Embarking on the journey of drug development is an endeavor fraught with complexity, significant investment, and rigorous scientific scrutiny. It’s a methodical process, meticulously designed to ensure that any new medical intervention—be it a drug, vaccine, or device—is not only effective against its target condition but also safe for human use. For anyone interested in how innovative treatments reach patients, understanding these distinct clinical research phases is absolutely fundamental.
This intricate process, often spanning many years and costing billions, moves from initial laboratory and animal testing through several stages involving human volunteers and patients. Each phase builds upon the last, progressively gathering more comprehensive data on safety, dosage, efficacy, and potential side effects. It’s a carefully choreographed dance between scientific discovery and patient well-being, designed to mitigate risks while maximizing therapeutic benefits.
In this practical guide, we’ll demystify the critical stages of clinical research, providing a clear roadmap from the lab bench to initial human trials. We’ll break down what each phase entails, its primary objectives, the types of studies conducted, and the pivotal questions researchers aim to answer, offering a hands-on understanding of this vital pathway in medical innovation.
1. **Preclinical Research: Laying the Essential Groundwork**Before any promising new drug or medical intervention can even be considered for human testing, it must first undergo extensive preclinical research. This foundational stage is entirely conducted without human subjects, serving as a critical gatekeeper in the drug development process. Its primary purpose is to determine whether a candidate drug has sufficient potential to warrant the significant investment and ethical considerations of human clinical trials, ultimately becoming an Investigational New Drug (IND).
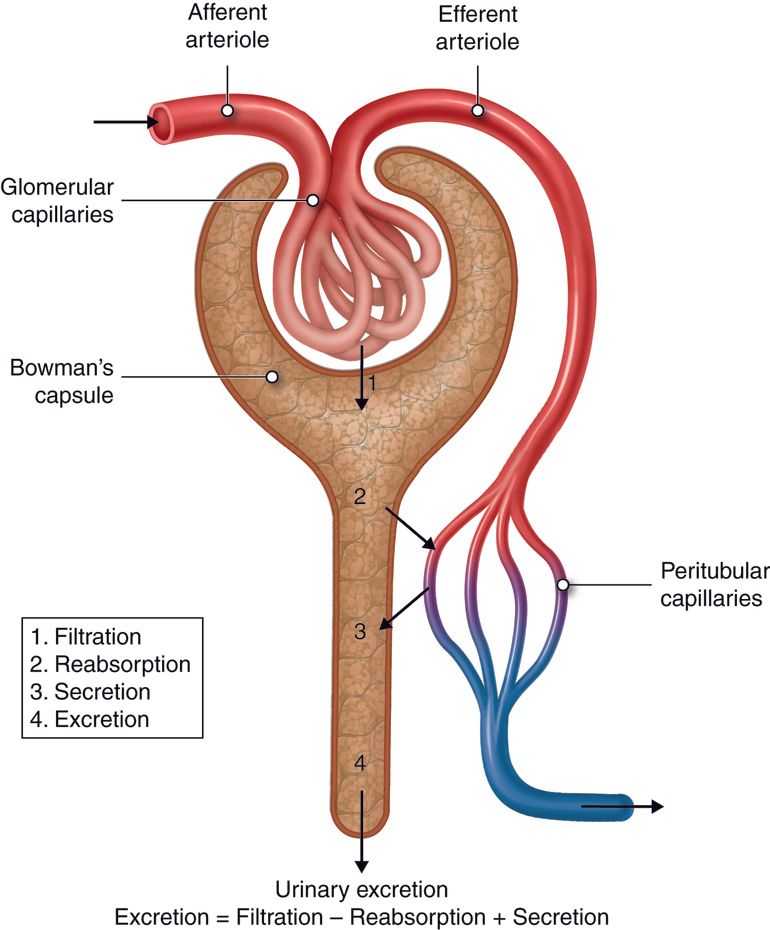
Preclinical studies involve a wide array of tests, typically exploring a broad range of doses to understand the compound’s initial behavior. These investigations are divided into two main categories: *in vitro* experiments, which are conducted in a test tube or using cell cultures, and *in vivo* experiments, which involve model animals. These tests are meticulously designed to gather preliminary information regarding the drug’s potential efficacy, its toxicity profile, and its pharmacokinetics – essentially, what the body does to the drug.
The pharmacokinetic data collected at this stage provides crucial insights into how the drug is absorbed, distributed, metabolized, and excreted by the body. Simultaneously, toxicology studies help identify any adverse effects or harmful properties the compound might possess before it ever enters a human system. This comprehensive testing allows researchers to make informed decisions about whether a candidate drug has the safety and therapeutic promise to proceed to the next, more complex stages of clinical development.

2. **Phase 0 Clinical Trials: Microdosing for Early Human Insights**Phase 0 clinical trials represent a relatively newer, optional, and exploratory stage in the drug development pipeline. Introduced under the U.S. Food and Drug Administration’s (FDA) 2006 exploratory Investigational New Drug (eIND) guidelines, these trials are often referred to as human microdosing studies. Their innovative design aims to accelerate the development of promising drugs by providing very early insights into a compound’s behavior in humans.
These trials are characterized by several distinct features. They involve only a small number of subjects, typically between 10 to 15 individuals, who receive a single, subtherapeutic dose of the investigational drug. This microdose is significantly lower than what would be expected to produce any therapeutic effect or cause significant side effects, often less than 1/100th of the dose anticipated to produce a pharmacological effect, and usually not exceeding 100 micrograms. The duration of these studies is also notably short, often completed within six months, with multi-dose studies generally not exceeding seven days.
The primary objective of Phase 0 trials is to gather preliminary pharmacokinetic data, such as oral bioavailability and half-life, and to ascertain whether the drug’s performance in humans aligns with expectations derived from preclinical research. While these studies do not provide data on drug safety or efficacy due to the extremely low doses, they are invaluable for ranking and evaluating candidate drugs. By allowing drug developers to screen the most promising compounds using human models, Phase 0 can sometimes predict pharmacokinetic behavior that animal models alone might not accurately forecast, thereby streamlining the selection of compounds for further, more intensive development.

3. **Phase I Clinical Trials: The First Steps into Human Safety and Dosing**Clinical trials formally commence with Phase I, historically known as the ‘First in Human’ (FIH) studies. This is the initial stage where an investigational drug is administered to human subjects, making safety the paramount concern. The primary goals of Phase I trials are to evaluate the drug’s safety, identify potential side effects, determine the optimal dose range, and assess the most suitable formulation for future studies.
Typically, Phase I trials recruit a small group of 20 to 100 participants. For most new drugs, these subjects are healthy volunteers, as their stable physiological state helps researchers isolate the drug’s direct effects without interference from pre-existing conditions. However, in specific scenarios where the drug is highly toxic or intended for a specific patient population, such as advanced cancer or HIV patients, the trials may exclusively enroll individuals with the target disease. These trials are generally non-randomized, meaning subjects are not randomly assigned to different treatment groups, which can introduce some selection bias but is often acceptable given the safety-focused objective.
These crucial studies are commonly conducted in specialized clinical trial centers, often managed by Contract Research Organizations (CROs). These centers are equipped with dedicated personnel who continuously monitor the subjects’ conditions. Following drug administration, participants are observed over several drug half-lives to thoroughly assess safety (pharmacovigilance), tolerability, pharmacokinetics (what the body does to the drug), and pharmacodynamics (what the drug does to the body). Before any Phase I trial can begin, an Investigational New Drug (IND) application, detailing comprehensive pharmacological data from cellular and animal models, must be submitted to regulatory authorities like the FDA.
4. **Sub-phases of Phase I: Precision in Dose Determination**Phase I trials are not monolithic; they often incorporate several specialized sub-phases to meticulously determine the drug’s safety profile and optimal dosing. These include Single Ascending Dose (SAD) studies, Multiple Ascending Dose (MAD) studies, and Food Effect studies, each providing distinct yet complementary information critical for a new drug’s progression.
Single Ascending Dose (SAD), also known as Ia phase, involves administering a single dose of the drug to small groups of subjects, typically around three individuals per group. Following administration, these subjects are closely monitored over a specific period for safety, while pharmacokinetic data is collected to understand how their bodies process the drug. If no unacceptable side effects are observed and pharmacokinetic data remains within safe thresholds, a new group of subjects receives a higher dose. This dose-escalation process continues until either the dose reaches a pre-determined pharmacokinetic safety level or subjects begin to experience unacceptable toxicity, at which point the maximum tolerated dose (MTD) is identified. Though variations exist, the general design assumes the MTD is the dose at which approximately one-third of subjects experience unacceptable toxicity.
Conversely, Multiple Ascending Dose (MAD), or Ib phase, studies focus on the pharmacokinetic and pharmacodynamic properties of the drug under repeated dosing. In these trials, a group of subjects receives multiple low doses over a set period. Biological samples, such as blood and other bodily fluids, are collected at various time points and analyzed to gather comprehensive pharmacokinetic attributes, including ADME (absorption, distribution, metabolism, and excretion) properties. Similar to SAD, the dose is incrementally increased in subsequent groups until the desired level is reached or unacceptable toxicity emerges. A critical aspect of MAD trials is assessing whether there is any drug accumulation in the body with repeated administration.
Finally, Food Effect studies are short-term experiments designed to investigate how ingesting food before drug administration might influence drug absorption or alter its pharmacokinetics. Given that food can significantly impact a drug’s absorption rate and overall pharmacokinetic profile—data that is crucial for predicting its real-world behavior—these studies are essential. Typically designed as crossover trials, volunteers take the same dose of the drug under both fasted and fed conditions, usually involving at least 12 subjects. Increasingly, to streamline costs and development timelines, pharmaceutical companies often integrate a preliminary assessment of food effects into their SAD or MAD trials by adding extra cohorts, providing an early evaluation of this important factor.
5. **Phase II Clinical Trials: Evaluating Efficacy and Side Effects**Once a drug has successfully navigated the safety and preliminary dosing assessments of Phase I, it progresses to Phase II clinical trials. This stage marks a pivotal shift in focus; while safety continues to be monitored, the primary objective here is to evaluate the drug’s biological activity, or efficacy, and its effectiveness in patients suffering from the specific disease it aims to treat. This phase is often described as the ‘treatment effect exploration’ or ‘optimal dose finding’ stage.
Phase II trials enroll a larger cohort of participants compared to Phase I, typically ranging from 50 to 300 individuals. Crucially, these participants are all patients diagnosed with the particular disease or medical condition targeted by the drug. Researchers often select patients with as few other confounding conditions as possible to ensure that any observed effects can be primarily attributed to the investigational drug. The aim is to find the minimum effective dose that provides positive therapeutic outcomes while minimizing side effects, thereby ensuring a favorable risk-benefit ratio.
To ensure robust data, Phase II clinical trials commonly employ rigorous study designs, frequently using randomized double-blind controlled trials. In such designs, some patients receive the investigational drug, while others receive a placebo or the current ‘standard of care’ treatment, without either the patients or the researchers knowing who is receiving which treatment. This helps minimize bias and provides a clearer picture of the drug’s true therapeutic effect. Despite these careful designs, Phase II is notorious for high failure rates, often stalling due to the drug’s inability to achieve pharmacodynamic targets or the emergence of unexpected toxic reactions. Genetic polymorphism studies are sometimes incorporated at this stage, especially when there’s evidence of individual differences in drug metabolism, to better understand patient response variability.

6. **Sub-phases of Phase II: Proving Concept and Pinpointing the Dose**To refine the understanding of a drug’s effectiveness and to precisely tailor its application, Phase II clinical trials are often subdivided into IIa and IIb. While there are no rigid formal definitions for these sub-categories, they serve distinct yet interconnected purposes in the journey toward confirming a drug’s therapeutic value.
Phase IIa studies are typically referred to as ‘Proof of Concept’ (POC) studies. Their primary aim is to provide a preliminary demonstration of the drug’s clinical efficacy or biological activity in a relatively small number of patients, usually between 20 to 200 individuals. These studies focus on early efficacy endpoints to quickly ascertain if the drug exhibits the anticipated clinical effect. If these initial findings are promising, indicating that the drug indeed has the desired biological activity, then the development progresses to Phase IIb, involving a larger cohort of patients for more comprehensive evaluation.
Following a successful IIa phase, Phase IIb, or ‘Dose Finding’ (DF) studies, are initiated. The central goal here is to determine the optimal clinical dose that not only demonstrates biological activity but also has minimal side effects. These studies place a greater emphasis on evaluating efficacy across different dosages, meticulously seeking the ideal balance between therapeutic benefit and adverse reactions. Furthermore, IIb studies can serve as a crucial bridge to Phase III, addressing any potential changes in dosing requirements that might arise from differences in formulation, crystalline form, or salt type between earlier and later trial stages. These larger, more detailed studies are frequently designed as double-blind, randomized, controlled, multi-center trials.
In the context of cancer drug development, for instance, Phase II studies often incorporate a specific design to efficiently screen out low-activity drugs. Researchers might establish a minimum activity threshold, such as requiring the drug to show activity in at least 20% of subjects. If the estimated activity falls below this benchmark, the study might be abandoned or not proceed at the maximum tolerated dose. Conversely, if the activity surpasses 20%, more subjects are recruited to obtain a more precise estimate of the response or remission rate. Thus, typical cancer Phase II clinical studies often recruit fewer than 30 patients to estimate efficacy, making this stage a lean yet critical decision point in the development pathway.
Having explored the foundational stages of drug development, from preclinical research to the nuanced sub-phases of Phase II, we now transition to the pivotal, large-scale studies that confirm a drug’s therapeutic value. This next leg of the journey scrutinizes extensive patient populations, delves into the substantial financial and temporal investments required, examines the critical success rates that shape the industry, and highlights modern adaptive designs that are revolutionizing clinical research. Ultimately, we will look beyond market approval to the ongoing vigilance that ensures long-term safety and effectiveness.
7. **Phase III Clinical Trials: The Definitive Efficacy and Safety Confirmation**Once a drug has demonstrated promising efficacy and a manageable safety profile in Phase II, it progresses to Phase III clinical trials, often referred to as the ‘treatment effect confirmation stage’ and ‘pre-market research.’ This is the largest and most expensive stage of clinical development, designed to comprehensively evaluate the drug’s efficacy and safety in a broad patient population, solidify its optimal dosage, and confirm its value in clinical practice. The data gathered here is crucial for regulatory submission and, ultimately, for bringing the drug to patients.
These trials involve a large patient group, typically ranging from 300 to 3,000 individuals, or even more, depending on the specific disease or medical condition being studied. All participants are patients randomized into controlled, multi-center trials. A primary objective is to compare the new intervention against the current ‘gold standard’ treatment or a placebo, definitively assessing its therapeutic benefits, side effects, potential drug interactions, possible contraindications, and its overall impact on patient quality of life and health economics.
Given their scale and duration—often spanning two to five years—Phase III trials are the most complex to design and operate. They significantly increase participants’ exposure to the investigational drug, allowing for a more thorough assessment of its long-term safety and efficacy across diverse patient demographics, including variations in , age groups, ethnicities, and patients with co-existing conditions. These trials are critical for providing the robust evidence needed to support a new drug application.
Typically, regulatory agencies like the U.S. FDA or the European Medicines Agency (EMA) require data from at least two successful Phase III clinical trials to grant marketing approval. The comprehensive findings from these trials, alongside preclinical and earlier human study data, manufacturing processes, formulation details, and stability information, are compiled into a ‘regulatory submission.’ This extensive dossier is then submitted to the appropriate authorities for their meticulous review and, hopefully, subsequent approval for the drug’s production and sale.

8. **Sub-phases of Phase III: Strategic Extensions and Label Expansion**Just as Phase I and II have their sub-divisions, Phase III trials also include distinct sub-phases—IIIa and IIIb—which serve strategic purposes around the critical period of regulatory submission and initial market entry. While not always formally defined in every context, these distinctions help manage the evolving data needs and commercial objectives for a new drug.
Phase IIIa studies are typically conducted prior to the submission of a New Drug Application (NDA) to regulatory bodies. The main goal of these studies is to gather even more efficacy and safety data by administering the investigational drug to patients who have the specific treatment indication. This additional data provides a more robust evidence base, bolstering the information package submitted to regulators and helping to address any lingering questions about the drug’s profile before a final decision on approval.
Conversely, Phase IIIb studies are generally initiated after the regulatory submission has been made but before the drug receives final marketing approval and is put into production. These trials focus on acquiring supplementary efficacy and safety results, often delving into aspects such as the drug’s economic impact or its effect on patients’ quality of life. Significantly, IIIb studies also play a crucial role in ‘label expansion,’ where a drug that is already approved for one indication is investigated for new clinical uses, or an existing active ingredient is studied for new dosages or combinations. These studies help to support additional marketing claims or to collect further safety data for these new applications.

9. **Adaptive Designs: Agile Approaches to Clinical Research**In an effort to streamline drug development and respond more dynamically to emerging data, modern clinical research often employs ‘adaptive designs.’ These innovative trial methodologies allow for pre-specified modifications to a study’s design during its conduct, typically occurring within Phase II or III, based on interim results and sophisticated statistical analysis. This flexibility represents a significant departure from traditional, rigid trial designs and offers several strategic advantages.
The core principle behind adaptive design is to optimize the trial by making adjustments as new information becomes available. This could involve modifying the study protocol, adjusting patient randomization ratios, altering dosages, or even terminating unsuccessful designs early. Such adaptability aims to accelerate the development process, minimize the resources spent on less promising treatments, and enhance the likelihood of success for viable drug candidates, ensuring that research efforts are as efficient and effective as possible.
The benefits of adaptive designs are manifold. They can significantly shorten trial times and often require fewer subjects, which translates into reduced costs and faster timelines for drug development. Furthermore, the ability to stop a trial early if a drug is clearly ineffective or, conversely, exceptionally effective, protects patients and ensures resources are used wisely. Prominent examples include large-scale international trials like the World Health Organization’s Solidarity trial, Europe’s Discovery trial, and the UK’s Recovery Trial for COVID-19, all of which successfully leveraged adaptive designs to rapidly modify experimental treatment strategies in response to real-time data. This flexible approach also facilitates the coordination of design changes across international multi-center trials, bringing greater harmony and efficiency to global drug development efforts.

10. **Success Rates and Development Challenges: A Risky Endeavor**The journey through clinical development is fraught with significant challenges, and the probability of a new drug successfully navigating all phases to market approval remains remarkably low. Historically, drug development projects from Phase I to FDA approval have an average success rate of just 7.9%. This substantial attrition rate underscores the immense risk and investment inherent in pharmaceutical innovation, making each successful drug a testament to rigorous scientific perseverance.
Failure rates are particularly high in Phase II, which often stalls due to the drug’s inability to achieve its pharmacodynamic targets or the emergence of unexpected toxic reactions. Only about 28.9% of drug candidates successfully transition from Phase II to Phase III. Even at the advanced stage of Phase III, approximately 50% of candidate drugs fail or are rejected by regulatory authorities. This high rate of failure in later stages is especially impactful given the escalating costs and time investments as drugs progress through development.
Success rates also vary dramatically depending on the disease area being targeted. For instance, a review from 2019 revealed that cancer drug clinical trials had an average success rate of merely 3% between 2005 and 2015, highlighting the formidable complexities of oncology research. In stark contrast, drugs for eye diseases and infectious disease vaccines showed higher success rates, averaging around 33%. The use of disease biomarkers, particularly in cancer research, has been shown to improve success rates compared to trials not utilizing these biological indicators, offering a glimmer of hope for more targeted and efficient development pathways in challenging therapeutic areas. For example, in cancer Phase II studies, researchers often set a minimum activity threshold, abandoning drugs that fall below this benchmark to efficiently screen out low-activity compounds.
11. **The Substantial Investment: Time and Capital**Bringing a new drug from the initial preclinical research stage to market approval is not only a scientific marathon but also an economic one, often consuming vast amounts of time and capital. The entire drug development process, from discovery to market launch, typically spans an arduous 12 to 18 years and frequently incurs costs exceeding a staggering $1 billion. This ‘three tens’ principle—10 years, $10 billion, 10% success—though a generalization, powerfully illustrates the industry’s investment landscape.
Breaking down the timeline further, the clinical research phases themselves account for a significant portion of this duration. On average, Phase I clinical trials take about 2.3 years, followed by Phase II at 3.6 years, and Phase III consuming another 3.3 years. The subsequent regulatory approval phase typically adds another 1.3 years. This means, from the start of Phase I to eventual FDA approval, the journey often extends for an average of 10.5 years, a testament to the methodical and protracted nature of scientific validation.
The financial outlay for these later stages is equally daunting. Phase II research, where initial efficacy is explored, can cost up to $20 million per drug candidate. As trials scale up dramatically for comprehensive confirmation, Phase III studies become substantially more expensive, with costs potentially soaring to as much as $53 million. These figures underscore why late-stage failures are so financially devastating for pharmaceutical companies, making meticulous planning and robust scientific rigor paramount at every step.
Read more about: Navigating the AI Frontier: OpenAI’s Billion-Dollar Bets and the Global Stakes
12. **Phase IV Clinical Trials: Post-Market Vigilance and Real-World Impact**Even after a drug successfully navigates the rigorous gauntlet of Phase I, II, and III trials and receives regulatory approval, its journey of evaluation is far from over. This is where Phase IV clinical trials, also known as ‘post-market surveillance’ or ‘drug monitoring trials,’ come into play. This crucial stage aims to ensure the long-term safety and effectiveness of the drug, vaccine, device, or diagnostic test in the real-world setting, as it is used by a much larger and more diverse patient population over an extended period.
Phase IV studies encompass ongoing safety monitoring, a process known as pharmacovigilance, and continuous technical support for the marketed drug. These trials are conducted for various reasons: they can be a mandatory requirement from regulatory agencies, driven by industry competition to identify new market needs or expanded uses, or initiated to address gaps in earlier trial data, such as drug interactions or effects on specific populations (e.g., pregnant women or children) not comprehensively studied in pre-market phases. Unlike the earlier, more controlled trials, Phase IV collects data on a drug’s performance in actual clinical practice, under less idealized conditions.
A critical aspect of Phase IV is its ability to detect rare adverse reactions or long-term side effects that might not have emerged in the smaller, shorter-duration Phase I-III trials. With the drug now available to thousands or even millions of patients, subtle or infrequent safety concerns can become apparent. Discoveries made during Phase IV can have significant consequences, potentially leading to a drug’s market withdrawal or restrictions on its clinical use. Historic examples include cerivastatin (Baycol), troglitazone (Rezulin), and rofecoxib (Vioxx), which were either withdrawn or had their use severely limited due to post-market safety concerns.
It is important to note that while Phase IV clinical trials represent a form of real-world research, they are not synonymous with it. Real-world studies broadly leverage ‘real-world data’—information collected from diverse sources outside traditional clinical trials, pertaining to patient health status and routine healthcare. Phase IV trials, while using real-world data, are a specific, regulated category of research within the broader domain of real-world evidence generation. They serve as an indispensable complement to earlier phases, ensuring a drug’s safety and efficacy are continuously assessed throughout its entire lifecycle.
The journey of drug development, as we have seen, is an extraordinary testament to human ingenuity, perseverance, and ethical commitment. From the meticulous preclinical investigations to the expansive post-market surveillance of Phase IV, each stage plays a vital role in ensuring that new medical breakthroughs are not only effective but also demonstrably safe for those who need them most. It is a path paved with immense challenges, significant investments, and rigorous scientific scrutiny, all culminating in the profound impact these innovations have on global health and patient well-being.