
Dysautonomia, a term that for many remains shrouded in mystery, represents a vast and often debilitating collection of disorders impacting the autonomic nervous system. While it affects an astonishing number of people worldwide, its effects frequently go unseen, making it one of the most common yet least understood conditions of our time. This invisibility often leads to profound frustration for those living with it, as symptoms are dismissed or misattributed, delaying diagnosis and much-needed support.
The autonomic nervous system, or ANS, functions as the silent maestro of our internal bodily processes, orchestrating essential functions we rarely consciously acknowledge. From regulating our heart rate and blood pressure to managing digestion, breathing, and even body temperature, the ANS works tirelessly behind the scenes. When this intricate system malfunctions, the impact can be widespread and profoundly disruptive, manifesting in a bewildering array of symptoms that can make daily life an immense challenge.
This article delves into the complex world of dysautonomia, shedding light on its definition, common manifestations, the significant hurdles to diagnosis, and the very real experiences of those who navigate its unpredictable landscape. Through a blend of scientific explanation and personal narratives, we aim to demystify this invisible illness and underscore the critical need for greater understanding and compassion for the millions affected.
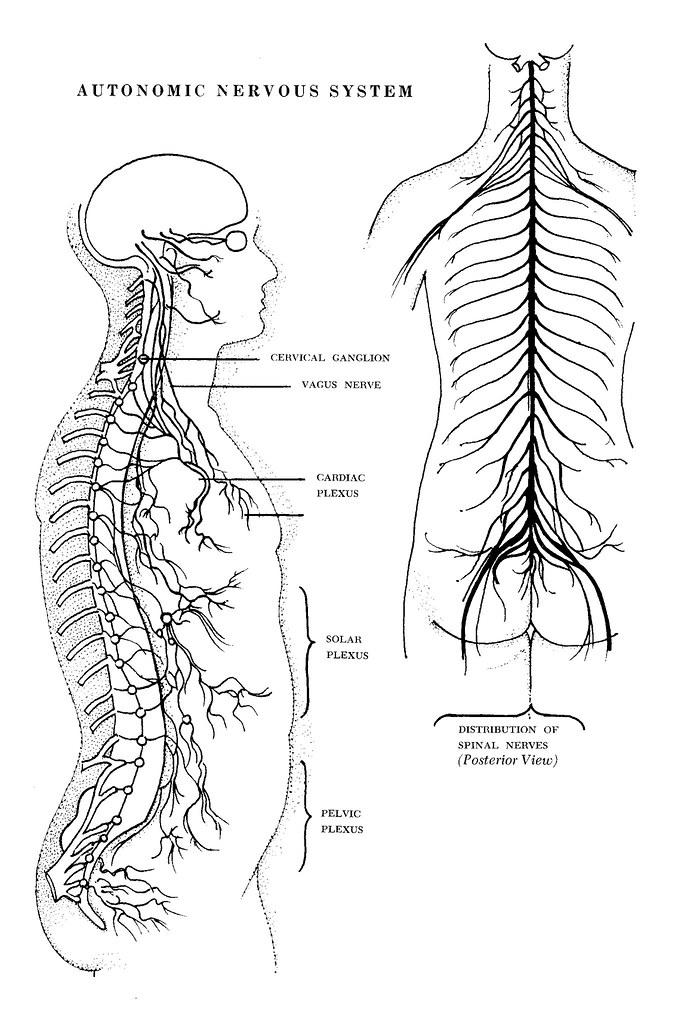
1. **Defining Dysautonomia: The Autonomic Nervous System Unveiled**: At its core, “dysautonomia” serves as a broad, encompassing term for any disorder that disrupts the normal functioning of your autonomic nervous system (ANS). This vital subdivision of our nervous system is truly “self-governing,” meaning it controls all the body system processes you never have to consciously think about. Without the ANS, fundamental life-sustaining activities like maintaining blood pressure, regulating body temperature, breathing, digestion, and even heart rate would cease to function properly.
Imagine your body as a finely tuned vehicle, constantly adjusting its speed, stopping when necessary, and accelerating smoothly. In this analogy, the sympathetic and parasympathetic nervous systems act as your body’s “gas and brake pedals,” working in harmony to ensure safe and functional operation. Dysautonomia, then, arises when these crucial “pedals” are not functioning as they should, leading to a cascade of internal havoc that can range from incredibly mild to utterly debilitating, affecting a variety of vital organs.
2. **The Myriad Manifestations: Understanding Dysautonomia’s Diverse Symptoms**: Given the sheer breadth of functions managed by the autonomic nervous system, it follows that dysautonomia can present with an extraordinarily wide and diverse range of symptoms. These manifestations are not only numerous but can also change constantly, adding another layer of complexity and confusion for both patients and healthcare providers alike. It’s this unpredictable variability that often makes the condition so challenging to identify and treat effectively.
Common symptoms associated with dysautonomia include, but are not limited to, persistent chest pain, debilitating mood swings, recurrent fainting spells, profound and unrelenting fatigue, and pervasive dizziness. One individual battling the condition described a loss of control over their entire digestive system, from mouth to “the other end,” along with uncontrollable blood pressure and “random symptoms I get which constantly change all the time.” This personal account powerfully illustrates the highly individualized and often baffling nature of the illness.
3. **An Unseen Epidemic: How Common is Dysautonomia?**: Despite its relative obscurity in public discourse, dysautonomia is far from rare. Various forms of this condition are, in fact, remarkably common, impacting a staggering number of individuals globally. More than 70 million people worldwide are estimated to have some form of dysautonomia, making it a significant, albeit largely unrecognized, public health concern.
To put its prevalence into perspective, one specific dysautonomia condition, Postural Orthostatic Tachycardia Syndrome (POTS), affects between 1 million and 3 million Americans alone. This means POTS on its own is “more common than multiple sclerosis,” a condition with far greater public recognition. Dysautonomia can be congenital, meaning present at birth, or it can develop at any point in life, with the average time of onset often falling between the ages of 50 and 60, though it can strike much earlier.

4. **The Challenging Road to Diagnosis: Why Dysautonomia Remains a Mystery to Many**: For many, the journey to a dysautonomia diagnosis is a long, arduous, and emotionally draining one, often fraught with skepticism and disbelief from the very medical professionals meant to provide care. It has been aptly called “the most common condition you’ve never heard of,” and sadly, many sufferers are initially told by doctors that their symptoms are “all in their head,” leading to immense psychological distress on top of their physical ailments. This lack of understanding creates a rough road to diagnosis, often stretching over years.
Patients frequently find themselves navigating a healthcare system where providers have limited experience with the condition, as “the condition can vary widely and take many forms.” Corey Sukalich, a 36-year-old former electrical engineer, recounted how it was “years before doctors put a name to his ‘invisible illness’,” even being told by one doctor to “try harder, basically, ‘Suck it up.’” Similarly, Stacy Campo, an avid hunter, was dismissed with “Oh it’s nothing, you’re just high-strung” when her debilitating symptoms began.
The frustrating reality for many is that “every test I have been subjected to has come back negative,” as noted by one patient, leaving them with no clear answers. Carmen Gonzales, a single mom, endured “twenty-eight times to the hospital in a two-year period” before finally receiving a diagnosis at Vanderbilt, where “doctors knew right away what it was.” Victoria Moghadammi also faced disbelieving doctors, who dismissed her severe symptoms with “It’s just anxiety, you’ll be fine,” despite her harrowing experiences of not being able to exhale and feeling her anxiety “through the roof.” This pervasive skepticism makes the diagnosis process not just challenging, but often “mortifying.”
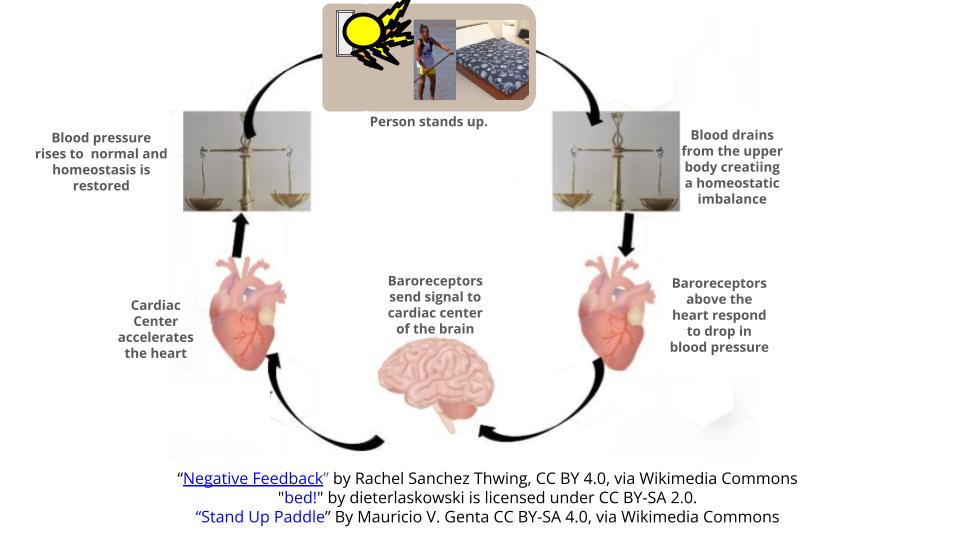
5. **POTS: A Common Form of Dysautonomia**: Among the various forms of dysautonomia, Postural Orthostatic Tachycardia Syndrome, widely known as POTS, stands out as one of the most frequently diagnosed and discussed. This specific condition is characterized by a set of symptoms that significantly impact a patient’s ability to maintain an upright posture without experiencing severe physiological distress. Understanding POTS is key to grasping how dysautonomia can profoundly disrupt daily life.
The hallmark of POTS is the dramatic change in heart rate and blood pressure upon standing. As Dr. Umesh Patel, a cardiologist, explains, “a patient’s heart races and blood pressure drops when they stand up.” This postural intolerance leads to common symptoms such as dizziness, light-headedness, and fainting spells, which can be disorienting and dangerous. Victoria Moghadammi, for instance, was diagnosed with POTS after being bedridden for three months, describing how she “couldn’t stand up without feeling like I ran a marathon.”
Beyond the core issues of heart rate and blood pressure regulation, POTS patients often experience a constellation of other symptoms including chest pain, abdominal pain, and profound fatigue. The simple act of standing up can trigger an intense internal response, as Carmen Gonzales vividly put it, “Most people jump out of airplanes to get an adrenaline rush. I just stand up.” This illustrates the extraordinary effort and physiological chaos that even routine movements can induce for those living with POTS.

6. **The Invisible Burden: Living with Dysautonomia’s Profound Fatigue**: Perhaps one of the most debilitating yet often misunderstood symptoms of dysautonomia is the overwhelming and profound fatigue it inflicts upon patients. This is not merely tiredness that a good night’s sleep can remedy; it is a deep, soul-sapping exhaustion that permeates every aspect of existence, leaving individuals drained of energy and vitality. It’s the kind of fatigue that Dr. Patel characterizes as “sucks it out of you fatigue.”
This level of exhaustion can render even the simplest daily tasks monumental challenges. Victoria Moghadammi, grappling with POTS, revealed that for three months she was “practically bedridden” and “couldn’t stand up without feeling like I ran a marathon.” Corey Sukalich’s experience echoes this, as he “was not able to be reliably on time” for work and found “daily tasks like showering were taxing,” making it impossible for him to hold a regular job.
The invisible nature of this fatigue, like many dysautonomia symptoms, makes it difficult for others to comprehend, often leading to further isolation for sufferers. Mark Martin, after a long day at his new, safer job where he works on his feet for eight to ten hours, “comes home and collapses onto the couch,” unable to contribute to household chores. This pervasive lack of energy, though unseen, undeniably exerts an enormous impact on the quality of life, underscoring the critical need for compassion and support for those living with dysautonomia.
While the previous section laid bare the intricate symptoms and challenging diagnostic journey of dysautonomia, a deeper dive reveals the complex factors contributing to its onset and the varied paths patients take toward managing this enigmatic condition. Understanding the triggers, treatment strategies, and long-term outlook is crucial for both those affected and the wider community striving for greater recognition.

7. **Understanding the Complex Origins and Triggers**: The precise causes of dysautonomia often remain elusive, yet research and patient experiences have begun to shed light on potential origins and triggers that can lead to the autonomic nervous system malfunctioning. There exists a significant “knowledge gap” in fully understanding why this delicate system breaks down, but it is clear that for many, the onset of acute symptoms can be traced to specific events or illnesses.
Patients frequently report that their symptoms began after significant health traumas. These can include viral illnesses, major surgery, or other forms of physical trauma. For instance, Victoria Moghadammi’s symptoms started after a car accident and concussion, intensifying dramatically after a dry-needling procedure. Corey Sukalich also recalls two bouts of severe food poisoning in his teens, which he believes might have served as triggers for his own condition. Dr. Robert Wilson, a neurologist, eloquently compares this to “smoke damage” after a fire, suggesting that dysautonomia can be the lasting impact on a very delicate system after a previous bodily ordeal.
Beyond singular traumatic events, doctors also suggest that stress could be a contributing factor. In some cases, particularly with Postural Orthostatic Tachycardia Syndrome (POTS), about half of patients’ diseases are believed to stem from an immune response to an infection. This complex interplay of potential triggers underscores the highly individualized nature of dysautonomia’s onset, making its origins a critical area for continued research and understanding.

8. **Navigating Treatment and Symptom Management**: Despite the complexities surrounding its origins, and the fact that there is no known cure for dysautonomia itself, the condition is indeed treatable. The focus of management centers around alleviating individual symptoms and improving a patient’s quality of life, which can vary significantly depending on the specific form of dysautonomia and the patient’s unique symptom profile.
Common strategies often involve lifestyle adjustments and supportive therapies. Doctors frequently recommend increasing fluid intake and boosting salt levels, as well as wearing compression garments that fit tightly over the body. These measures are designed to counteract issues like blood pooling in the abdomen and thighs, which can contribute to light-headedness, fainting, and low blood pressure. Beyond these general approaches, specific medications are often prescribed to target particular symptoms. Stacy Campo, for instance, found relief on a low dose of Midodrine to help regulate her heart rate and blood pressure, while Carmen Gonzales made significant progress with the FDA-approved drug Northera.
For those whose dysautonomia is secondary to another underlying illness, such as Addison’s disease or Crohn’s disease, treating that primary condition becomes critical for controlling dysautonomia symptoms. Some patients, like Victoria Moghadammi, have explored holistic approaches, including dietary changes, and have successfully learned to manage and live with POTS. While medications may not eliminate all pain or discomfort, they demonstrably help patients feel better, illustrating that even without a cure, effective symptom management can lead to significant improvements in daily function.
The journey through dysautonomia is undeniably fraught with complexity, from its varied and often elusive origins to the profound emotional and social burdens it places on individuals and their families. Yet, the resilience of those living with this condition, coupled with a growing, fervent movement for awareness, offers a beacon of hope. As understanding expands within both the medical community and the general public, the path toward better diagnosis, more effective treatment, and compassionate support becomes clearer. This ongoing dialogue is not just about illuminating an invisible illness, but about fostering a world where every patient feels seen, heard, and genuinely cared for, regardless of the outward signs of their struggle.



