Pancreatic cancer is notoriously aggressive and presents a silent threat, often going undetected until it reaches more advanced stages. This formidable challenge is underscored by Dr. Mark Truty, a surgical oncologist at Mayo Clinic, who states, “It’s the most deadly — the least survivable — of all cancers that we know of.” The insidious nature of this disease means that its subtle warning signs can easily be overlooked or attributed to less serious conditions, making early detection a true “holy grail of medicine,” as described by radiologist Dr. Ajit Goenka.
While the symptoms can be vague and appear in unexpected places, understanding these indicators is paramount. The journey toward an earlier diagnosis begins with heightened awareness and a proactive approach to one’s health. It’s crucial for everyone to be informed about the potential signals the body might be sending, even those that manifest far from the pancreas itself.
This in-depth exploration will shed light on some of the most vital warning signs associated with pancreatic cancer, drawing directly from expert insights and medical research. By focusing on both specific and seemingly nonspecific symptoms, including those that can surprisingly begin in the legs, we aim to equip you with the knowledge to recognize when it’s time to seek immediate medical attention. Our goal is to empower you to take charge of your health and advocate for thorough investigation should these red flags emerge.
1. **Deep Vein Thrombosis (DVT) in the Legs**
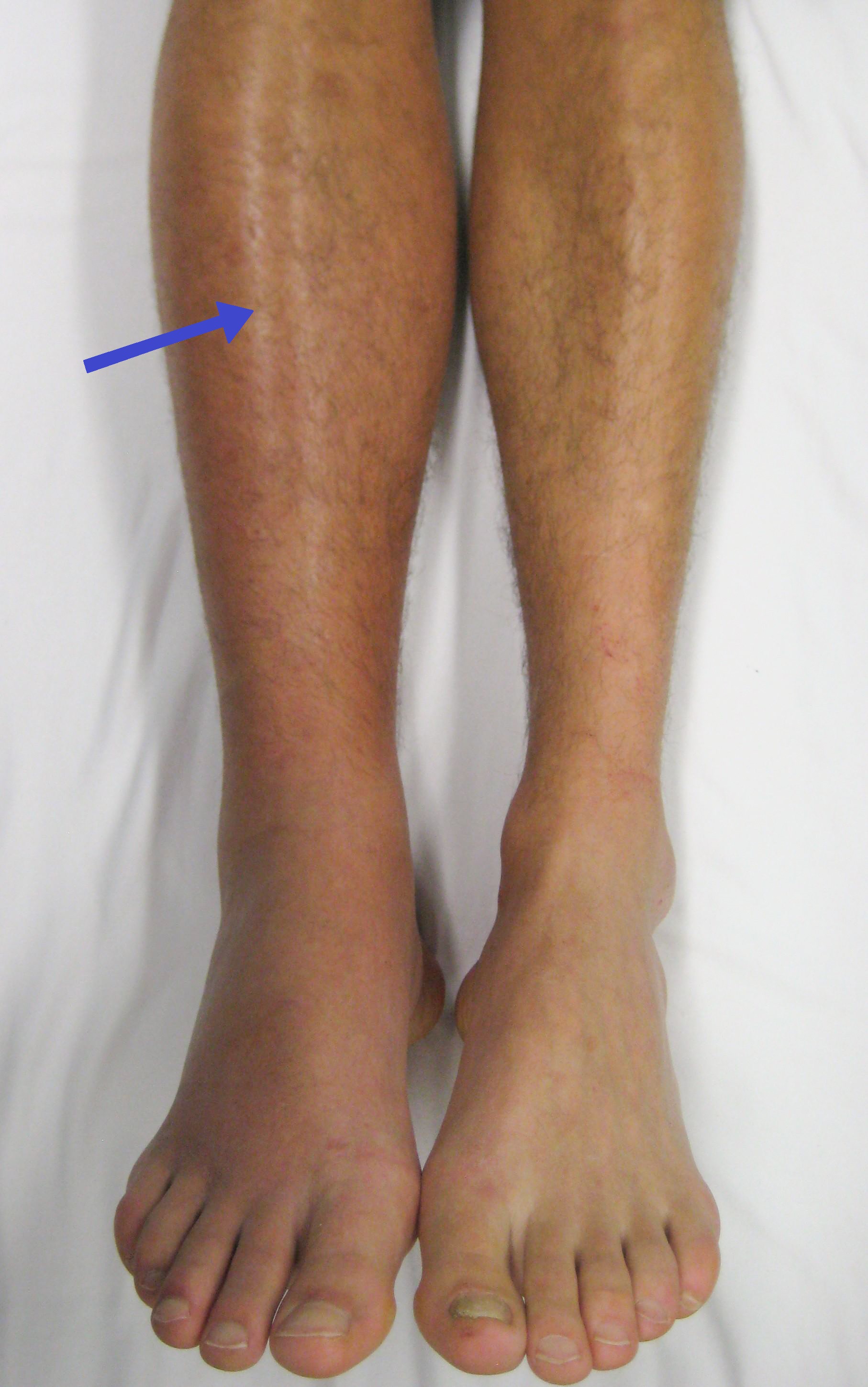
One of the most unexpected, yet crucial, early warning signs of pancreatic cancer can manifest in the legs: deep vein thrombosis, or DVT. This serious condition involves the formation of a blood clot in a deep vein, typically located in the legs or pelvis. What makes DVT particularly significant in the context of pancreatic cancer is its potential as a “first clue” that something more serious might be occurring within the body. According to the American Cancer Society, “sometimes, the first clue that someone has pancreatic cancer is a blood clot in a large vein, often in the leg,” highlighting its diagnostic importance.
Recognizing the specific symptoms of DVT in your legs is therefore essential. The four main signs that warrant immediate attention are severe pain, swelling, redness, and warmth in the affected limb. This localized discomfort and visible changes are not merely minor inconveniences; they are signals that your circulatory system is compromised. These symptoms arise because the blood clot obstructs normal blood flow, leading to inflammation and fluid buildup in the surrounding tissues. It’s important to differentiate this from everyday aches or minor injuries, as DVT symptoms are often persistent and can worsen over time.
The danger associated with DVT extends beyond localized discomfort. A significant concern is when a piece of the blood clot breaks off and travels through the bloodstream, potentially reaching the lungs. This condition, known as a pulmonary embolism (PE), is a life-threatening emergency characterized by symptoms such as difficulty breathing or chest pain. Doctors emphasize that when a blood clot travels to other body parts, including the lungs, it demands immediate medical treatment. Those diagnosed with pancreatic cancer are known to have a higher risk of blood clot formation, making these leg symptoms particularly relevant for early detection.
Experts explain that several factors contribute to this heightened risk of blood clot formation in individuals with pancreatic cancer. The cancer itself can alter the blood’s clotting mechanisms, making it more prone to form clots. Furthermore, various treatments for pancreatic cancer, such as chemotherapy or surgical procedures performed to remove a tumor, can also increase the likelihood of DVT. Even decreased mobility following surgery, a common aspect of recovery, can significantly elevate the risk of blood clots. Therefore, any new or worsening signs of DVT in the legs should trigger a prompt medical evaluation, especially when considering the possibility of an underlying condition like pancreatic cancer.
Read more about: Beyond ‘Toughing It Out’: 15 Critical Health Symptoms Men Must Never Ignore

2. **Jaundice and Related Symptoms**
Jaundice stands out as one of the most specific and visually apparent warning signs that can indicate pancreatic cancer. This condition is characterized by a distinctive yellowing of the whites of your eyes and your skin. Its appearance is a critical indicator because, as Dr. Mark Truty notes, “It isn’t until we see really specific things like jaundice, or skin turning yellow, or stools turning a lighter color, or urine getting darker… that we associate symptoms with pancreatic cancer.” This makes jaundice a symptom that should never be ignored, prompting immediate medical investigation.
The underlying cause of jaundice is the buildup of a chemical called bilirubin in your tissues. Bilirubin is a dark yellow-brown waste product generated by your liver when it breaks down old red blood cells. It’s a key component of bile, a substance produced by your liver to aid in the digestion of food, particularly fats. In the context of pancreatic cancer, a growing tumor often blocks the bile duct, the pathway that releases bile into your intestine. When bile cannot flow through this blocked duct, bilirubin accumulates in the body, leading to the yellow discoloration of jaundice.
The location of the tumor plays a significant role in when jaundice might appear. Adenocarcinoma tumors, which account for about 90% of pancreatic cancers, often start in the head of the pancreas. Because the head of the pancreas is situated near the bile duct, even a relatively small tumor in this area can obstruct the duct, causing jaundice to develop relatively early, sometimes while the cancer is still contained within the pancreas. However, if a tumor begins in the body or tail of the pancreas, which are farther from the bile duct, jaundice may not become apparent until the cancer has grown larger or spread to the liver, impacting its function.
Beyond the noticeable yellowing, jaundice can also present with several other symptoms that are directly related to bilirubin buildup. Itchy skin is a common complaint, as the accumulation of bilirubin can irritate nerve endings in the skin, leading to itching that may be mild or severe and can occur anywhere on the body, including the hands, feet, arms, or legs. Another tell-tale sign is dark yellow or brown urine, which can sometimes be the first indication of developing jaundice, as the body attempts to excrete excess bilirubin through the kidneys. Conversely, light-colored or clay-colored poop (pale gray or beige instead of brown) is also a strong indicator, as bilirubin is what normally gives stool its brown color. Without bile flowing into the intestine, the stool lacks its usual pigment. Moreover, the inability to digest fats properly due to bile duct blockage can result in fatty, very smelly poop that may float or stick to the sides of the toilet bowl.
Read more about: Beyond the Spotlight: Unraveling the Alleged Tragic Autopsy Details of Elvis Presley’s Final Days

3. **New-Onset Diabetes or Worsening Diabetes**
The pancreas plays a dual vital role in the body: producing enzymes for digestion and manufacturing hormones like insulin to regulate blood sugar levels. When pancreatic cancer develops, it can directly impact the pancreas’s ability to perform this crucial endocrine function, leading to significant changes in blood sugar. The emergence of new-onset diabetes, particularly in adulthood, or a sudden, unexplained difficulty in managing pre-existing diabetes, can be a subtle yet powerful warning sign for pancreatic cancer, warranting careful attention from both patients and clinicians.
Diabetes can develop when chronic pancreatitis, a known risk factor for cancer, damages the cells that produce insulin. Similarly, “some people with pancreatic cancer develop high blood sugar (diabetes) as the tumor destroys the insulin-making cells in your pancreas.” This destruction of insulin-producing cells means the body loses its capacity to regulate blood glucose effectively, leading to elevated blood sugar levels. Your doctor may become suspicious of an underlying pancreatic issue if these blood sugar changes are observed on a blood test, especially if they appear suddenly without other clear explanations.
Patients experiencing new-onset diabetes may notice classical symptoms of high blood sugar, such as increased thirst, a persistent feeling of hunger, and having to urinate more frequently than usual. These symptoms often prompt a visit to the doctor for diabetes diagnosis and management. However, when these symptoms arise without typical risk factors for Type 2 diabetes, or if they appear alongside other vague digestive issues, it becomes even more critical to consider the pancreas’s health beyond just diabetes management. The context specifically mentions “another specific symptom of pancreatic cancer is diabetes that suddenly becomes difficult to treat,” indicating that even established diabetics should be vigilant about unexplained changes in their condition.
While diabetes itself is a widespread condition, the *suddenness* of its onset or a rapid, unexplainable deterioration in its management, particularly in older adults, can serve as a red flag for pancreatic cancer. It’s not the diabetes alone, but the context and trajectory of its development or change that matters. Therefore, if you experience sudden blood sugar changes or a new diagnosis of diabetes, especially without a clear hereditary predisposition or significant lifestyle changes, it is imperative to discuss the possibility of further investigation into pancreatic health with your doctor.
Read more about: A Month Before: Your Body’s 11 Subtle Signals Warning of a Coming Heart Attack

4. **Unexplained Weight Loss and Loss of Appetite**
Unexplained weight loss and a persistent loss of appetite are common symptoms across many health conditions, but when they occur in the context of pancreatic cancer, they carry significant weight as potential warning signs. These symptoms are frequently reported by patients and are among the key reasons doctors advise seeking medical attention. The insidious nature of pancreatic cancer means that these nonspecific symptoms, while easily dismissed, can be crucial indicators of a serious underlying problem, especially when they cannot be attributed to diet, increased activity, or other clear factors.
There are several reasons why individuals with pancreatic cancer might experience a profound loss of appetite and unintended weight loss. One contributing factor is the buildup of bilirubin in the body, which can occur if the tumor blocks the bile duct, as discussed with jaundice. This systemic accumulation of waste products can lead to a general feeling of malaise and a reduced desire to eat. Additionally, as the tumor grows, it may begin to compress nearby organs, including the stomach. This compression can lead to a sense of early fullness during meals (satiety) or an uncomfortable swelling in the abdomen, making eating a full meal difficult or unappealing. Patients may feel bloated or gassy, further deterring food intake.
Moreover, the pancreas plays a vital role in producing digestive enzymes necessary for breaking down food, particularly fats. With both acute and chronic pancreatitis, and critically, with pancreatic cancer, the pancreas may not produce sufficient amounts of these enzymes. This deficiency in digestive enzymes can lead to malnutrition, as the body struggles to absorb nutrients from food, even if it is consumed. This malabsorption, along with reduced intake, contributes directly to unintended weight loss and, in some cases, diarrhea. The body essentially starves for nutrients despite food being available, leading to a noticeable decline in physical mass.
Given the potential seriousness, experts strongly advise paying close attention to these symptoms. The Mayo Clinic explicitly lists “Losing weight without trying” as a sign of chronic pancreatitis, which itself is a risk factor for pancreatic cancer, and underscores the urgency to “see your doctor right away if you have… Unexplained weight loss.” It is not merely about shedding a few pounds; it is about a consistent, noticeable reduction in body weight without any intentional effort to do so, combined with a diminished interest in food. These signs, especially when coupled with other symptoms discussed, should serve as a powerful impetus for a thorough medical evaluation, ensuring that any underlying condition, including pancreatic cancer, is identified as early as possible.
Having explored the initial set of crucial indicators, our journey continues to unveil more vital symptoms that might signal the presence of pancreatic cancer. These signs, while sometimes subtle or easily confused with less serious ailments, carry significant weight in the context of this challenging disease. Recognizing them can be a pivotal step towards seeking timely medical intervention and potentially improving outcomes.
Read more about: Beyond ‘Toughing It Out’: 15 Critical Health Symptoms Men Must Never Ignore
5. **Persistent Upper Belly Pain Radiating to the Back**
Pain in the upper belly, particularly when it persistently radiates to the back, is a symptom that demands careful consideration as a potential warning sign of pancreatic cancer. This type of discomfort is frequently experienced by individuals with both acute and chronic pancreatitis, conditions that can be either linked to pancreatic cancer or increase its risk. The location and nature of this pain are critical clues for medical professionals to assess.
When a pancreatic tumor grows, especially those starting in the body or tail of the pancreas, it can become large enough to press on surrounding organs and nerves in the abdomen. This compression is a common cause of pain, which often begins in the upper abdomen and can then extend, or “radiate,” to the middle or upper back. The pain may not be constant; it can vary in intensity and may even feel worse after eating, when lying flat, coughing, exercising, or consuming more than usual.
Understanding how to manage this pain and when it becomes alarming is crucial. While sitting upright, leaning forward, curling into a ball, or eating less might offer some temporary relief, the key characteristic here is persistence and a lack of clear explanation. Unlike fleeting aches, this pain tends to linger and can signify an ongoing issue within the pancreas. Dr. Santhi Swaroop Vege, a gastroenterologist at Mayo Clinic, acknowledges that it is not feasible to investigate every instance of abdominal or back pain, but persistent, unexplained pain warrants medical attention.
Therefore, if you experience new or worsening upper belly pain that radiates to your back, especially if it doesn’t improve with typical remedies or is accompanied by other concerning symptoms, it’s imperative to consult your doctor. This symptom, while common to many less serious conditions, can be a vital indicator that requires a thorough medical evaluation, often involving imaging tests like a pancreas protocol CT scan, to determine its underlying cause.
Read more about: From Peril to Progress: Unearthing 13 Deadly 19th-Century Diseases Now Easily Curable
6. **Oily, Smelly Stools (Steatorrhea)**
A distinct change in bowel habits, specifically the appearance of oily, unusually smelly stools—medically known as steatorrhea—can be a significant, though often uncomfortable, indicator related to pancreatic health. This symptom arises directly from the pancreas’s vital role in digestion, particularly its production of enzymes necessary for breaking down fats. When these enzymes are insufficient, fats are not properly absorbed by the body.
The pancreas produces digestive juices, called enzymes, that are essential for breaking down food in the small intestine. If a pancreatic tumor obstructs the duct that delivers these enzymes, or if the cancer impairs the pancreas’s ability to produce them, fats pass through the digestive system undigested. This results in stools that are pale, greasy, bulky, and often float in the toilet bowl because of their high fat content. They may also appear to stick to the sides of the toilet and have a particularly foul odor.
This malabsorption of fats is not merely an unpleasant symptom; it can lead to significant nutritional deficiencies and unintended weight loss, as the body fails to extract necessary nutrients from food. The Mayo Clinic lists “oily, smelly stools” as a symptom of chronic pancreatitis, which itself is a risk factor for pancreatic cancer. Neuroendocrine tumors (NETs) of the pancreas, though rare, can also present with foul-smelling fatty stools, among other symptoms.
While several conditions can cause steatorrhea, its sudden onset or persistence, especially when coupled with other pancreatic cancer warning signs, should prompt a visit to your doctor. Describing the characteristics of your stool—whether it’s oily, floats, or has a distinct odor—can provide your doctor with crucial diagnostic information. This seemingly minor detail can be a direct clue that your pancreas is not functioning correctly, necessitating further investigation.

7. **Persistent Fatigue or Physical Weakness**
Feeling perpetually tired or experiencing unexplained physical weakness, even without significant physical exertion, is a common symptom across many health issues. However, when these feelings are persistent and cannot be attributed to typical causes like lack of sleep or stress, they become a crucial, albeit non-specific, warning sign of pancreatic cancer that should not be overlooked. Many people may dismiss this symptom, but its persistence can indicate an underlying medical problem.
Pancreatic cancer, like other serious illnesses, can induce a general state of malaise and fatigue through various mechanisms. The body expends significant energy fighting the cancer cells, leading to systemic inflammation and a feeling of being run down. Furthermore, the accompanying symptoms often seen in pancreatic cancer, such as loss of appetite, unintended weight loss, and malabsorption, can lead to malnutrition, further exacerbating feelings of weakness and exhaustion. The buildup of bilirubin in the body, which can occur with jaundice, also contributes to a general sense of unwellness.
Individuals experiencing persistent fatigue may also struggle with sleep disturbances or even develop depression, symptoms that can further impact their energy levels and overall well-being. The challenge with fatigue is that it can stem from countless benign causes, making it difficult for individuals to recognize its potential gravity. However, if this fatigue is profound, unremitting, and doesn’t improve with rest, it warrants a closer look by a healthcare professional.
While fatigue and weakness alone are rarely definitive of pancreatic cancer, their presence, especially when combined with other symptoms like unexplained weight loss, new-onset diabetes, or changes in digestive patterns, should serve as a prompt for medical consultation. Your doctor can help determine if there is an underlying condition affecting your energy levels and recommend appropriate diagnostic tests to rule out serious concerns.
Read more about: Unlock Restful Nights: 12 Simple Steps to Boost Your Sleep Quality by 50% in Under 1 Week

8. **Other Related Digestive Problems: Nausea, Vomiting, Bloating, and Early Fullness**
Beyond the more distinct symptoms discussed, pancreatic cancer can manifest through a cluster of general digestive problems that, while common, warrant attention when persistent or unexplained. These include nausea, vomiting, a feeling of bloating, and experiencing early fullness during meals. Individually, these symptoms might seem minor, but collectively, or in conjunction with other warning signs, they paint a more concerning picture regarding pancreatic health.
Nausea and vomiting can occur if a growing tumor compresses the stomach or other parts of the digestive tract, impairing the normal flow and digestion of food. Patients might feel particularly unwell right after eating, as their body struggles to process the meal. This mechanical obstruction can lead to a backlog of food and digestive juices, triggering feelings of sickness and subsequent vomiting, which can further contribute to malnutrition and weight loss.
Similarly, a sense of early fullness, or satiety, during meals, often accompanied by uncomfortable swelling in the abdomen, points to issues within the digestive system. This feeling of being “bloated or gassy” can also be caused by tumor compression on the stomach or intestines. It means that even a small amount of food can make a person feel uncomfortably full, deterring them from eating adequate amounts and potentially contributing to the unintended weight loss often associated with pancreatic cancer.
These digestive issues are frequently encountered in everyday life and can be attributed to diet, stress, or other minor conditions. However, their persistence, severity, or appearance alongside other signs like jaundice, unexplained weight loss, or changes in blood sugar, should never be ignored. As Dr. Santhi Swaroop Vege notes, it’s about recognizing the context and the combination of symptoms. If you find yourself consistently grappling with these digestive discomforts, it is important to discuss them thoroughly with your doctor.
Pancreatic cancer presents a formidable challenge in diagnosis due to its often-vague and late-appearing symptoms. However, by understanding and heeding these critical warning signs—from leg symptoms like DVT to digestive disturbances and systemic changes like jaundice, diabetes, weight loss, and persistent fatigue—we empower ourselves to act proactively. Early detection truly is the holy grail, offering the best chance for successful treatment. If any of these symptoms resonate with your experience, or if you have a combination of them, do not hesitate; consult your doctor immediately to ensure a comprehensive evaluation and peace of mind.





