
In the whirlwind of our busy lives, it’s all too common to brush off persistent fatigue, unexplained pains, or sudden mood changes as ‘just stress,’ ‘getting older,’ or ‘something in our head.’ We’ve been conditioned to believe that minor discomforts are part of the daily grind. However, as a seasoned media editor who has poured over countless patient stories and expert insights, I can tell you that this mindset can be dangerously misleading. Misdiagnosis isn’t a rare anomaly; it’s a terrifyingly common occurrence, especially when serious health issues mimic everyday complaints. It’s a profound challenge that can lead to delayed treatment and avoidable suffering.
This article isn’t designed to spark fear, but rather to ignite a powerful sense of self-advocacy within you. Through personal experience and extensive research, I’ve learned that asking the right questions, pushing for thorough investigations, and truly trusting your instincts can be life-saving. We’re often told to listen to our bodies, but it’s equally important to understand how medical conditions can wear cunning disguises, making them incredibly difficult to pinpoint without specific knowledge and proactive measures.
Join us as we explore the first seven of fifteen serious health issues that frequently escape proper diagnosis, often hiding behind symptoms easily confused with anxiety, depression, or other less severe conditions. Our mission here is to arm you with the knowledge and tools necessary to be your own best health advocate, ensuring you and your loved ones receive the accurate care you deserve. Let’s dive in and unravel these medical mysteries, one vital condition at a time.

1. **Vitamin B12 Deficiency That Looks Like Alzheimer’s**I vividly recall a poignant story about a 57-year-old man who was slowly losing his cognitive faculties. He was experiencing hallucinations, stumbling, and showing all the distressing signs of what appeared to be dementia. Initially, his symptoms were misdiagnosed as depression, a label that unfortunately delayed the true understanding of his condition. It’s a stark reminder of how insidious some health issues can be, mimicking conditions that are far more commonly recognized.
As it turned out, his severe decline was not due to dementia or depression, but rather a profound Vitamin B12 deficiency. Low B12 levels can have a devastating impact on your brain, nerves, and mood, leading to a cascade of symptoms that include memory loss, confusion, and even hallucinations. In older adults, these manifestations are eerily similar to the signs of Alzheimer’s disease, creating a critical diagnostic challenge for healthcare providers.
The real “kicker” in many of these cases is that a “normal” B12 blood test might still fail to reveal the true problem. Doctors often wave off levels between 200–300 pg/mL as acceptable, yet individuals within this range can still suffer from what is known as a functional deficiency. This more nuanced deficiency only becomes apparent when specific markers like methylmalonic acid (MMA) or homocysteine are tested, highlighting the limitations of standard screening methods.
Certain groups face a higher risk of B12 deficiency. Vegetarians and vegans, whose diets naturally lack animal products rich in B12, are particularly vulnerable. The elderly population also commonly experiences absorption issues, as do individuals with specific medical conditions such as pernicious anemia or those who have undergone gut surgery. For these groups, vigilance and a deeper dive into diagnostic testing are paramount.
Therefore, if you or a loved one are exhibiting signs of cognitive decline, it’s crucial not to settle for a basic B12 test alone. Be proactive and insist on testing for MMA and homocysteine. This comprehensive approach can make all the difference in uncovering a treatable condition that might otherwise be tragically mistaken for an irreversible neurodegenerative disease, offering a path to recovery and improved quality of life.

2. **Hypothyroidism Misread as Depression**Have you ever felt persistently sluggish, unexpectedly sad, mentally foggy, or unusually cold, only to have doctors suggest antidepressants? It’s a scenario that plays out far too often, yet the underlying issue might not be a mood disorder at all. Instead, your body could be signaling a need for thyroid hormones, indicating a condition like hypothyroidism.
The reason for this widespread misdiagnosis lies in the striking overlap of symptoms. Hypothyroidism, a condition where your thyroid gland doesn’t produce enough hormones, can manifest as profound fatigue, inexplicable mood swings, and significant memory issues. These symptoms are, unfortunately, eerily similar to those associated with depression. This confusion is particularly prevalent in women, where such complaints are sometimes too readily dismissed as purely emotional or psychological in nature, overlooking a physiological cause.
Beneath these seemingly emotional symptoms could be Hashimoto’s thyroiditis, an autoimmune condition where the body’s immune system mistakenly attacks and gradually slows down the thyroid gland. Without proper and comprehensive testing, this underlying autoimmune process can remain undetected for years. Merely testing TSH (Thyroid-Stimulating Hormone) often isn’t enough; a thorough evaluation requires testing free T3, free T4, and thyroid antibodies to reveal the full picture of thyroid function.
Recent data underscores the severity of this issue. A 2024 survey revealed that a significant 2.4% of women presenting with thyroid problems were initially misdiagnosed as having mental health conditions. This alarming statistic points to systemic issues, including outdated diagnostic norms that contribute to women being consistently under-tested for thyroid dysfunction, delaying their path to appropriate care and relief.
This is why advocating for yourself is so important. If you suspect your symptoms might be related to your thyroid, don’t hesitate to ask for a full thyroid panel that includes all the necessary markers. This simple yet crucial step could be transformative, helping you move beyond a misdiagnosis of depression and toward the correct treatment that truly addresses your body’s needs, potentially changing your life for the better.

3. **Women’s Heart Attacks Dismissed as Anxiety**For women experiencing symptoms like chest pain, unusual fatigue, or even jaw pain, the response from medical professionals can sometimes be a dismissive, “it’s just anxiety.” This phenomenon, often described as medical gaslighting, is not only frustrating but incredibly dangerous. It can lead to life-threatening delays in diagnosing a serious cardiac event, underscoring a critical gender bias in medicine.
The core of this issue lies in how men’s and women’s heart attack symptoms are typically perceived. Men often present with the “textbook” crushing chest pain, making diagnosis more straightforward. However, women’s symptoms frequently deviate from this classic presentation, manifesting as more subtle or atypical signs such as jaw pain, nausea, shortness of breath, or a general feeling of unease. Because these symptoms are less recognized, women are tragically 50% more likely to be misdiagnosed during a cardiac event than men.
A compelling 2024 study further illuminated this disparity, finding that 4.6% of women with serious heart conditions were initially brushed off with an anxiety label. The context vividly recounts the experience of one woman who was explicitly told her pain was “all in her head”—only to discover she required emergency intervention for a genuine heart condition. This highlights how easily severe physiological distress can be misinterpreted as psychological, with severe consequences.
Compounding the problem, general anxiety can cause a rapid heart rate, sweating, difficulty sleeping, nausea, and difficulty breathing. These physical symptoms mirror those of a heart attack, creating a complex diagnostic challenge. While some people may indeed experience anxiety alongside a medical condition, or even due to the trauma of health challenges, doctors sometimes attribute *all* symptoms to anxiety when another underlying issue is at play.
If you are a woman experiencing new, severe, or genuinely frightening symptoms that could indicate a cardiac issue, it is imperative to advocate fiercely for yourself. Do not allow your concerns to be dismissed as mere anxiety. Insist on immediate diagnostic tests such as an ECG (electrocardiogram) or cardiac enzymes. These objective measurements can quickly differentiate between a panic attack and a potentially life-threatening heart condition, ensuring you receive timely and appropriate medical attention.
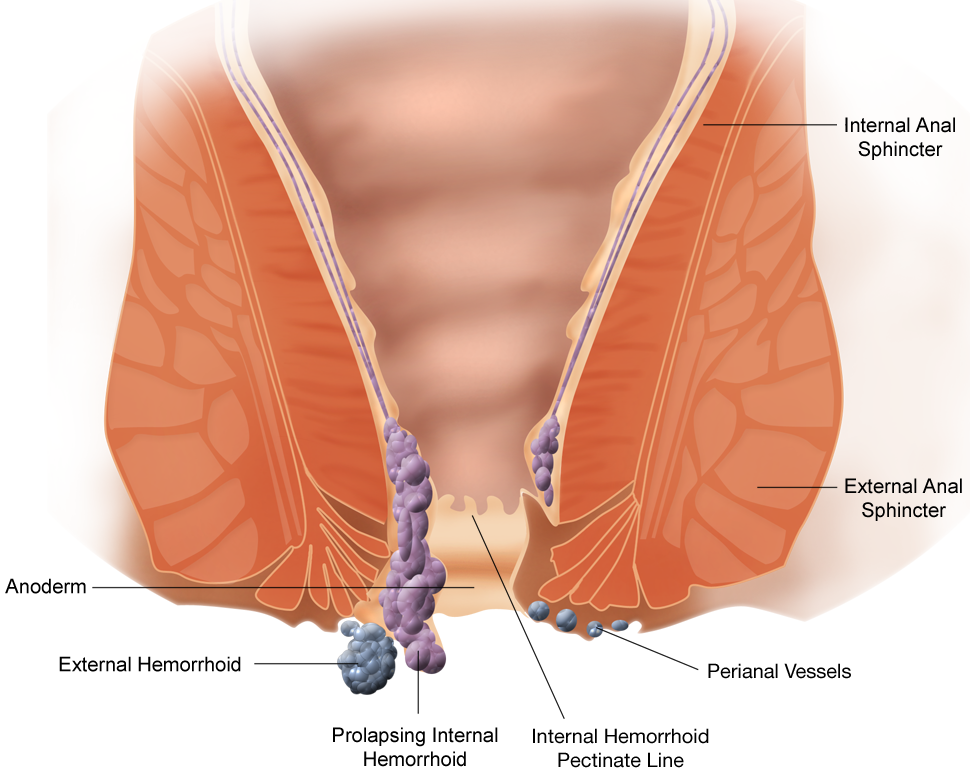
4. **Colon Cancer Misjudged as Hemorrhoids**Discovering blood when you go to the bathroom can be alarming, and often, doctors might reassure you that it’s simply hemorrhoids, particularly if you are under the age of 45. While hemorrhoids are a common and generally benign condition, this seemingly innocuous diagnosis can be a dangerous oversight. The reality is that colon cancer is on the rise among younger adults, and mislabeling serious symptoms can tragically cost lives by delaying critical treatment.
It’s essential to be aware of the red flags that suggest something more serious than mere piles. Persistent rectal bleeding that doesn’t resolve, constant abdominal pain that doesn’t ease, unexplained weight loss, and changes in bowel habits—such as alternating episodes of diarrhea and constipation—are all crucial indicators that warrant deeper investigation. These symptoms, especially when they persist or occur in combination, should never be ignored or casually dismissed.
Disturbing statistics highlight the prevalence of this misdiagnosis. In one study, a significant 15–20% of colorectal cancer patients were initially misdiagnosed with hemorrhoids. This often led to delays in treatment that could extend up to a year, a critical period during which cancer can progress and become much more challenging to treat effectively. Such delays can have profound and devastating impacts on patient outcomes and survival rates.
The traditional approach to colonoscopies, often recommending them primarily for individuals over 50, is increasingly being challenged by current trends. Given the rising incidence of colon cancer in younger demographics, a proactive stance is becoming vital. If you experience persistent symptoms like those mentioned, or if your gut instincts tell you something is wrong, you must push for a colonoscopy, regardless of your age.
Taking this assertive step is a crucial aspect of self-advocacy. Early detection dramatically improves the prognosis for colon cancer, making it a potentially curable disease. Therefore, if your symptoms persist and your doctor is hesitant, do not shy away from insisting on the necessary diagnostic procedures to rule out or confirm a more serious condition, safeguarding your long-term health.

5. **Brain Tumors That Look Like Mood Swings**I once heard a friend recount a distressing change in his father’s behavior, noting, “My dad was getting so mean—it wasn’t like him.” What initially seemed like a sudden shift in personality or a particularly bad mood turned out to be far more sinister. It was, in fact, a brain tumor, specifically one pressing against his frontal lobe, the area of the brain responsible for personality and behavior. This story powerfully illustrates how deeply medical conditions can impact our mental and emotional states.
When it comes to brain tumors, the symptoms can be incredibly deceptive, often mimicking psychiatric disorders. Watch out for sudden and uncharacteristic personality changes, such as unexpected aggression or pronounced apathy. Other warning signs include persistent headaches that differ from usual patterns, unexplained nausea, new-onset seizures, or noticeable changes in vision. These neurological symptoms are frequently overlooked or misattributed, leading to dangerous delays in diagnosis.
Tragically, these subtle yet critical symptoms often lead to patients receiving psychiatric labels and treatments before doctors even consider the possibility of a physical brain anomaly. The focus shifts to mental health interventions, diverting attention from the urgent need for neurological imaging. It’s a profound diagnostic pitfall where the internal workings of the brain are misread as purely psychological distress.
However, the truth can often be revealed through advanced imaging techniques. A CT (computed tomography) scan or an MRI (magnetic resonance imaging) can provide clear visual evidence of a brain tumor, pinpointing its location and size. These scans are indispensable tools that can literally save lives by enabling timely intervention, whether through surgery, radiation, or chemotherapy, before the tumor progresses further.
If you observe sudden and significant changes in a loved one’s behavior or personality, especially if accompanied by other neurological symptoms, do not hesitate. Time is of the essence in such situations. You must advocate passionately and push for neurological imaging without delay. This proactive step can be the critical factor in catching a brain tumor early, allowing for effective treatment and offering the best possible chance for recovery and preserving cognitive function.

6. **Lupus Masquerading as a Rash or Fatigue**Lupus is widely known in the medical community as the “great imitator,” a moniker earned due to its extraordinary ability to mimic a vast array of other conditions. Its symptoms can be so varied and non-specific that it’s frequently mistaken for common ailments like allergies, general fatigue, arthritis, or even anxiety. This makes diagnosing lupus a significant challenge, often leading patients on a prolonged and frustrating journey before receiving an accurate diagnosis.
What might you notice if lupus is at play? One classic sign is a distinctive butterfly-shaped rash that spreads across the cheeks and bridge of the nose. However, symptoms extend far beyond skin manifestations, including persistent aching joints, chronic and debilitating fatigue that doesn’t improve with rest, and unexplained low-grade fevers. More severely, lupus can involve vital organs, affecting the kidneys, heart, lungs, and brain, underscoring its systemic and serious nature.
The widespread and fluctuating nature of lupus symptoms makes it incredibly difficult to pin down. Patients often experience symptoms that come and go, or that affect multiple body systems simultaneously, further complicating the diagnostic process. This variability contributes significantly to the high rate of misdiagnosis, with an alarming 40% of lupus patients being incorrectly identified, sometimes for years.
Given the complexity and widespread impact of lupus, early and accurate diagnosis is absolutely critical for effective management and preventing organ damage. If you are experiencing a constellation of symptoms that seem to come and go, or if your health issues involve multiple systems of your body, it’s imperative to take action. Don’t settle for a generalized diagnosis that doesn’t fully explain your condition.
Your next crucial step should be to ask for an ANA (antinuclear antibody) test. This is a common screening test for autoimmune diseases like lupus. Furthermore, insist on a referral to a rheumatologist, a specialist in autoimmune and inflammatory conditions. A rheumatologist has the expertise to interpret complex symptom patterns and specialized test results, providing the focused attention needed to correctly diagnose and manage lupus, thereby improving your quality of life.

7. **Adult ADHD Confused With Stress**Are you constantly struggling to focus, frequently losing things, or missing deadlines, only to have someone suggest you’re simply “burnt out” or just need to manage your stress better? While stress is a ubiquitous part of modern life, these symptoms might actually be indicative of undiagnosed Adult Attention-Deficit/Hyperactivity Disorder (ADHD). This condition often flies under the radar in adults, particularly because its presentation differs significantly from childhood ADHD.
Adult ADHD is frequently missed because its symptoms don’t always align with the stereotypical image of a hyperactive child. In adults, ADHD often manifests as chronic distraction, persistent restlessness (which can be internal rather than outwardly hyperactive), and impulsivity. These signs are easily misinterpreted as general life stress, poor organizational skills, or a lack of motivation, rather than a neurodevelopmental condition.
There’s a notable gender disparity in how adult ADHD is identified. It is frequently dismissed in women, who tend to internalize their symptoms. Many women with ADHD might develop coping mechanisms to “mask” their difficulties, leading them to misattribute their struggles to anxiety, perfectionism, or general overwhelm. This internal struggle often prevents their condition from being recognized by healthcare professionals who may be less familiar with atypical presentations.
Recent research underscores the scale of this problem. In 2024, studies found that a substantial 42% of adult ADHD cases were initially misdiagnosed, with anxiety or depression being the most common incorrect labels. This is particularly problematic for women, whose tendency to mask symptoms makes accurate diagnosis even more challenging. The impact of such misdiagnosis can lead to years of ineffective treatment and a lack of understanding regarding their genuine struggles.
If you find yourself identifying with these patterns, and suspect that your chronic distraction, restlessness, or impulsivity might be more than just stress, it’s time to take a proactive approach. Do not hesitate to request an ADHD screening that utilizes the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria. This standardized assessment provides a comprehensive framework for accurate diagnosis, moving beyond superficial discussions about stress and towards a clearer understanding of your cognitive profile, opening the door to appropriate support and strategies for thriving.
Decoding the Disguises: Eight More Critical Health Conditions Frequently Misidentified, Empowering You to Seek Accurate Diagnosis and Life-Saving Care.
We’ve uncovered some truly astonishing cases of misdiagnosis in our journey so far, shedding light on conditions that hide in plain sight. But the detective work doesn’t stop there. As we continue to navigate the complexities of our health, it’s vital to stay informed about even more subtle and cunning disguises that serious medical issues can wear. Remember, every piece of knowledge you gain is a shield against potential medical oversights, empowering you to stand firm and advocate for the care you truly deserve. Let’s dive into the next chapter of understanding, where we’ll explore eight additional conditions that are often mistaken for something less severe, but demand our keen attention.

8. **Fatigue That Was Really Heart Failure**How often do we simply attribute persistent tiredness to the demands of a hectic schedule, not enough sleep, or perhaps just getting older? It’s incredibly easy for doctors, and for us, to wave off chronic fatigue as a minor, manageable complaint. However, for some individuals, this overwhelming exhaustion isn’t merely a symptom of a busy life or a passing phase; it can be an early, critical warning sign of something far more serious: heart failure.
When fatigue goes beyond normal tiredness, becoming debilitating and unresponsive to rest, it demands closer scrutiny. Beyond just feeling weary, keep a vigilant eye out for accompanying symptoms such as noticeable swelling in your feet and legs, experiencing shortness of breath even with mild exertion, or a diminished tolerance for physical activity. These are not isolated incidents but rather crucial signals from your body that warrant immediate attention.
The statistics are a powerful call to action: a 2022 study highlighted that a significant one in five heart failure patients endured a misdiagnosis for over a year. This delay is not just frustrating; it can have profound impacts on treatment effectiveness and long-term health outcomes. If you’re experiencing these persistent symptoms, don’t just hope they go away. Be proactive and insist on specific diagnostic steps.
Accurate diagnosis often hinges on objective medical tests. Simple blood tests, particularly those that measure B-type natriuretic peptide (BNP), can be incredibly insightful, as elevated levels may indicate stress on the heart. Furthermore, an echocardiogram—a non-invasive ultrasound of the heart—can provide detailed images of your heart’s structure and function, helping to reveal early cardiac issues that might otherwise be missed. Taking these steps can truly make a difference in identifying and managing heart failure promptly.
Read more about: Beyond the Hype: Unmasking the Worst Fast Fashion Brands of 2025, Ranked by Consumer Scrutiny for Ethics & Sustainability

9. **Eye Floaters That Signaled Retinal Tear**Many of us have experienced the occasional “floater”—those tiny specks or cobwebs that drift across our vision, often dismissed by a GP as harmless and a natural part of aging. While often benign, this casual dismissal can be incredibly dangerous. In certain cases, these seemingly innocuous visual disturbances can be an urgent signal of a serious underlying condition: a retinal tear, which can quickly escalate into a retinal detachment.
There are specific symptoms that absolutely demand immediate attention and distinguish serious issues from ordinary floaters. If you suddenly experience a significant increase in the number of floaters, or if they appear alongside flashes of light, it’s an urgent warning. Furthermore, any perception of a shadow or a “curtain” falling over your field of vision, or a sudden blurring or distortion of sight, indicates a critical emergency.
Research underscores the potential for misdiagnosis in these cases. A 2023 study revealed that between 10% and 15% of retinal tears were initially misdiagnosed, leading to crucial delays. A retinal detachment is not merely an inconvenience; it is a true medical emergency. Any significant delay in diagnosis and treatment can result in permanent vision loss, making swift action absolutely paramount.
If you ever experience sudden flashes of light, a dramatic increase in floaters, or any of the other urgent visual changes described, do not hesitate. Call an eye doctor—a specialist like an ophthalmologist or optometrist—immediately, ideally on the very same day. Explaining the sudden and severe nature of your symptoms will help them understand the urgency and prioritize your appointment, potentially saving your sight.

10. **That Back Pain Was Pancreatic Cancer**Back pain is one of life’s most common complaints, often attributed to muscle strain, poor posture, or simply overexertion. Because it’s so ubiquitous, persistent back pain, particularly in the mid-back or upper abdomen, can easily be misattributed to these less serious causes. However, in rare but devastating instances, this seemingly ordinary pain can be the first, and sometimes only, indicator of a much more sinister foe: pancreatic cancer.
When your back pain persists and feels different—perhaps radiating from the mid-back to the upper abdomen—it’s crucial to consider other potential warning signs. Look out for unexplained weight loss, which can be a subtle but significant red flag. Jaundice, characterized by a yellowing of the eyes or skin, is another critical symptom. Additionally, any noticeable changes in stool consistency or digestion, such as pale, greasy stools, or new-onset diabetes, should raise alarms.
The implications of misdiagnosis in pancreatic cancer are particularly grim. A 2021 study revealed a concerning statistic: one in four pancreatic cancer patients initially experienced back pain that was misdiagnosed before the true, devastating diagnosis emerged. Tragically, by the time many pancreatic cancers are correctly identified, they have often advanced to a stage where treatment options are limited, severely impacting prognosis.
If you are experiencing persistent, unexplained back pain, especially when accompanied by other digestive symptoms, jaundice, or unexplained weight loss, do not accept a superficial diagnosis. You must advocate for a more thorough investigation. Insist on advanced imaging tests such as a CT scan (computed tomography) or an MRI (magnetic resonance imaging). These vital diagnostic tools can provide the clarity needed to identify or rule out pancreatic cancer, potentially leading to earlier intervention and a better chance at survival.
Read more about: Beyond Jaw Pain: Essential Heart Attack Warning Signs You Must Never Overlook, Especially for Women
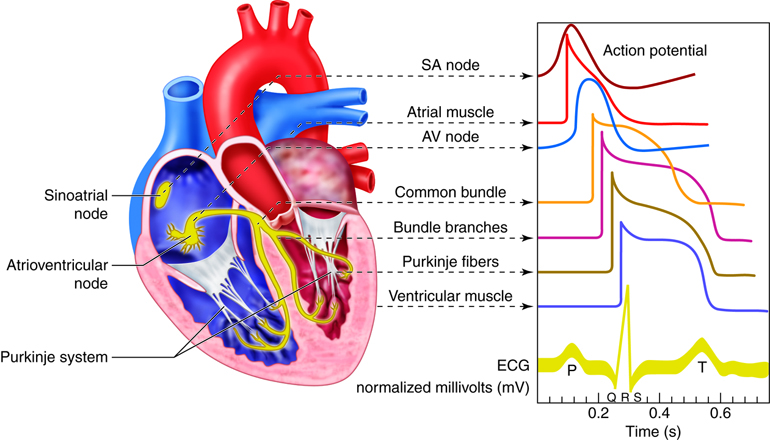
11. **Cardiac Arrhythmias: The Heart’s Role in Anxiety-like Symptoms**The alarming sensation of a racing or fluttering heart is often immediately linked in our minds to anxiety or a panic attack. While anxiety can certainly trigger these sensations, there’s a vital distinction to be made: irregular heartbeats, known as cardiac arrhythmias, can present with symptoms that are strikingly similar to anxiety attacks. This overlap frequently leads to misdiagnosis, leaving a potentially serious cardiac issue unaddressed.
Individuals suffering from arrhythmias commonly report a range of unsettling symptoms. These include noticeable palpitations, a sudden onset of dizziness, and unexplained shortness of breath. The feeling of a heart that is not beating rhythmically can be incredibly frightening, easily leading individuals to believe they are experiencing an anxiety attack or pure psychological distress, especially when other cardiac symptoms are less prominent.
It’s crucial to understand that arrhythmias are a structural or functional issue with the heart’s electrical system, demanding specific medical attention that goes beyond managing anxiety. Objective diagnostic tools are key here. An Electrocardiogram (ECG or EKG) can record the electrical activity of your heart and reveal irregular rhythms. Other cardiac tests, such as Holter monitors or event recorders, can track heart rhythms over longer periods, capturing intermittent arrhythmias that might not be present during a brief office visit. Recognizing the heart’s direct role in these symptoms is essential for both mental and physical well-being, as untreated arrhythmias can pose significant health risks, including stroke or more severe cardiac complications.
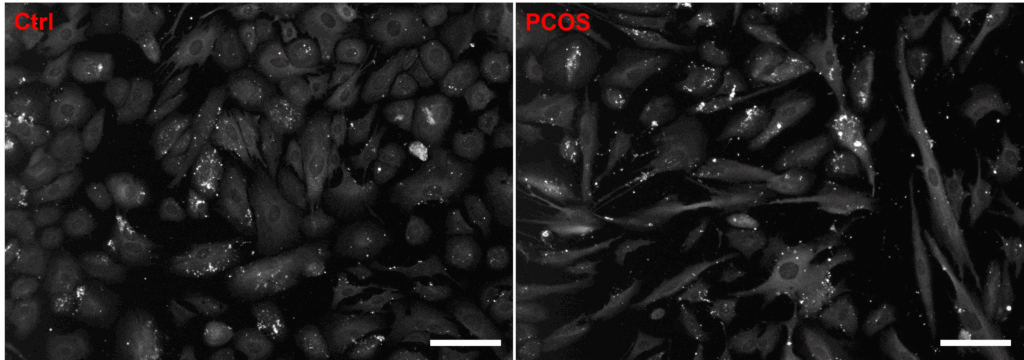
12. **Polycystic Ovary Syndrome (PCOS) Mistaken for Anxiety**For many women, the journey through hormonal health can be fraught with misunderstanding, and Polycystic Ovary Syndrome, or PCOS, stands as a prime example of a condition often entangled with anxiety. PCOS is a common hormonal disorder characterized by enlarged ovaries that may develop small cysts on their outer edges. While anxiety disorders can indeed coexist with PCOS, the hormonal imbalances inherent in the syndrome can directly manifest in ways that are easily mistaken for anxiety itself, leading to diagnostic confusion.
The intricate interplay of hormones in PCOS can directly impact a woman’s emotional and mental state. Hormonal imbalances, particularly higher levels of androgens (male hormones), can lead to noticeable mood changes, persistent fatigue, and increased irritability. These are precisely the kinds of emotional and physical symptoms that are frequently encountered in anxiety disorders, blurring the lines between a hormonal issue and a purely psychological one.
However, there are distinct characteristics that differentiate PCOS from anxiety. A key indicator of PCOS is higher-than-usual testosterone levels, which can be precisely determined through a simple blood test. Beyond anxiety-like symptoms, women with PCOS often experience irregular menstrual cycles, excessive hair growth on the face and body (hirsutism), acne, and weight gain. These physical manifestations offer crucial clues that point towards an underlying hormonal condition.
It’s imperative not to dismiss these combined symptoms as ‘just anxiety.’ As ‘Teen Mom’ star Maci Bookout powerfully shared, reflecting on her own experience with PCOS: “Sometimes I’m like if I didn’t have PCOS, then maybe I wouldn’t have been so irritable with my children today.” This personal insight highlights how deeply PCOS can impact daily life and mood. If you suspect PCOS, advocate for comprehensive hormonal blood tests to ensure a correct diagnosis and appropriate management plan, which can significantly improve both physical health and emotional well-being.
Read more about: Beyond the Veil: 7 Crucial Menstruation Facts Often Misunderstood – A Deep Dive into What Period Dramas (and Society) Miss
13. **Inflammatory Bowel Disease (IBD) Confused with Anxiety**When persistent stomach pain, cramping, and unpredictable bowel habits become a daily struggle, it’s not uncommon for these symptoms to be dismissed as general stress, irritable bowel syndrome (IBS), or even outright anxiety. Yet, for many, these uncomfortable gastrointestinal issues are actually the tell-tale signs of Inflammatory Bowel Disease, or IBD, a far more serious group of conditions that involve chronic inflammation of the gastrointestinal tract, including Crohn’s disease and ulcerative colitis.
The connection between gut health and mental health is undeniable, and symptoms of IBD can indeed create a deceptive mimicry of anxiety. Abdominal pain, cramping, and chronic fatigue, which are hallmarks of IBD, can directly lead to significant stress and anxiety. Conversely, stomach pain is also a well-known physical symptom of anxiety. This complex overlap makes it challenging for both patients and healthcare providers to pinpoint the true origin of the distress.
Delving deeper, conditions like Crohn’s disease are often misdiagnosed as merely IBS or anxiety due to their shared gastrointestinal symptoms. However, Crohn’s is an inflammatory bowel disease, triggered by genetics, the immune system, or environmental factors that provoke an autoimmune response. It is fundamentally different from IBS, which is a functional disorder, and it is certainly not ’caused’ by anxiety, though stress can exacerbate its symptoms.
To differentiate IBD from anxiety or IBS, it’s vital to recognize the distinctive red flags of IBD. These often include chronic diarrhea, the presence of blood in the stool, and unexplained weight loss. For an accurate diagnosis, a healthcare professional will typically order specific diagnostic procedures such as a colonoscopy and various imaging studies. These tests provide concrete evidence of inflammation and structural changes within the digestive tract, which are absent in anxiety or typical IBS.
As Caitlyn McAfee Hieatt shared from her own experience: “I do have anxiety, but I also have also been recently diagnosed with Crohn’s disease. Before my diagnosis, I thought a lot of my Crohn’s symptoms were because of my anxiety, so I waited a lot longer to seek help than I should have.” Her story underscores the critical importance of listening to your body and pushing for a thorough investigation. A correct diagnosis of IBD can unlock specific treatments and management strategies, significantly improving quality of life and preventing long-term complications that generic anxiety treatments would fail to address.
**Be Your Own Health Advocate: The Unwavering Power of Informed Action**
Our journey through these fifteen frequently misdiagnosed health conditions has unveiled a critical truth: your health narrative is uniquely yours, and you are its most important storyteller. Doctors are experts, but they are also human, operating under time constraints and relying on the information you provide. The responsibility to know your body, trust your instincts, and ask incisive questions is not just a right; it’s a profound act of self-preservation.
Misdiagnosis is not merely a statistical anomaly; it represents lost time, avoidable suffering, and missed opportunities for early, effective treatment. By arming yourself with knowledge, understanding the subtle disguises these conditions wear, and insisting on comprehensive testing when something feels genuinely amiss, you become an empowered participant in your healthcare. Remember, your voice is the most powerful tool in your diagnostic arsenal. Don’t hesitate to seek a second opinion, push for specialized tests, or find a provider who truly listens. Your ability to advocate fiercely for yourself is the single most vital step towards catching something early, treating it right, and reclaiming the vibrant, healthy life you deserve.



