Mental health conditions, much like complex engineering systems, are common, and the advancements in treatment offer more pathways than ever for people to cope, recover, and ultimately thrive. Yet, an invisible force often acts as a significant impediment to these journeys: the pervasive and often insidious phenomenon of mental health stigma. This societal pressure can prevent or delay individuals from seeking essential care, or even cause them to discontinue treatment, much like unseen friction can hamper a vehicle’s optimal performance.
Stigma, in its essence, refers to the negative attitudes, beliefs, and stereotypes that people may harbor towards those who experience mental health conditions. Despite a growing wave of understanding and acceptance, deeply entrenched negative perceptions continue to influence individuals, families, and entire communities. This article aims to dismantle these misconceptions, providing an authoritative and detailed examination of the multifaceted challenges presented by mental health stigma, much like a meticulous review dissects the mechanics and dynamics of a high-performance machine.
Our journey will navigate through the intricate landscape of mental health stigma, scrutinizing its various manifestations and profound impacts. By meticulously charting these territories, we equip ourselves with the knowledge necessary to accelerate meaningful change, foster an environment of acceptance, and pave the way for a future where mental well-being is prioritized without prejudice. Understanding these underlying mechanisms is the first crucial step in engineering a more supportive and stigma-free society.
1. Understanding Stigma: Definition and Ubiquity
At its core, stigma is a powerful social construct, defined as “negative attitudes, beliefs, and stereotypes people may hold towards those who experience mental health conditions.” It is not merely a misunderstanding but a deeply ingrained pattern of thought that can shape perceptions and interactions in profound ways. This foundational definition helps us grasp the pervasive nature of the challenge we face, highlighting that stigma is not an abstract concept but a tangible barrier.
While progress has been made in public discourse around mental health, the reality on the ground indicates that “many individuals and communities still hold negative attitudes or beliefs about those living with mental health conditions.” This persistent presence demonstrates that simply increasing awareness is often insufficient; deeper, more systemic shifts are required to dismantle these long-standing perceptions. The journey towards genuine acceptance is ongoing, requiring sustained effort and a commitment to re-evaluating our collective mindset.
The universality of mental health stigma is a stark and sobering truth. A pivotal 2016 report unequivocally concluded that “there is no country, society or culture where people with mental illness have the same societal value as people without mental illness.” This global pervasive nature underscores that stigma is not a localized issue but a worldwide challenge demanding a synchronized and comprehensive response. It’s a universal design flaw that hinders human potential across all demographics.

2. The Three Pillars of Stigma: Structural, Public, and Self-Stigma
To effectively dismantle stigma, we must first understand its distinct architectures. Mental health stigma manifests in various forms, each presenting unique challenges. The context identifies three primary pillars: structural stigma, public stigma, and self-stigma. Each form contributes to the overall weight of prejudice, creating a complex web of discrimination that impacts individuals and communities.
Structural stigma is embedded within the very framework of society, “involving laws, regulations, and policies that can limit the rights of those with mental health conditions.” These systemic barriers can range from inadequate insurance coverage to restrictive employment regulations, creating institutional hurdles that disproportionately affect individuals with mental health challenges. This form of stigma operates on a macro level, shaping access to resources and fundamental opportunities, much like restrictive road design impacts vehicle flow.
Public stigma, conversely, refers to “negative attitudes and beliefs from individuals or from larger groups towards people with mental health conditions, or their families or health care providers that care for them.” This encompasses the societal judgments and stereotypes that lead to social exclusion, prejudice, and discrimination in everyday interactions. It is the widespread cultural narrative that often frames mental illness in a negative or fearful light, influencing how individuals are perceived and treated by those around them.
Finally, self-stigma emerges “from within the person with a mental health condition.” Individuals grappling with self-stigma “may believe they are flawed or blame themselves for having the condition.” This internalized prejudice can be profoundly damaging, leading to feelings of shame, worthlessness, and a reduced sense of self-efficacy. It represents the personal battle against societal narratives, often resulting in diminished hope and a reluctance to pursue recovery, much like an internal engine fault that undermines performance.
3. The Chilling Effect of Discrimination
When stigma moves beyond attitudes and beliefs and into action, it transforms into discrimination, creating tangible and often devastating consequences. “When stigma leads to discrimination, people living with mental health conditions may be treated negatively,” directly impeding their ability to lead full and meaningful lives. This shift from perception to prejudice marks a critical juncture in the experience of those with mental illness.
The real-world examples of this discrimination are stark and pervasive. Individuals may “experience being excluded by others in their social groups due to their mental health conditions.” Furthermore, professional and economic opportunities are often curtailed; “employers may not hire them, landlords may not rent to them.” Even within the healthcare system, the very place designed to offer support, “the health care system may offer a lower standard of care.” This systematic disadvantage compounds the burden of illness.
The psychological impact of such systemic discrimination is profound, often leading to a debilitating cycle of lowered self-esteem and self-efficacy. These negative experiences can foster thoughts such as “Why try? Someone like me is not worthy, or unable to work, live independently, or have good health.” This internal dialogue, fueled by external prejudice, creates a significant barrier to recovery and personal growth, effectively trapping individuals in a spiral of intended and unintended loss of opportunity.
Read more about: The Raw Horsepower of a Decade: 10 ’60s Contenders That Still Command the Track

4. Media’s Double-Edged Sword: Shaping Perceptions of Mental Illness
In our information-rich society, media serves as a powerful conduit, shaping public perception and, unfortunately, often perpetuating mental health stigma. “Media representations of people with mental illness can influence perceptions and stigma, and they have often been negative, inaccurate or violent representations.” The narratives presented in film, television, and news have a profound capacity to either reinforce stereotypes or challenge them, much like media reviews can define public perception of a new vehicle.
A compelling study by Scarf et al. in 2020 offers a recent, potent example: the popular film *Joker* (2019). This cinematic portrayal depicted a lead character with mental illness who descended into extreme violence. The research found that “viewing the film ‘was associated with higher levels of prejudice toward those with mental illness,'” illustrating the significant negative impact that such representations can have on public attitudes. These portrayals, even if fictional, can cement harmful associations in the public consciousness.
Beyond merely influencing public prejudice, the authors of the *Joker* study further suggested that the film “may exacerbate self-stigma for those with a mental illness, leading to delays in help seeking.” This highlights the dual harm of negative media: it not only fuels external bias but can also deepen the internalized struggles of individuals already facing mental health challenges. Such irresponsible portrayals act as roadblocks, diverting individuals from the path to recovery.

5. Individual Well-being Undermined: The Personal Toll of Stigma
For those living with mental health conditions, stigma and discrimination are not abstract concepts; they are lived realities that directly impact personal well-being. “Stigma and discrimination can contribute to worsening symptoms and reduced likelihood of getting treatment,” creating a vicious cycle where the very factors that could alleviate suffering are hindered. This direct link between stigma and clinical outcomes underscores the urgency of addressing this issue.
The effects of self-stigma, in particular, paint a grim picture for individual experience. A comprehensive review of research found that these internalized negative beliefs lead to a cascade of adverse outcomes among people diagnosed with severe mental illnesses. These can include “reduced hope,” which is critical for motivation and forward progress, and “lower self-esteem,” which erodes confidence and self-worth. Such impacts compromise the foundational elements of personal stability.
The personal toll extends further, manifesting as “increased psychiatric symptoms” due to the stress and isolation caused by stigma. Individuals often face “difficulties with social relationships,” as the fear of judgment or actual exclusion leads to withdrawal. Furthermore, there is a “reduced likelihood of staying with treatment,” undermining therapeutic efforts, and “more difficulties at work,” impacting financial stability and a sense of purpose. These are performance metrics indicating severe distress.

6. Recovery Roadblocks: How Stigma Impedes Healing
Recovery from mental illness is a complex and often arduous journey, made significantly more challenging by the presence of stigma. The path to healing, much like optimizing a vehicle for peak performance, requires consistent engagement and support. However, self-stigma specifically acts as a powerful impediment, making that journey far more difficult to navigate for those diagnosed with severe mental illnesses.
Extensive research has meticulously documented this detrimental connection. A “recent extensive review of research found that self-stigma leads to negative effects on recovery among people diagnosed with severe mental illnesses.” This finding is crucial, as it pinpoints how internalized societal judgments can undermine an individual’s own belief in their capacity to heal, thereby hindering the very process of recovery. It’s an internal resistance to forward momentum.
A compelling 2017 study by Oexle et al. further elucidated this enduring challenge, involving more than 200 individuals with mental illness tracked over a period of two years. The longitudinal data revealed a clear pattern: “greater self-stigma was associated with poorer recovery from mental illness after one and two years.” This empirical evidence solidifies the argument that addressing self-stigma is not merely about emotional comfort, but a critical component of successful long-term recovery strategies.

7. Beyond the Individual: Stigma’s Wider Societal and Economic Reach
The impact of mental health stigma extends far beyond the individual, creating widespread societal and economic repercussions that affect collective well-being. An editorial in The Lancet, a respected medical journal, highlights that “the impacts of stigma are pervasive, affecting political enthusiasm, charitable fundraising and availability, support for local services and underfunding of research for mental health relative to other health conditions.” This speaks to a systemic underappreciation of mental health needs.
This societal apathy translates into practical challenges across various domains. There is a demonstrable “reluctance to seek help or treatment and reduced likelihood of staying with treatment,” which directly impacts public health outcomes. “Social isolation” becomes a common experience, fragmenting community bonds. Furthermore, individuals face “fewer opportunities for work, school or social activities or trouble finding housing,” severely limiting their integration into society and economic stability.
The most severe forms of stigma can lead to “bullying, physical violence or harassment,” creating unsafe environments for those with mental health conditions. Economically, “health insurance that doesn’t adequately cover your mental illness treatment” places an immense burden on individuals and families. Ultimately, stigma can instill “the belief that you’ll never succeed at certain challenges or that you can’t improve your situation,” stifling potential and hindering overall societal progress. These systemic failures represent critical performance deficits in our social infrastructure.
Our exploration of mental health stigma has brought us through its complex mechanics and pervasive impacts, much like a detailed diagnostic review of a vehicle’s intricate systems. Now, we shift gears to the engineering of solutions, delving into the powerful strategies and innovative approaches designed to dismantle stigma and accelerate progress towards a truly supportive society. This section will meticulously examine the various interventions, the crucial role of personal narratives, and the practical actions that individuals and organizations can take, ultimately driving us toward a future of true parity and rights.
8. Public Health Approaches: Engineering Effective Anti-Stigma Interventions
The journey to effectively reduce mental health stigma is not a simple drive; it requires carefully engineered public health approaches, informed by years of dedicated research. We’ve learned that successful interventions are those that prioritize genuine connection and targeted strategies, moving beyond broad, often less effective, campaigns. These aren’t just about awareness; they are about fundamentally altering perceptions and behaviors, much like re-calibrating an engine for optimal performance.
Substantial research on anti-stigma interventions has illuminated several key components that make them truly impactful. Foremost among these is the inclusion of “contact,” which can be in-person or, when executed thoughtfully, through video. This direct or mediated interaction with individuals who have lived experience profoundly shifts perspectives. Moreover, effective interventions wisely “focus on a range of disorders, not just depression or mental illness broadly,” ensuring a comprehensive and inclusive approach that mirrors the diversity of human experience.
Another critical element involves the active “participation of people with ‘lived experience’,” whose authentic stories are indispensable in humanizing mental health challenges. These initiatives are also most potent when they “target groups that have the most interaction or where lack of help-seeking is most problematic,” such as young people, undocumented communities, or military communities. Furthermore, for maximum credibility and resonance, they must be “tailored to be credible to specific language and cultural signifiers of the target group” and are often designed to “last several years in order to be effective,” signifying a sustained commitment rather than a fleeting effort.
9. The Power of Personal Narratives: Unlocking Relatability and Empathy
In the intricate design of anti-stigma efforts, one of the most powerful catalysts for change is the simple yet profound act of sharing personal stories. Just as knowing the history of a beloved classic car brings it to life, knowing or having contact with someone who has experienced mental illness dramatically reduces the mystery and fear often associated with it, making it “less scary and more real and relatable.” This human connection builds bridges of understanding that no amount of abstract information can match.
The impact of individuals speaking out and sharing their journey cannot be overstated. When real people open up about their struggles and triumphs, they transform an abstract concept into a tangible human experience. This is especially true for young people, who are actively “searching for health information online and mental health issues are among the top searches.” They are looking for genuine connection, with “about four in 10 teens said they have looked for people with similar health concerns.”
The visibility of celebrities like Demi Lovato, Dwayne “The Rock” Johnson, Michael Phelps, Taraji P. Henson, and Lady Gaga publicly sharing their mental health challenges has been a game-changer. These influential voices have brought crucial discussions into the mainstream, demystifying mental illness and validating the experiences of countless others. Additionally, recent studies have confirmed the effectiveness of brief videos featuring personal experiences in reducing stigma and improving mental health care access, particularly for those in need, underscoring the power of lived experience in a digestible format.

10. Individual Actions: Driving Change from the Driver’s Seat
While large-scale campaigns are vital, the daily choices and actions of individuals represent a powerful, accessible mechanism for dismantling stigma, much like tuning a vehicle for optimal street performance. Each of us holds the steering wheel in this effort, capable of making conscious decisions that foster a more accepting and understanding environment. The National Alliance on Mental Illness (NAMI) provides an excellent roadmap for these personal contributions, empowering everyone to be an agent of change.
NAMI suggests several practical individual actions that collectively create a significant impact. First, “talk openly about mental health, such as sharing on social media,” normalizing conversations that have historically been shrouded in silence. Second, “educate yourself and others – respond to misperceptions or negative comments by sharing facts and experiences,” proactively correcting inaccuracies and fostering informed understanding. Third, “be conscious of language – remind people that words matter,” challenging stigmatizing terminology and promoting respectful discourse.
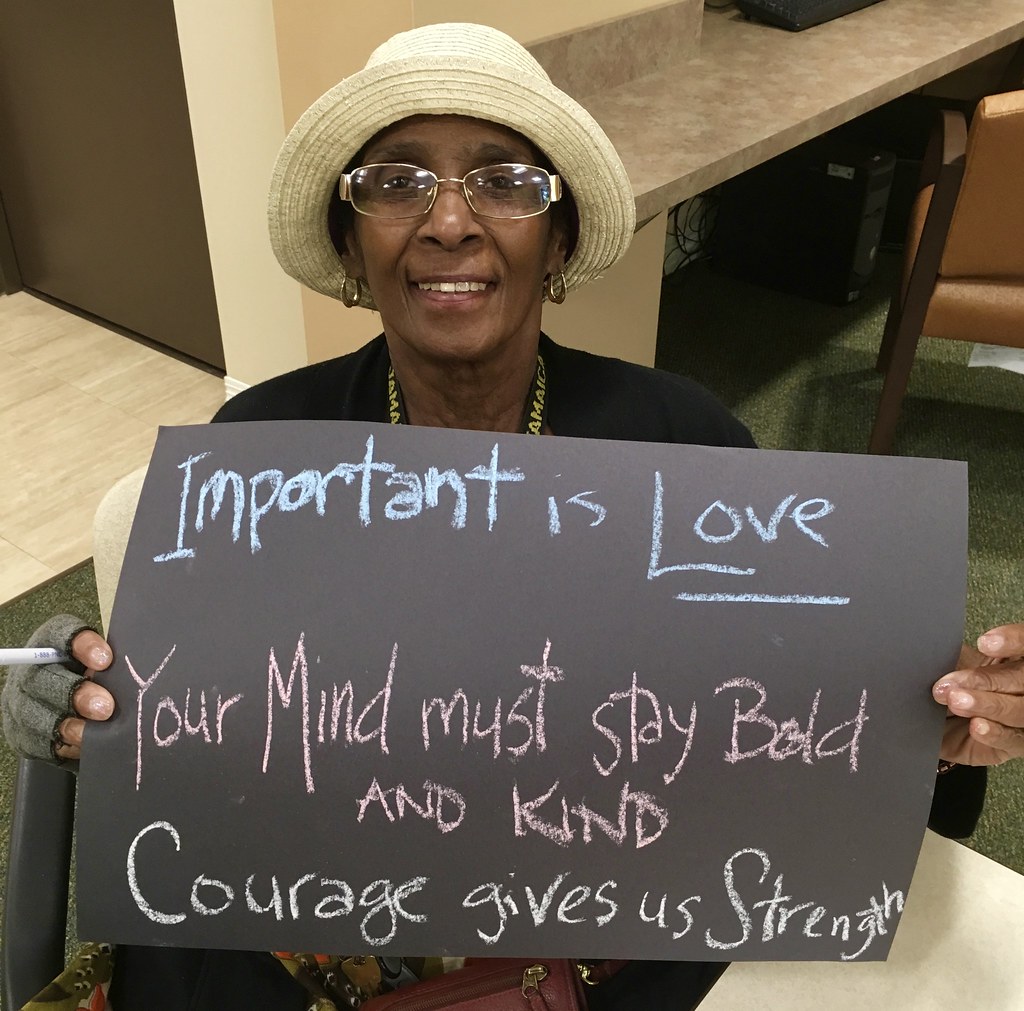
Further, NAMI encourages us to “encourage equality between physical and mental illness – draw comparisons to how they would treat someone with cancer or diabetes,” emphasizing that mental health conditions deserve the same compassion and care as physical ailments. It’s also crucial to “show compassion for those with mental illness” and “be honest about treatment – normalize mental health treatment, just like other health care treatment.” Finally, individuals can actively “let the media know when they are using stigmatizing language” and, perhaps most profoundly, “choose empowerment over shame,” embracing one’s story as a source of strength, as eloquently put by Val Fletcher: “I fight stigma by choosing to live an empowered life. To me, that means owning my life and my story and refusing to allow others to dictate how I view myself or how I feel about myself.”
Read more about: The 14 Car Features Drivers Are Paying For But Rarely Use: An Expert Dive Into Unutilized Tech

11. Workplace Stigma Reduction: Cultivating a Healthy Corporate Culture
Just as a high-performing automotive team nurtures its talent, forward-thinking employers are increasingly recognizing their pivotal role in addressing mental health stigma within the workplace. The work environment, where many spend a significant portion of their lives, can be either a source of stress or a beacon of support. Creating a truly “behaviorally healthy workplace” is not just good for employees; it’s a strategic imperative for attracting and retaining top talent, enhancing overall company culture.
While stigma and discrimination persist, organizations are making concerted efforts to foster an open and supportive atmosphere. The APA Foundation’s Center for Workplace Mental Health emphasizes the need for robust healthcare services coupled with deliberate actions to break the silence surrounding mental illness. Their vision is to “create a culture in which mention of depression, anxiety, post-trauma, and other common illnesses become as mentionable as diabetes, hypertension, and migraines,” promoting an environment where seeking help is as normalized as managing any other health condition.
Employers leading this charge offer practical advice: “tailor programs/approaches to your company culture and existing strengths,” ensuring relevance and effectiveness. They advocate for consistently mentioning a “commitment to leading a behaviorally healthy workplace” alongside other company values. Furthermore, “train leaders to identify emotional distress and make referrals and to responding promptly and constructively to behavioral performance issues,” equipping management with the skills to support their teams. Critically, being “welcoming of the need for accommodations” and training managers to respond appropriately ensures that mental health support is integrated into the fabric of the organization, much like a well-designed safety feature.
12. Organizations and Campaigns: A Fleet of Initiatives Driving Change
Across the nation, a diverse fleet of organizations and campaigns is passionately driving the movement to reduce mental health stigma and discrimination. These initiatives, each with its unique approach, are vital engines of change, building communities, providing resources, and amplifying voices to foster greater understanding and acceptance. Their collective impact is much like a well-coordinated rally, propelling the conversation forward at an impressive pace.
One prominent example is the “Love, Your Mind” campaign, a collaborative effort by the Huntsman Mental Health Institute and the Ad Council. This initiative provides “inspiration, community and educational resources to encourage people across the U.S. to be more open and proactive when it comes to their mental health,” encouraging self-care and open dialogue. Similarly, “Stop Stigma Together” aims to “unite organizations to create resources, generate funding, bring clarifying awareness, and address the issues around mental health and substance use disorders,” striving for true well-being.
“This is My Brave” offers a unique and powerful platform through storytelling theatre shows, where individuals bravely “share their stories of living a successful life despite mental illness.” Since 2014, they have empowered nearly 800 storytellers, and even launched BraveTV during the pandemic to continue sharing hope. The “Mental Health Coalition,” spearheaded by Kenneth Cole in partnership with numerous organizations and celebrities, focuses on “fighting stigma through the sharing of stories with the tag line ‘How are you really?'”, fostering authentic conversations. Other impactful campaigns include Glenn Close’s “Bring Change to Mind,” NAMI’s “StigmaFree campaign,” the “Stamp Out Stigma” initiative, and the “Healthy Minds with Dr. Jeffrey Borenstein” series, all contributing to a robust ecosystem of anti-stigma advocacy.
13. Research Insights: The Engine of Evidence-Based Stigma Reduction
To effectively combat mental health stigma, we must rely on rigorous research to understand which interventions truly move the needle, much like automotive engineers constantly test and refine new designs. Decades of social psychology literature have explored various approaches to changing public stigma, broadly categorized into protest, education, and contact strategies. While protest appeals to moral authority, the bulk of research focuses on education and contact as the primary mechanisms for fostering change.
Education, with its “seductive appeal” to simply teach people about social ills, often proves to be a less effective engine for deep-seated change. While promoting “mental health literacy may help people to better consume services,” research suggests it has “little impact on the prejudice and discrimination that limit a person’s rightful opportunities.” For instance, a review of sixteen population studies found that despite a significant increase in knowledge that conditions like schizophrenia are brain disorders, “no improvement in the stigma of depression was observed, and the stigma of schizophrenia actually worsened.”
Indeed, “unintended effects of education emerge when considering programs that frame ‘mental illness as a brain disorder,'” as this view is “highly associated with beliefs that people with mental illness are dangerous and incompetent.” While genetic models can decrease blame, they can also lead the public to believe that people “will not recover,” thus leading to “poor prognoses” that deter employers and landlords. In stark contrast, meta-analyses consistently show that “contact, compared to education, yielded significantly greater change in attitudes and behavioral intentions,” particularly through “in vivo contact” or face-to-face interactions, highlighting the irreplaceable power of personal connection.

14. Beyond Pity: Advocating for Parity and Rights
Our journey to understand and dismantle mental health stigma ultimately leads us to a fundamental paradigm shift: moving beyond mere pity towards a steadfast advocacy for parity and rights. While sadness and sympathy are natural reactions to the challenges of mental illness, research warns that an over-reliance on pity can have unintended, disempowering consequences, much like a well-intentioned but ultimately flawed vehicle design that undermines the driver’s control. True progress lies in fostering empathy that champions equality and self-determination.
Educational programs focusing on biological causes, while reducing blame, may inadvertently “increase pity” and lead to a “benevolence stigma,” where individuals with mental illness are perceived as “incapable of competently handling life’s demands,” requiring a “benevolent authority who can make decisions for them.” This patronizing view can obstruct recovery and disempower individuals, stripping them of their autonomy and agency. Advocates and researchers emphatically argue that “appeals to sympathy must be replaced by calls for empowerment and self-determination,” ensuring that all decisions about life goals and interventions remain firmly “in the hands of the person with mental illness.”
This critical shift informs the two distinct yet often competing agendas in stigma change: the “services agenda” and the “rights agenda.” The services agenda seeks to “destigmatize mental illnesses by framing them as treatable disorders,” aiming to promote help-seeking and engagement with evidence-based services. In contrast, the rights agenda, much like a powerful engine designed for enduring performance, “poses mental illness stigma in the same light as any civil right, calling for ending discrimination and promoting opportunities.” While both are vital, they have different messages, expected benefits, and drivers, underscoring the comprehensive, multi-faceted approach required to achieve the ultimate goal: parity, not pity.
The road ahead for mental health is undoubtedly challenging, but the collective drive towards a stigma-free society is gaining powerful momentum. From innovative public health strategies to the brave voices sharing personal narratives, and from individual acts of kindness to sweeping organizational commitments, the gears are turning. We’re learning that genuine connection, informed action, and an unwavering commitment to equality are the core components of this transformation. By understanding the intricate mechanics of stigma and championing evidence-based solutions, we can engineer a future where mental well-being is not just understood, but truly valued, ensuring every individual has the right to thrive on their own terms, free from prejudice. The destination is clear: a world where mental health is recognized as an integral part of human experience, deserving of the same respect, resources, and rights as physical health. Let’s drive forward with purpose and unwavering resolve.




