Blood clots are a natural and essential part of the body’s defense mechanism. When you experience a cut or injury, these gel-like clumps of blood form rapidly to stop bleeding, transforming from a liquid to a semi-solid state. This vital process prevents excessive blood loss and initiates healing, showcasing the intricate efficiency of our circulatory system. Platelets, small cell fragments, play a key role in this coagulation process, forming a mesh over the injury site to stem the flow.
However, while crucial for wound repair, blood clots can sometimes form inappropriately inside veins or arteries, posing a significant threat to health. When these clots do not dissolve naturally after their job is done, or when they form without a direct injury, they can obstruct blood flow and lead to serious medical conditions. Such dangerous clots can result in life-threatening emergencies, including heart attacks, strokes, or pulmonary embolisms, by preventing oxygen from reaching critical organs.
Recognizing the warning signs of these potentially dangerous blood clots is paramount for timely medical intervention. Early detection can make a profound difference in outcomes, helping individuals avoid severe complications and remain out of the danger zone. This comprehensive guide will explore critical blood clot symptoms, paying particular attention to those that can manifest in your arm or leg, empowering you with the knowledge to act swiftly when necessary. Understanding these indicators, which vary depending on the clot’s location, is the first step in protecting your health.

1. **Swelling in One Limb**One of the most common and recognizable symptoms of a blood clot, especially a deep vein thrombosis (DVT), is unexplained swelling in a single limb. This swelling typically affects one arm or leg, occurring because the clot partially or completely obstructs the normal flow of blood back to the heart. This blockage causes fluid to accumulate in the tissues behind the obstruction, leading to a noticeable increase in the limb’s size. It is important to note that you can get blood clots in blood vessels in just about any part of your body.
The appearance of swelling from a blood clot can be quite sudden and is characteristically limited to one limb, making it asymmetrical compared to the other side. This unilateral nature is a key indicator that distinguishes clot-related swelling from more generalized fluid retention. For instance, if a blood clot forms in one of the deep veins in your leg, beneath the skin’s surface, the entire leg or just the specific area around the clot may swell up. This swelling can sometimes progress to “pitting edema” — a buildup of fluid that leaves a “pit” or dimple if you press on your leg.
While deep vein thrombosis is most commonly associated with the legs, particularly after prolonged periods of immobility such as post-surgery or during long plane trips, it can also affect the arms. Deep vein thrombosis in the arm, though less frequent, occurs more often in young, healthy people (especially athletes) after intense arm activity, such as wrestling, swimming, or repeated ball throwing. In these cases, your arm may suddenly swell up, much like a leg DVT.
It is crucial to understand that unexplained or asymmetrical swelling in an arm or leg warrants immediate medical attention. Swelling in the arm, even at its onset, can significantly interfere with strength and mobility, making it hard to ignore. While various causes can lead to limb swelling, such as local infection or compression of blood vessels or nerves, when there is no other apparent reason for it, and especially if accompanied by other signs, a blood clot should be strongly suspected and evaluated promptly by a medical professional. Prompt diagnosis is essential because, like a leg DVT, a DVT in your arm can also become a medical emergency.
Read more about: The Shocking Truth About Depreciation on the 2024 BMW iX: A Consumer Reports Deep Dive

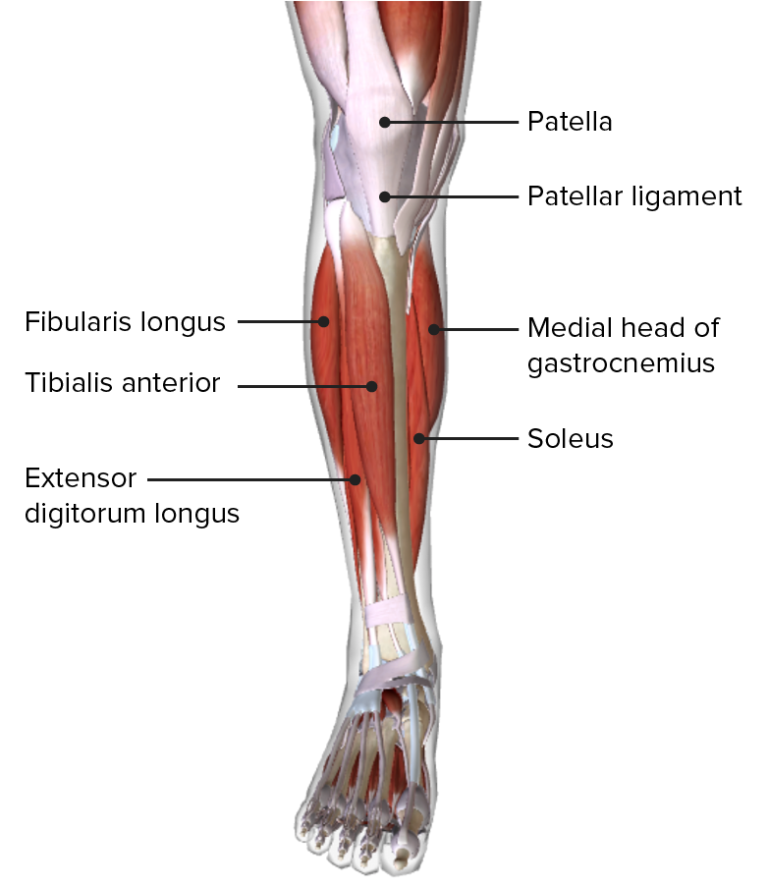
2. **Pain or Tenderness in the Affected Area**Another significant warning sign of a blood clot is the presence of pain or tenderness in the affected limb. This discomfort is often described as a cramp, a general soreness, or a throbbing sensation, and it typically localizes to the area where the clot has formed. When a deep vein thrombosis develops in the leg, the pain frequently originates in the calf or thigh, and this cramp might feel like a bad charley horse. For those experiencing a DVT in the arm, the pain might manifest as a general ache or a feeling of heaviness and tiredness.
A crucial distinguishing characteristic of clot-related pain is its persistence and nature. Unlike typical muscle pain or a common charley horse, the discomfort stemming from a blood clot does not typically subside with rest, stretching, or massage. In fact, the pain often intensifies over time as the clot grows or inflammation increases, and it may become noticeably worse when standing or walking for extended periods if the clot is in the leg. You may only feel pain when you stand or walk. This worsening with activity, coupled with a lack of relief from conventional methods, should raise immediate concern.
The severity of pain can vary; depending on the type and location of the blood clot, symptoms may be mild or quite severe. In some unfortunate instances, a DVT can even occur without any accompanying pain, making vigilance for other signs even more vital. However, if you experience new or worsening pain in a limb, particularly if it feels like a bad charley horse that doesn’t resolve, it is imperative to seek medical evaluation. Your arm may hurt and feel heavy and tired, and you might have trouble moving your arm.
This localized pain is a direct consequence of the clot obstructing blood flow and causing inflammation in the surrounding tissues. The pressure buildup and tissue irritation contribute to the characteristic sensations of a cramp or throbbing. Because such pain can escalate quickly and indicates a potentially dangerous situation, contacting your doctor right away or going to the emergency room is the recommended course of action if these symptoms develop, especially if they are persistent or worsening. Ignoring these signs can allow a DVT to progress and potentially lead to more severe complications.
Read more about: Behind the Workout: When Persistent Injuries Demand Professional Intervention

3. **Red or Discolored Skin**A visible change in the skin’s color over the affected area is a compelling indicator that a blood clot might be present. When a clot forms in a vein, the skin directly above it can become red or discolored, depending on your natural skin tone. This alteration in hue is a direct result of inflammation occurring around the clot and the restriction of normal blood flow to the area. The compromised circulation prevents oxygenated blood from reaching the capillaries efficiently and hinders deoxygenated blood from returning, leading to characteristic color changes.
The discoloration can manifest in various ways, from a distinct redness or purple tint to the skin appearing unusually pale or even having a blue cast. In some cases, the affected area might resemble a bruise or appear darkened, suggesting compromised circulation. For deep vein thrombosis in the arm, the skin on your arm may change colors, appearing red or purple, or your skin may be pale or have a blue tint. Similarly, in a leg DVT, your affected leg may change color — red or purple — depending on your skin color. Any sudden or unexplained change in skin tone, particularly when localized to one limb and accompanied by other symptoms, should be taken seriously and investigated.
This symptom often appears in conjunction with other signs such as warmth and swelling, forming a constellation of indicators that point towards a DVT. The inflammation caused by the clot directly contributes to the redness as blood vessels near the surface become engorged. The stagnant blood flow also affects the oxygenation of the tissues, leading to a bluish or purplish discoloration, particularly noticeable in individuals with lighter skin tones. For those with darker skin, these changes might be more subtle, appearing as a darker, purplish, or greyish area.
It is crucial not to dismiss these skin changes as minor or superficial. A discolored limb is a visual alarm signaling that something is impeding healthy blood circulation. Whether the skin appears red, purple, pale, or blue, these are vital clues that underscore the need for prompt medical evaluation. Visible veins in your arm and chest that may stand out more than usual or even bulge can also be an accompanying sign of an arm DVT, further indicating compromised venous return. Such symptoms are critical alerts that demand immediate professional medical assessment to diagnose the underlying cause and initiate appropriate treatment.
Read more about: Bring Back the Black: Your Expert 12-Step Guide to Restoring Faded Plastic Trim on Any Car
4. **Warmth in the Skin**Experiencing unusual warmth in a specific area, typically in the arm or leg where a blood clot is present, is another significant warning sign of a deep vein thrombosis. This localized increase in skin temperature occurs because the blood clot triggers an inflammatory response in the surrounding tissues. The body’s immune system reacts to the obstruction and irritation caused by the clot, leading to localized inflammation that manifests as increased heat.
This warmth is often felt as the affected skin being distinctly hotter than the skin on the unaffected limb or other areas of the body. When you touch the skin on your leg with the DVT, for example, it may feel warmer than other skin. This sensation of heat is a direct physiological consequence of the body’s efforts to respond to the blockage and can be a subtle yet powerful indicator that a clot is forming or has formed within the deeper veins. It is a sign that the body is under stress due to the circulatory disruption.
The symptom of warmth rarely occurs in isolation. It is frequently observed in conjunction with other classic signs of a blood clot, such as redness or discoloration of the skin and swelling in the affected limb. This triad of warmth, redness, and swelling forms a particularly strong indicator of a DVT. When these symptoms collectively appear in one arm or leg, they strongly suggest the presence of an underlying blood clot that requires urgent attention.
Considering the potential seriousness of a blood clot, any unexplained warmth in a limb, especially when accompanied by other warning signs, should prompt immediate action. This is not a symptom to “wait and see” about. Medical advice from a healthcare professional is crucial. The presence of warm skin is a tangible physical sign of an internal process that needs to be assessed quickly to prevent the clot from growing, breaking loose, or causing permanent damage. Therefore, it is important to call your doctor immediately or visit emergency care right away if you detect this symptom, alongside others mentioned.
Read more about: Beyond the Bloating: Essential Warning Signs of Ovarian Cysts, Including Lower Back Pain, You Should Understand
5. **Leg Fatigue or Heaviness**Individuals who develop blood clots in their legs may experience a distinct feeling of fatigue, heaviness, or aching in the affected limb. This sensation is more than just general tiredness; it often feels like a persistent, unyielding weight or dull ache that is specifically isolated to one leg. This symptom arises because the blood clot obstructs venous return, causing blood to pool in the veins and increasing pressure within the affected limb. The compromised circulation and increased pressure lead to muscle fatigue and a sensation of profound heaviness.
The fatigue or heaviness associated with a blood clot typically worsens with activity and improves with rest or elevation. This characteristic pattern can help differentiate it from ordinary muscle soreness, which might improve with activity or gentle stretching. As the clot grows larger or as inflammation in the vein increases, this feeling of heaviness can become more pronounced and debilitating, making everyday movements difficult and uncomfortable. The feeling can be subtle at first but may progress as the clot grows or inflammation increases.
At its onset, this symptom can be subtle and might be easily mistaken for general tiredness, muscle strain from overuse, or even the effects of aging. However, the key differentiator is its unilateral nature and its persistence without an obvious cause like recent strenuous exercise. This symptom is sometimes mistaken for general tiredness or overuse, which is why it’s important to assess whether the sensation is isolated to one leg. If the sensation of heaviness or fatigue is persistently isolated to one leg and does not resolve as expected, it warrants closer inspection.
Understanding that a heavy or achy feeling in one leg can be a harbinger of a serious underlying condition is vital. It underscores the importance of being attuned to changes in your body and seeking professional medical evaluation when these symptoms arise without clear explanation. Your doctor can conduct the necessary tests, such as an ultrasound, CT scan, and even a blood test, to determine the exact cause of your discomfort and provide appropriate guidance and treatment, ensuring that what might seem like a minor inconvenience isn’t a sign of a more serious, developing health threat.
Read more about: Eat Cleaner, Sleep Deeper: The 10 Worst Dinner Choices Disrupting Your Rest, According to Sleep Experts
6. **Sudden Shortness of Breath**When a blood clot, often originating in an arm or leg, breaks free and travels to the lungs, it can cause a life-threatening condition called a pulmonary embolism (PE). This severe event occurs when the clot obstructs blood flow within the lung’s arteries, preventing oxygen from reaching the blood effectively. Recognizing the warning signs of a PE is critically important, as it demands immediate medical treatment to prevent severe complications or even a fatal outcome.
One of the most alarming and prominent symptoms of a pulmonary embolism is the sudden onset of unexplained shortness of breath or trouble breathing. This feeling is not a gradual change; it can come on very quickly and unexpectedly, even when an individual is at complete rest. Furthermore, this shortness of breath often worsens significantly with any form of physical exertion, making even simple daily tasks feel overwhelmingly difficult.
This sudden inability to catch your breath is a direct and urgent signal that your body’s oxygen supply is severely compromised due to the arterial blockage in the lungs. If you experience such abrupt difficulty breathing, especially if it’s accompanied by other concerning symptoms like sharp chest pain or a persistent cough, it is crucial to seek emergency medical attention without any delay. Prompt intervention can truly make the difference in saving a life and preserving lung function.
Read more about: Beyond Jaw Pain: Essential Heart Attack Warning Signs You Must Never Overlook, Especially for Women
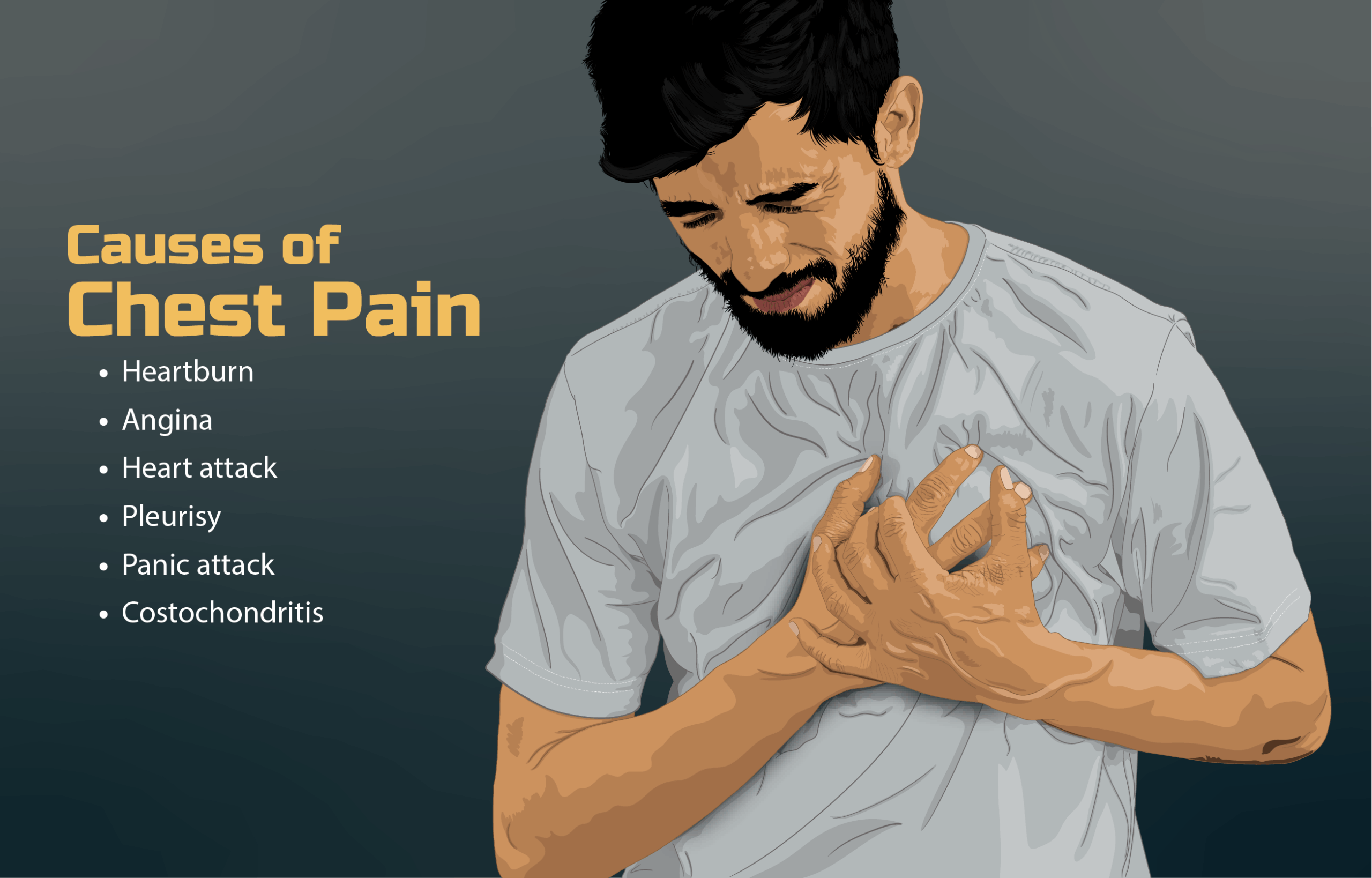
7. **Chest Pain**Another critical warning sign that may strongly indicate a pulmonary embolism is the presence of chest pain, which can be quite severe. This discomfort associated with a PE often manifests as a sharp, stabbing sensation or a feeling of heavy pressure within the chest. It is particularly concerning because this pain tends to intensify markedly when taking a deep breath or when coughing, further exacerbating respiratory distress.
While any form of chest pain should always be taken seriously, it’s important to recognize characteristics that might distinguish PE-related pain. Unlike the generalized crushing or squeezing sensation often associated with a heart attack, the chest pain from a pulmonary embolism is typically more localized and presents as an acute, sharp discomfort. However, due to the potential for significant symptom overlap with other serious cardiac or respiratory conditions, it is absolutely essential to treat any new or unexplained chest pain as a medical emergency until its underlying cause has been definitively determined by a qualified healthcare professional.
The sudden onset of such chest pain, especially when paired with shortness of breath, a rapid heartbeat, or any other related systemic symptoms, necessitates immediate medical evaluation. This persistent pain is a direct indication of severe stress on the cardiovascular system and profoundly impaired lung function due to the presence of the blood clot. Delaying medical attention in such a situation can have dire and life-threatening consequences, highlighting the absolute importance of swift and decisive action.
Read more about: Beyond Jaw Pain: Essential Heart Attack Warning Signs You Must Never Overlook, Especially for Women

8. **Coughing (Possibly with Blood)**A sudden, unexplained cough can also serve as a significant indicator of a blood clot that has traveled to the lungs, culminating in a pulmonary embolism. This cough may present in different forms; it could be a dry, persistent hacking cough, or it might be productive, meaning it produces mucus. The sudden appearance of such a cough, without a clear preceding illness or explanation, warrants careful attention.
In more severe and concerning instances of a pulmonary embolism, the cough can even produce sputum that is tinged with blood, a symptom medically known as hemoptysis. The appearance of blood in your mucus, even in small amounts, is a serious medical sign that should never be ignored or dismissed. It signifies that the delicate tissues within the lungs may be damaged or irritated due to the clot’s presence and the subsequent lack of adequate blood flow. This symptom serves as an urgent alert requiring immediate medical investigation.
When a cough is accompanied by other critical symptoms of a pulmonary embolism, such as sharp chest pain, a rapid or irregular heartbeat, or particularly, sudden shortness of breath, it forms a constellation of signs that strongly points towards a life-threatening emergency. In such cases, seeking emergency medical care without hesitation is paramount for survival and recovery. These combined symptoms unequivocally indicate a severe blockage affecting both the respiratory and circulatory systems, demanding rapid intervention to mitigate potential and severe harm.
9. **Rapid Heartbeat or Palpitations**A blood clot lodged in the lungs, specifically a pulmonary embolism, can force the heart to work considerably harder than usual to pump blood through the obstructed vessels. This increased effort and strain on the heart often results in a rapid or irregular heartbeat, a symptom commonly referred to as palpitations. Individuals may describe this sensation as a fluttering in the chest, a racing heart, or a strong, unusually noticeable pounding feeling.
While experiencing heart palpitations can stem from a wide array of causes, many of which are benign, their sudden occurrence in the context of other potential blood clot symptoms should raise an immediate and serious alarm. If you notice a rapid or irregular heartbeat alongside sudden shortness of breath, unexplained dizziness, or acute chest pain, these combined indicators strongly suggest a more serious underlying issue that requires urgent investigation. The heart’s altered rhythm is a profound physiological response to the severe stress placed upon it by the compromised blood flow and reduced oxygenation.
The body’s intricate circulatory system is designed for efficient and continuous blood flow. Any significant obstruction, especially one affecting the critical lung vasculature, can severely disrupt this delicate balance. A racing heart under these circumstances is a clear signal that the body is struggling intensely to maintain adequate oxygen supply to vital organs. Therefore, any unexplained rapid heartbeat, particularly when coupled with other warning signs, mandates prompt medical evaluation to rule out a life-threatening pulmonary embolism and initiate necessary, timely treatment.
Read more about: Beyond Fatigue: Crucial Thyroid Disorder Symptoms You Should Never Overlook, Including Early Signs That Begin in Your Hair and Skin
10. **Dizziness or Fainting**In severe cases, a blood clot, particularly a large pulmonary embolism obstructing significant lung blood flow, can lead to a sudden and precipitous drop in blood pressure. This abrupt decrease in systemic pressure can manifest as symptoms such as dizziness, lightheadedness, or, in more extreme instances, actual fainting. These symptoms are critical early indicators of a serious problem with the body’s circulation and its ability to oxygenate vital tissues effectively. When the brain does not receive sufficient oxygenated blood, these profound neurological signs become readily apparent.
Fainting, medically known as syncope, is an especially alarming and serious symptom that demands immediate attention. Its occurrence, particularly when combined with other critical indicators such as chest discomfort, rapid heartbeat, or difficulties with breathing, serves as a major red flag for an urgent medical situation. It unequivocally signifies a profound disruption in the body’s ability to maintain consciousness due to severely impaired blood flow and oxygen delivery to the brain. Such an event could indicate not only a pulmonary embolism but also potentially a stroke, especially if accompanied by signs like a sudden loss of balance, facial drooping, or one-sided weakness.
Recognizing dizziness or fainting as a potential symptom of a dangerous blood clot is absolutely crucial. These are not minor inconveniences but clear signals of a severe systemic issue that could rapidly escalate to a life-threatening crisis. If you or someone you are with experiences these symptoms, especially in conjunction with any other warning signs discussed in this guide, immediate emergency medical attention is absolutely vital. Swift action can prevent further damage to organs and potentially save a life by addressing the underlying circulatory crisis with urgency and expertise.
**Risk Factors and When to Seek Immediate Medical Attention**
While vigilance for the distinct warning signs of blood clots is crucial for everyone, it is particularly important for individuals who fall into certain heightened risk categories. Understanding these specific factors can empower you to be more proactive in seeking timely medical care. Key risk factors include prolonged periods of immobility, such as during long flights or extended hospital stays, and undergoing major surgery, especially procedures involving the legs, hips, or abdomen. Pregnancy and the postpartum period also notably increase susceptibility, as do hormonal birth control or hormone replacement therapy, and the presence of a broken bone.
Furthermore, certain lifestyle choices and underlying medical conditions play a significant role in increasing risk. Smoking, obesity, a family history of blood clots or clotting disorders, and the presence of cancer or undergoing cancer treatments all significantly elevate the risk profile. Age, while not a direct cause, can be a contributing factor, as blood clots regrettably do not discriminate based on age. If you find yourself in any of these elevated risk categories and begin to notice any of the aforementioned symptoms, it is even more imperative to seek prompt and thorough medical evaluation.
The single most crucial piece of advice regarding potential blood clots is this: absolutely do not take a “wait and see” approach if you even remotely suspect one. Blood clots possess the dangerous potential to evolve into life-threatening emergencies within a matter of hours, leading to severe and irreversible complications like a debilitating stroke, a catastrophic pulmonary embolism, or a fatal heart attack. Your best and most effective defense against these grave outcomes is immediate, decisive action. If you experience any combination of the warning signs discussed, or if a single symptom is severe, persistent, and unexplained, seek emergency medical attention without hesitation or delay.
Read more about: Beyond the Bloating: Essential Warning Signs of Ovarian Cysts, Including Lower Back Pain, You Should Understand
Your personal awareness and swift response can truly be the difference between life and death. Being acutely attuned to your body’s subtle signals and understanding precisely when to act is paramount in safeguarding your health and preventing potentially devastating outcomes. Do not delay, do not dismiss; your informed vigilance could critically save your life or the life of someone you deeply care about by ensuring timely diagnosis and immediate, appropriate treatment.