
Obstructive Sleep Apnea (OSA) is far more than just loud snoring or feeling a bit tired during the day. It’s a serious and widespread sleep disorder that silently disrupts breathing patterns, lowers vital oxygen levels, and, in doing so, can profoundly impact nearly every aspect of your health, especially your mental well-being. While many people associate sleep apnea primarily with physical health risks like heart disease and diabetes, a growing body of evidence reveals its deep and often underestimated connection to mood disorders and cognitive function. Ignoring these subtle yet significant signs can have cumulative, long-lasting effects on your quality of life.
Millions of adults worldwide unknowingly grapple with OSA, a condition where throat muscles relax during sleep, leading to repeated interruptions in airflow. These brief cessations in breathing are jarring enough to rouse a person just enough to reopen their airway, but often so fleeting that the individual never remembers waking. This constant cycle of oxygen deprivation and sleep fragmentation takes a massive toll on the brain and body, setting the stage for a range of symptoms that extend far beyond the bedroom, often manifesting in unexpected ways, particularly in your mood and mental clarity. It is crucial to understand these indicators, as recognizing them is the first step toward effective treatment and regaining control over your health.
Navigating the complexities of sleep disorders requires a keen eye, much like detective work. Patients frequently focus on a few prominent symptoms while overlooking others they deem irrelevant. For clinicians and individuals alike, understanding the full spectrum of OSA’s presentation, especially its influence on mental and emotional states, is vital. This in-depth look will explore some of the most critical indicators of OSA, moving beyond the obvious to shed light on the serious impacts that often start within your mood and should never be ignored. We aim to simplify complex medical information, offering clear, evidence-based insights and actionable advice to empower you to take charge of your sleep and mental health.
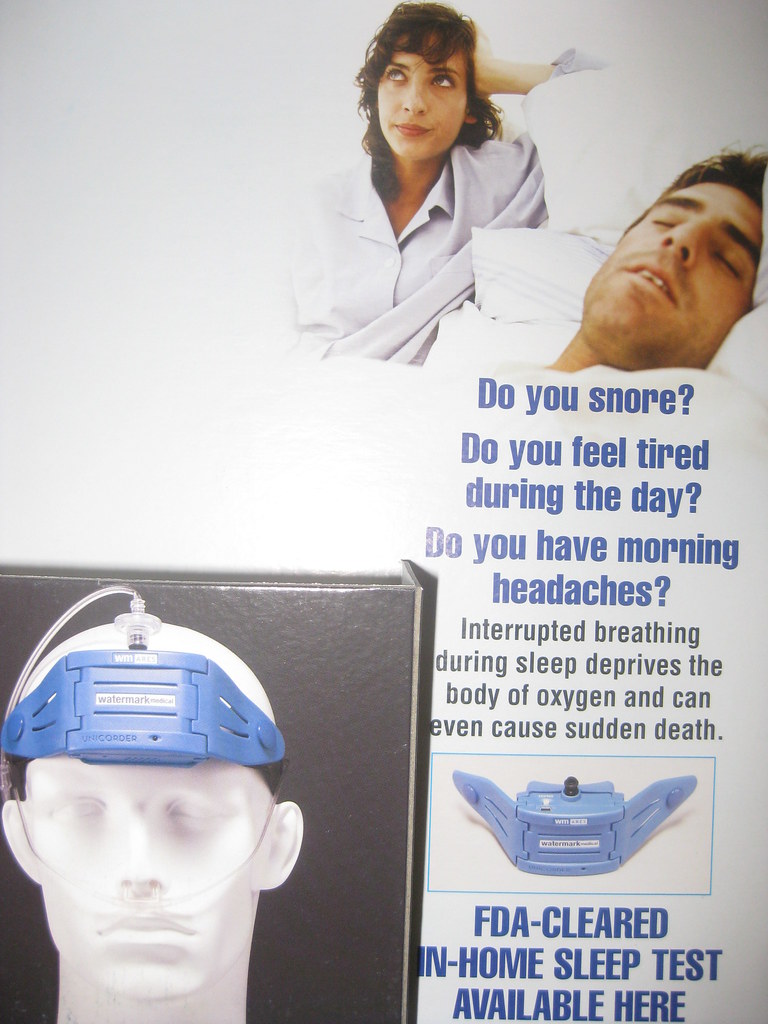
1. **Loud Snoring with Breathing Pauses**The most commonly recognized symptom, and often the first clue for partners, is loud snoring punctuated by distinct intervals where breathing ostensibly stops for a few seconds before resuming. This can sometimes sound like the individual is choking, a frightening experience for anyone witnessing it. While snoring itself isn’t always indicative of OSA, the characteristic pauses followed by gasps or chokes are a hallmark sign that should trigger immediate concern and professional evaluation.
These breathing cessations, known as apneic episodes, occur when the soft tissues in the airway relax and partially collapse, creating an obstruction. The cessation in airflow is startling enough to cause a partial awakening, which, despite not being remembered, profoundly disrupts the natural sleep cycle. Patients with mild OSA may experience between five and ten such episodes per hour, while severe cases can see over 30 episodes per hour, transforming a night’s rest into a continuous struggle for breath.
This chronic disruption means the body and brain are not getting the restorative sleep they desperately need. The intermittent lack of oxygen and repeated micro-arousals trigger a stress response, flooding the body with adrenaline even during sleep. This ongoing cycle not only strains the cardiovascular system but also has direct implications for brain function and emotional regulation, setting the stage for many of the less obvious symptoms discussed below. Recognizing these breathing pauses is a critical first step in uncovering underlying sleep apnea.
Read more about: 12 Critical Warning Signs of Sleep Apnea You Can’t Afford to Ignore: A Comprehensive Guide to Understanding and Addressing This Silent Threat

2. **Excessive Daytime Sleepiness and Fatigue**Despite spending hours in bed, individuals with Obstructive Sleep Apnea frequently wake up feeling unrefreshed, sluggish, and profoundly tired. This leads to persistent, excessive daytime sleepiness and fatigue, which is often cited as the major and most distinctive symptom of OSA. It’s not just a feeling of being a bit sleepy; it’s an overwhelming urge to fall asleep during inappropriate times, often impacting daily activities, work performance, and overall safety.
This chronic exhaustion is a direct result of sleep fragmentation. Each apneic event, even if not consciously remembered, triggers a brief awakening that disrupts the crucial deep sleep and REM (rapid eye movement) stages essential for physical and mental restoration. When this cycle repeats dozens or even hundreds of times throughout the night, the body and brain are continually deprived of the restorative sleep they need, accumulating a significant sleep debt that manifests as debilitating daytime fatigue.
Many patients mistakenly attribute this chronic tiredness to demanding schedules, aging, or other health issues, overlooking the possibility of a sleep disorder. However, if you find yourself struggling to stay awake during meetings, while driving, or even during quiet activities, it’s a serious indicator that your sleep quality is severely compromised. Addressing this symptom is not just about feeling more energetic; it’s about protecting your cognitive function and preventing accidents, highlighting the urgent need for a proper diagnosis.
Read more about: Critical Depression Symptoms You Should Never Ignore: A Deep Dive into the Sleep-Depression Connection for Your Well-being
3. **Morning Headaches and Confusion**Waking up with a dull, throbbing headache or a feeling of mental fogginess is another common yet often dismissed indicator of Obstructive Sleep Apnea. These morning headaches and confusion are direct consequences of the physiological stress your body endures throughout the night due to intermittent oxygen deprivation and elevated carbon dioxide levels. As the brain attempts to compensate for these imbalances, it can lead to discomfort and impaired cognitive function upon waking.
During apneic episodes, the body experiences moments of hypoxia, where oxygen levels in the blood drop, and hypercapnia, where carbon dioxide levels rise. These changes affect blood flow to the brain and can trigger a cascade of events, including inflammation and cerebral small vessel disease. The brain, struggling under these conditions, often manifests its distress through a morning headache, which typically improves as the day progresses and normal breathing resumes.
Coupled with headaches, morning confusion or ‘brain fog’ is a pervasive symptom. The fragmented sleep prevents the brain from adequately clearing toxins, consolidating memories, and forming new neural pathways. This leaves individuals feeling disoriented, struggling to think clearly, and experiencing a diminished ability to concentrate immediately after waking. If your mornings consistently start with a clouded mind or persistent headaches, it’s a strong signal that your sleep quality is being severely compromised by an underlying issue like OSA.
Read more about: Unleash Your Inner Mechanic: 15 Essential DIY Car Hacks to Save a Fortune on Maintenance

4. **Depression**The link between Obstructive Sleep Apnea and depression is increasingly recognized as a critical, often overlooked, aspect of the disorder. Recent research has shown that OSA is an independent risk factor for depression, meaning it can contribute to or exacerbate depressive symptoms even in the absence of other risk factors. This connection is so strong that prevalence studies indicate as many as three in five people (63%) with sleep apnea are also clinically depressed, often experiencing high levels of daytime fatigue and sleepiness alongside their mood issues.
The chronic sleep disruption and intermittent oxygen deprivation caused by OSA have a profound impact on brain chemistry and function, directly affecting neurotransmitters like serotonin and dopamine, which play key roles in mood stabilization. The cumulative effect of regularly disrupted sleep, coupled with the body’s constant stress response, can lead to persistent feelings of sadness, hopelessness, irritability, and a general loss of interest in activities once enjoyed, all characteristic of depression.
Evidence-based studies underscore this correlation. A 2003 cross-sectional study involving almost 19,000 participants revealed that patients with major depressive disorder are five times more likely to have OSA. More recently, a 2023 study found that OSA patients are 1.36-fold more likely to experience depression, with the severity of OSA positively correlating with depressive symptoms. Thankfully, treatment for OSA, particularly with CPAP therapy, has shown significant improvements in mental health, with one study reporting a decrease in depressive symptoms in 96% of patients after just three months.
Read more about: Beyond Fatigue: Crucial Thyroid Disorder Symptoms You Should Never Overlook, Including Early Signs That Begin in Your Hair and Skin

5. **Anxiety**Just as OSA is closely linked to depression, it also has a significant association with anxiety disorders. Untreated sleep apnea can heighten stress hormone levels, creating a constant state of physiological alert that predisposes individuals to feelings of worry, nervousness, and panic. This often manifests as an increased likelihood of developing an anxiety disorder, with one study indicating that more than one in two people (54%) with OSA experience some degree of ongoing anxiety.
The underlying mechanisms contribute to this heightened anxiety. Sleep fragmentation, a hallmark of OSA, leads to increases in sympathetic nervous system activity and oxidative stress, both of which can amplify the body’s ‘fight or flight’ response. The repeated drops in oxygen levels throughout the night are perceived as a threat by the brain, triggering the release of stress hormones like cortisol. This chronic elevation of cortisol contributes to feelings of restlessness, irritability, and pervasive worry, making it difficult for individuals to relax even when awake.
For those with OSA, the anxiety can be multifaceted. Beyond the direct physiological impact, there’s often the subconscious stress of struggling to breathe each night, even if not remembered. A systematic review and meta-analysis published in 2020 showed a notably high presence of both depressive and anxiety symptoms among individuals with OSA, with anxiety symptoms reported in 32 percent of cases. Recognizing the presence of persistent anxiety as a potential indicator of OSA is crucial for a comprehensive health assessment, as effectively treating the sleep disorder can lead to a significant reduction in anxiety symptoms, as demonstrated in patient studies.
Read more about: Beyond Jaw Pain: Essential Heart Attack Warning Signs You Must Never Overlook, Especially for Women

6. **Mood Swings and Irritability**One of the most disruptive yet frequently dismissed indicators of Obstructive Sleep Apnea is the presence of pronounced mood swings and pervasive irritability. Family members and colleagues often notice these changes first, attributing them to general stress or personality quirks. However, these emotional fluctuations are often a direct consequence of the fragmented sleep architecture and the brain’s struggle to regulate emotions under chronic oxygen deprivation.
Fragmented sleep impairs emotional regulation, making individuals more prone to sudden, seemingly unprovoked mood changes. The brain relies on deep and REM sleep stages to process emotions, diffuse stress, and maintain emotional balance. When these critical sleep stages are repeatedly interrupted by apneic events, the brain’s ability to manage emotional responses is severely compromised, leading to a diminished capacity for emotional resilience and increased reactivity to everyday stressors.
Beyond emotional regulation, the chronic lack of restorative sleep and the underlying physiological stress contribute to a state of heightened agitation. The body is continually deprived of oxygen and then flooded with adrenaline, creating an internal environment ripe for irritability and short-temperedness. Patients in one study, for example, presented with symptoms related to humoral and cognitive spheres such as irritability, difficulty in concentrating, mood swings, and fatigue. If you or a loved one are experiencing unexplained and persistent shifts in mood or increased irritability, it’s a serious sign that your sleep health needs immediate attention and investigation for OSA.
Obstructive Sleep Apnea is a formidable adversary to overall health, its impact extending far beyond the immediate discomforts discussed in the previous section. As we delve deeper, we uncover the more insidious, long-term consequences that silently erode your well-being, from cognitive decline to a myriad of severe health complications, and crucially, how we can address them through accurate diagnosis and effective treatment.
Read more about: Beyond Fatigue: Crucial Thyroid Disorder Symptoms You Should Never Overlook, Including Early Signs That Begin in Your Hair and Skin

7. **Cognitive Decline and Memory Impairment**Beyond the fleeting mental fog many experience upon waking, Obstructive Sleep Apnea poses a serious, long-term threat to cognitive function and memory. This is not merely a matter of feeling a bit sluggish; it’s about the cumulative damage that can, over years, contribute to significant neurological issues. Experts suggest that conditions like Alzheimer’s disease can begin manifesting in the brain decades before overt symptoms appear, making early recognition of OSA’s impact vital.
The constant cycle of oxygen deprivation and fragmented sleep takes a massive toll on your brain’s health. When your brain is repeatedly deprived of oxygen and denied the restorative deep and REM sleep it needs, its ability to form new neural pathways, consolidate memories, and maintain overall cognitive resilience is severely compromised. This impairment can lead to persistent difficulties in learning, memory retention, and emotional processing, making daily tasks more challenging.
Evidence strongly supports this alarming connection. Older patients diagnosed with OSA face a higher risk of developing mild cognitive impairment and dementia. One study revealed a 1.7-fold increase in risk among participants with OSA, with the risk being even more pronounced in specific demographics. Men with OSA in their 50s showed a 6-fold greater risk of impairment, while women aged 70 years or older with OSA had a 3.2-fold greater risk, highlighting the severity of this link.
Recognizing these cognitive changes, such as your memory being notably worse than it was a decade ago or struggling with concentration, isn’t just about managing daily frustration. It’s about proactive health management. Screening for and treating OSA, alongside other sleep disturbances, offers a crucial pathway to help stem neurodegeneration and cognitive decline, potentially preserving your mental sharpness for years to come.
Read more about: Beyond Restlessness: Unpacking the Side Effects of Sleep Aids That Leave Patients Saying ‘Worse Than the Insomnia’

8. **Decreased Libido**Among the less frequently discussed, yet highly impactful, symptoms of Obstructive Sleep Apnea is decreased libido. While not life-threatening, a significant reduction in drive can profoundly affect an individual’s quality of life, relationships, and overall sense of well-being. This symptom is a direct outcome of the body’s chronic stress and exhaustion from continually disrupted sleep.
The persistent fatigue and ongoing stress response triggered by OSA profoundly affect hormonal balance. The body’s constant state of alarm, fueled by repeated oxygen drops and adrenaline surges during sleep, prioritizes survival functions over reproductive ones. This physiological shift can lead to imbalances in hormones crucial for ual desire, such as testosterone, contributing to a noticeable decline in libido.
It’s a symptom specifically mentioned in the clinical presentation of OSA patients, alongside daytime sleepiness, fatigue, morning headaches, and confusion. Patients often attribute this diminished desire to age, relationship issues, or general life stress, missing the underlying connection to their sleep health. However, it’s a critical clue for clinicians and individuals alike, pointing towards a deeper physiological struggle.
Addressing OSA through effective treatment can often lead to a significant improvement in energy levels, mood, and overall physiological balance, which in turn can help restore libido. Recognizing decreased libido as a potential indicator of sleep apnea is important for a holistic understanding of the disorder’s widespread effects and empowers individuals to seek help for this often-overlooked aspect of their health.
Read more about: 12 Evidence-Based Techniques to Naturally Manage Anxiety and Reclaim Your Calm

9. **Broader Physiological Mechanisms Undermining Brain Health**To fully grasp the insidious nature of Obstructive Sleep Apnea, it’s essential to look beyond the symptoms and understand the intricate physiological mechanisms at play. Research has broadly indicated that the widespread neurological and psychiatric disorders associated with OSA can be traced back primarily to two core processes: sleep fragmentation and intermittent hypoxia. These aren’t just academic terms; they represent fundamental assaults on your brain’s integrity.
Sleep fragmentation, the repeated micro-awakenings caused by apneic events, constantly disrupts the delicate architecture of your sleep cycle. This chronic disruption leads to a cascade of negative effects throughout the body. It increases sympathetic nervous system activity, pushing your body into a constant ‘fight or flight’ mode even when you’re supposed to be resting. It also generates oxidative stress and neuroinflammation, essentially causing cellular damage and an inflammatory response within the brain itself, while decreasing vasomotor reactivity.
Meanwhile, intermittent hypoxia occurs as OSA patients are repeatedly and momentarily starved of oxygen throughout the night. These repeated drops in oxygen levels are incredibly damaging, accelerating cerebral small vessel disease. This can lead to hypoperfusion, meaning a lack of vital nutrients reaching the brain, and manifest as white matter integrity anomalies and even gray matter loss, directly impacting the brain’s structure and function. It also increases the permeability of the blood-brain barrier and further fuels neuroinflammation.
These interrelated processes are not isolated; they compound one another, creating a vicious cycle of damage. The combined effect results in neuronal damage, triggers neurodegenerative processes that can mimic or exacerbate conditions like Alzheimer’s, contributes to vascular depression, and ultimately leads to profound cognitive impairment. Understanding these mechanisms underscores why timely diagnosis and treatment are not just about improving sleep, but about safeguarding your long-term brain health.
Read more about: Beyond the Bait: Critical Challenges and Concerns That Can Turn Modern Fishing into an Environmental Hazard

10. **Increased Risk of Serious Physical Comorbidities**While the mental and cognitive impacts of Obstructive Sleep Apnea are increasingly highlighted, it’s vital not to overlook the profound and severe physical health consequences that untreated OSA can precipitate. The constant oxygen deprivation and adrenaline surges during sleep place an immense strain on virtually every system in the body, particularly the cardiovascular system, setting the stage for a host of serious medical problems.
The body’s struggle for breath each night triggers a powerful stress response, causing blood pressure to rise and the heart to work harder. This ongoing burden significantly increases the risk of developing conditions such as high blood pressure (hypertension), cardiac arrhythmias (irregular heartbeats), and metabolic syndrome. Over time, these conditions elevate the risk for far more critical events like heart disease, stroke, and the development or worsening of type 2 diabetes.
The physiological mechanisms driving these risks are complex. Chronic intermittent hypoxia and sleep fragmentation contribute to endothelial dysfunction, where the lining of blood vessels is damaged, and neuroinflammation, which affects both brain and vascular health. These processes exacerbate existing vulnerabilities and create new ones, making the body more susceptible to a wide range of chronic diseases. The cumulative effect of regularly disrupted sleep and oxygen deprivation stresses the circulatory system and vital organs immensely.
Ignoring sleep apnea means allowing this continuous internal struggle to take its toll, escalating your risk for potentially life-altering or life-ending physical conditions. This highlights why a comprehensive approach to health must include assessing and treating OSA, not only for immediate symptom relief but also for long-term disease prevention and the protection of your vital organs.
Read more about: Unpacking the Promise vs. Reality: 12 Weight Loss Apps & Why Users Are Calling Them ‘Gimmicks’
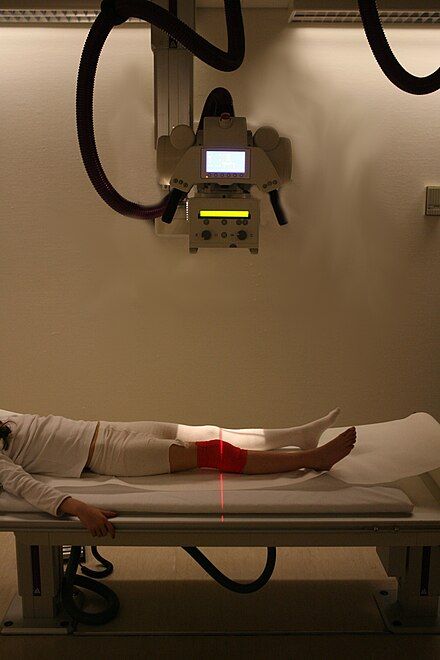
11. **The Crucial Role of Diagnosis: Sleep Studies**Given the diverse and often subtle ways Obstructive Sleep Apnea can manifest, diagnosing the condition accurately is absolutely crucial. Many individuals remain undiagnosed because their symptoms are either dismissed as normal aging, attributed to other conditions, or simply go unnoticed by the patient themselves. This is where professional clinical evaluation and diagnostic tools become indispensable.
The gold standard for diagnosing OSA is a sleep study, often referred to as polysomnography or a home sleep study. These studies are essential because they meticulously monitor critical physiological parameters while you sleep. A sleep study records your breathing patterns, blood oxygen levels, heart rate, brain activity, and muscle movements, providing a detailed picture of how your body functions during sleep. This comprehensive data allows medical professionals to identify the characteristic pauses in breathing and drops in oxygen that define OSA.
In recent years, home sleep studies have emerged as a convenient and affordable option, allowing individuals to self-administer the test in the comfort of their own homes. These devices monitor crucial data like blood oxygen levels, blood oxygen saturation, breathing, and heart rates, which are then reviewed by board-certified sleep physicians. This accessibility helps overcome barriers to diagnosis, though it’s important to remember that some insurance plans may not fully cover proper sleep studies, making it a challenge for some patients.
If you or a loved one are experiencing any of the persistent symptoms discussed, from loud snoring and daytime fatigue to mood disturbances and cognitive issues, undergoing a sleep apnea sleep study is a vital step. A proper diagnosis empowers you and your healthcare provider to understand the extent of the condition and to develop an effective, personalized treatment plan, paving the way to better health and well-being.
Read more about: Unraveling Marfan Syndrome: An In-Depth Look at its Multi-Systemic Impact and Evolving Care

12. **Effective Treatment Pathways for OSA**The good news amidst the serious implications of Obstructive Sleep Apnea is that it is a highly treatable problem. With the right diagnosis and commitment to therapy, individuals can significantly alleviate symptoms, improve their quality of life, and reduce their risk of long-term health complications. The treatment landscape offers a range of options, tailored to the severity of the condition and individual patient needs.
Often, the first line of treatment, especially for obese patients with mild symptoms, involves lifestyle modifications. Simple yet powerful changes like dietary adjustments to achieve weight loss and increasing physical activity can make individuals less prone to apneic episodes. Other lifestyle interventions include modifying sleep positioning, such as sleeping on one’s side, and limiting alcohol and sedatives, which can relax throat muscles and worsen airway collapse.
For more immediate and impactful intervention, continuous positive airway pressure (CPAP) therapy is the most common and effective treatment. A CPAP machine delivers constant airflow through a mask worn during sleep, keeping the airways open and preventing apneic episodes. Oral appliances, custom-fitted dental devices that reposition the jaw, offer another effective alternative, particularly for mild to moderate cases. Maxillomandibular advancement surgery, which physically expands the facial skeletal structure, is also an option for selected patients, especially those who cannot tolerate CPAP.
Beyond these, cognitive behavioral therapy (CBT) can be highly effective in managing sleep-related anxiety and improving adherence to CPAP therapy, addressing the psychological aspects that can impede treatment success. The important takeaway is that OSA, while serious, is manageable. By working closely with healthcare providers, individuals can explore these treatment pathways to restore restful sleep, improve their mental clarity, and protect their overall health from the insidious grip of sleep apnea.
Read more about: Beyond the Bloating: Essential Warning Signs of Ovarian Cysts, Including Lower Back Pain, You Should Understand
Obstructive Sleep Apnea is clearly more than just a nuisance; it’s a silent epidemic with far-reaching consequences for both mental and physical health. From insidious cognitive decline and mood disorders to severe cardiovascular complications, the impacts are profound. But with this deeper understanding comes empowerment. Recognizing these critical indicators and actively pursuing diagnosis and treatment can profoundly change the trajectory of your health, allowing you to regain the restorative sleep your body and mind desperately need to thrive. Prioritizing your sleep health is an investment in a longer, healthier, and more vibrant life.



