifts, altering its ability to accurately focus light onto the retina. This temporary change in the lens’s refractive power is what leads to the experience of blurred vision. Conversely, as blood sugar levels begin to drop—a common occurrence when treatment with insulin or other glucose-lowering medications is initiated—the lens gradually returns to its normal shape. This adjustment process can, somewhat counter-intuitively, cause another period of temporary blurriness as the eyes adapt to the normalizing glucose environment, a transition that can take several weeks to stabilize.
Interestingly, some people report a sudden, unexpected improvement in their distance vision even before they receive a formal diagnosis of diabetes. This peculiar phenomenon occurs because the abnormal swelling of the lens temporarily alters how light is refracted within the eye, sometimes reducing the need for previously worn corrective lenses. However, this seemingly positive change is, in fact, a misleading symptom of underlying high blood sugar. Once diabetes treatment commences and blood sugar levels begin to normalize, this lens swelling diminishes, and vision can blur once again. This often frustrates individuals who had initially believed their eyesight had permanently improved, highlighting the deceptive nature of uncontrolled diabetes and its effects on vision.
This adjustment period, where vision fluctuates as blood sugar stabilizes, can typically last for about three to four weeks. It is sometimes accompanied by mild headaches as the eyes work to adapt to the changing refractive state. While these temporary vision changes can undoubtedly be unsettling and uncomfortable, it is important to remember that they are rarely indicative of permanent damage to the eyes themselves. Instead, they serve as a clear physiological response to the metabolic shifts occurring within the body. If blurred vision persists after starting diabetes treatment, an eye exam can help confirm that the issue is indeed due to fluctuating blood sugar, rather than the onset of diabetic eye disease, offering reassurance and guiding appropriate management strategies. During this adjustment period, practical solutions like using over-the-counter reading glasses can offer temporary relief, allowing individuals to manage their vision while their blood sugar levels stabilize, but it’s crucial to avoid investing in new prescription lenses during these fluctuations, as they will likely become ineffective once glucose levels regulate. Early blood sugar control is the best way to prevent long-term vision loss, even when temporary changes are occurring. This holistic approach empowers you to confidently manage your eye health and protect your sight for years to come.

6. **Your Eye Exam: Laying the Foundation for Diabetes Vision Care**For anyone managing diabetes, a comprehensive eye examination isn’t just a routine check-up; it’s a critical cornerstone of preventing severe vision loss. These detailed evaluations detect the often-silent impact of diabetes on your ocular health, including diabetes-related retinal disease (DRD), diabetic macular edema (DME), glaucoma, and cataracts. The sooner these conditions are detected, the more likely you are to prevent or delay vision loss. Your eye doctor, whether an optometrist or ophthalmologist, conducts a series of tests that can take between one to three hours, ensuring every crucial aspect of your eye health is assessed.
The most important aspect of any medical evaluation, including ocular assessments for people with diabetes, is the history obtained from the patient. During this initial phase, your eye care professional delves into your diabetes journey. Understanding the duration of your diabetes, your current medications, glycemic stability, and A1C targets provides vital insights into your potential for developing DRD. Establishing a timeline of any visual changes helps direct the examination, determine treatment timing, and schedule follow-up appointments.
Following your medical history, your visual acuity is meticulously measured. This checks the best uncorrected and corrected vision in each eye, at both distance and up close, typically using an eye chart. Pinholes or formal refraction determine any refractive error and the best possible visual acuity with new lenses. Achieving 20/20 vision means you discern the same optotypes at 20 feet as a person with ideal vision. Dramatic fluctuations in blood glucose levels can cause vision changes, sometimes indicating diabetes for eye care professionals.
Another fundamental part of the examination involves pupil assessment. These are evaluated in both dark- and light-adapted states to observe reactivity, size, and shape symmetry. A significant difference in size (>0.4 mm) between the two pupils is anisocoria. The swinging flashlight test assesses for a relative afferent pupillary defect, analyzing optic nerve functionality. Pupil abnormalities are common in individuals with diabetes, often due to diabetes-related autonomic neuropathy and ocular ischemia, which can impair proper pupil dilation or light reaction.
7. **Beyond the Basics: Key Tests for Deeper Insights into Diabetic Eye Health**Beyond foundational assessments, a comprehensive eye exam delves into critical areas to uncover potential damage. Intraocular pressure (IOP), the fluid pressure inside your eye, is a vital measurement. Taken after topical anesthetic, by gently placing an applanator on the cornea, normal IOP is 12-22 mmHg. Elevated IOP signals glaucoma; diabetes and DRD modestly increase this risk. A detailed optic nerve examination during ophthalmoscopy, plus specialized testing, may be necessary.
Your eye care professional also meticulously evaluates your visual fields—the entire view perceived by each eye when looking straight ahead. Confrontation visual field testing grossly determines peripheral vision. While maintaining central fixation, you identify fingers in each quadrant’s periphery. If acuity is poor, the test might involve noting hand movement or light. Areas of decreased or lost vision appear as darkened regions.
Automated testing offers more precise evaluation, assessing points for central 10°, 24°, or 30° visual fields. For poorly attentive individuals or those with vision <20/200, a Goldmann visual field test maps the field while ensuring attention. For people with diabetes, visual field testing is useful for evaluating central macula and optic nerve function, and for glaucoma monitoring. Repeated testing determines disease stability or progression.
The external examination of the eye provides important clues. Abnormalities in eyelid position, symmetry, or ocular alignment can indicate cranial nerve dysfunction. Ptosis (lower eyelid position) with eye deviation could signal a cranial nerve III palsy, sometimes a temporary consequence of hyperglycemia. Gross inspection of the sclera, conjunctiva, and iris offers further insights.
Inflamed or red conjunctiva may relate to diabetes-related keratopathy, a corneal disease from decreased sensitivity. This can lead to non-healing corneal ulcers. Careful iris inspection may reveal neovascularization of the iris (NVI), where new, abnormal blood vessels grow in response to retinal ischemia. NVI is associated with advanced proliferative DR (PDR) and can cause spontaneous hyphema and neovascular glaucoma, underscoring severe repercussions.

8. **Unveiling Damage: Advanced Imaging and Ophthalmoscopy in Diabetic Eye Exams**To gain the deepest understanding of your eye health, your eye care professional employs sophisticated tools, including the slit-lamp microscope and ophthalmoscopy. The slit-lamp examination uses a specialized microscope with adjustable light to magnify and evaluate three-dimensional ocular structures. This detailed inspection checks lids, lashes, lacrimal system, conjunctiva, sclera, and cornea for abnormalities, inflammation, or defects.
Using higher magnification, the examiner visualizes deeper structures: the anterior chamber, iris, lens, and anterior vitreous. The presence of red or white blood cells, neovascularization of the iris (NVI), and lens opacifications are important indicators in diabetes-related retinal disease (DRD). These findings help identify early or advanced stages of ocular complications.
Ophthalmoscopy, or fundoscopy, is crucial for determining DRD presence and level. After pupil dilation, an ophthalmoscope provides a highly magnified view of the posterior chamber: vitreous, retina, retinal blood vessels, and optic nerve. Optic nerve evaluation focuses on neovascularization, pallor, thinning, and optic cup-to-disc ratio, signaling damage or disease progression. Close evaluation of the macula, retinal vasculature, and periphery can reveal critical findings. These include retinal hemorrhages, microaneurysms, hard exudates, diabetic macular edema (DME), and retinal ischemia (cotton wool spots), along with advanced signs like neovascularization and vitreous hemorrhage. The specific appearance helps determine DRD stage.
Ocular imaging provides invaluable objective data. Fundus photography captures high-resolution photos of posterior structures for education, staging, and monitoring DRD. Fluorescein angiography documents retinal circulation, highlighting nonperfusion or new blood vessels. Optical coherence tomography (OCT) creates cross-sectional retinal images, crucial for documenting retinal thickness and DME. B-scan ultrasonography helps when direct posterior segment visualization is limited, detecting vitreous blood, fibrosis, or detached retina. These techniques empower professionals to classify disease and tailor effective treatments.

9. **Navigating Life with Diabetes: Practical Vision Impairment Solutions**Living with diabetes and vision impairment can feel daunting, but effective management is entirely achievable with the right tools. These practical solutions empower you to maintain health control, ensuring accurate blood glucose monitoring, medication administration, and safe adherence to medical instructions. Adapt your environment and tools to compensate for vision changes, allowing confident continuation of essential self-care routines.
Improve your environment through “lighting the way” and using magnifying equipment. Low vision significantly affects checking blood glucose, giving injections, and reading medical instructions. A bright lamp with magnifying tools is incredibly helpful. A syringe magnifier attached to the insulin vial makes seeing the dosing line easier, ensuring accurate administration. Standing magnifying glasses keep hands free for device manipulation.
Choosing the right blood glucose monitor is paramount. Look for devices prioritizing accessibility, such as those with larger, tactile buttons and high-contrast coloring. Talking blood glucose meters audibly guide you through checking levels and provide vocal results. Select models with volume control and an external port for headphones for discreet testing. Test devices thoroughly for ease of setup and use, as some users find certain models overly complicated.
Administering insulin with pre-filled pens requires extra caution if visually impaired. Different strengths mean incorrect usage can have serious health consequences. For safety, especially when starting a new product or dose, have someone with good vision assist you. If using multiple insulin types, seek products with different colors or distinct tactile markings on plunger buttons to prevent errors.
Finally, ensure access to and review of healthcare information. Websites or information sheets are ineffective if unreadable. Ask a trusted companion to appointments to take notes. Request an exam report be sent to your primary care provider/endocrinologist and keep a copy. Recording conversations with healthcare providers is immensely beneficial, allowing re-listening to advice and reinforcing understanding.

10. **Your Vision, Your Control: Proactive Steps Against Diabetes-Related Eye Loss**While diabetes can significantly impact your vision, you possess considerable power to prevent or delay long-term vision loss. Proactive, diligent management of your diabetes is the most effective defense against eye complication progression. Consistently implementing key preventive strategies reduces your risk for severe eye diseases like diabetic retinopathy, glaucoma, and cataracts. This safeguards your sight through informed choices and collaboration with your healthcare team.
A cornerstone of preventing diabetes-related eye disease is maintaining optimal blood glucose levels. The American Diabetes Association (ADA) recommends an A1C target of less than 7% for most people with diabetes. Achieving this goal can significantly reduce microvascular complications, including eye disease, by up to 25 percent. This involves working with your doctor, following a healthy eating plan, regular physical activity, and consistently taking prescribed medications. These steps prevent high blood sugar that damages delicate eye blood vessels.
Beyond blood glucose, controlling your blood pressure is another critical factor. High blood pressure further compounds damage to tiny blood vessels in your eyes, escalating vision loss risk. Therefore, follow doctor-recommended steps to manage and control your blood pressure. This proactive measure protects ocular health and contributes to overall cardiovascular well-being, highlighting the holistic nature of diabetes management. Effective blood pressure control is a powerful ally against diabetes-related eye complications.
Regular, dilated eye exams are non-negotiable for proactive prevention. The ADA recommends an annual dilated eye exam, performed by an experienced ophthalmologist or optometrist. These exams reveal eye changes early, often before symptoms appear. As Rita Rastogi Kalyani, M.D., M.H.S., explains, “Early detection gives you time for treatments, such as laser therapy, that can protect your eyes.” She adds, “It also gives you more time to protect your vision by controlling blood sugar and blood pressure.” Consistent monitoring is your best chance for early intervention.
Finally, a simple yet profoundly impactful proactive step is to stop smoking. Tobacco use is a well-established risk factor that significantly adds to eye damage, compromising blood vessel health and accelerating diabetes-related eye disease progression. Eliminating smoking is one of the most powerful actions you can take to protect your vision and overall health. By embracing these diligent management strategies—optimal blood sugar control, blood pressure management, regular comprehensive eye exams, and avoiding tobacco—you empower yourself to confidently manage your eye health and protect your precious sight for many years to come.
As we’ve journeyed through the intricate ways diabetes can impact your vision, from initial blurriness to the serious threats of retinopathy, macular edema, cataracts, and glaucoma, one truth remains clear: knowledge is power, and proactive care is paramount. Your eyes are windows to the world; protecting them with diabetes is an ongoing, vital commitment. By understanding the signs, embracing regular, comprehensive eye exams, and diligently managing your blood sugar, blood pressure, and overall health, you’re not just reacting to a condition. You’re actively shaping a future where your vision remains clear, vibrant, and capable of capturing all of life’s beauty. Let these insights guide you, empowering you to work hand-in-hand with your healthcare team and steadfastly protect your most precious sense of sight.