
The year 2024 has been marked by a significant public health alert concerning a widespread Listeria outbreak linked to deli meats, primarily from Boar’s Head and Old Country brands. This contamination has triggered a national recall affecting millions of pounds of products distributed across numerous U.S. states and several international markets. The Centers for Disease Control and Prevention (CDC) and the U.S. Department of Agriculture’s Food Safety and Inspection Service (FSIS) have actively investigated, uncovering critical sanitation issues at manufacturing facilities.
This ongoing outbreak highlights severe concerns within the food industry, particularly regarding ready-to-eat meats sliced at deli counters. The consequences have been tragic, with dozens hospitalized and multiple fatalities reported, underscoring the serious health risks posed by Listeria monocytogenes. Vulnerable populations, including pregnant women, newborns, adults aged 65 or older, and individuals with weakened immune systems, face heightened risks.
As consumers seek clarity and assurance, this report compiles essential information regarding the outbreak’s progression, its identified causes, and the urgent measures being taken by health authorities and the implicated company. The following sections will detail key aspects of this massive recall, from the initial identification of contaminated products to the extensive list of affected items and retailers, providing a comprehensive overview of a significant food safety crisis.
1. **The Scale of the Outbreak**The 2024 Listeria outbreak is notably the largest listeriosis outbreak of its kind in the U.S. since 2011. Since the CDC’s initial report on July 19, a total of 59 people infected with the outbreak strain of Listeria have been reported from 19 states as of September 23. All 57 affected individuals have required hospitalization, indicating the illness’s severe nature.
Tragically, the outbreak has resulted in ten reported deaths across several states. These fatalities include one each in Illinois, New Jersey, Virginia, Florida, Tennessee, and New Mexico, and two each in New York and South Carolina. The CDC reported six new deaths on August 28, with an additional death in New York by September 23. These grim statistics highlight the lethal potential of Listeria monocytogenes, particularly for high-risk individuals.
Food safety lawyer Bill Marler noted that Listeria’s incubation period can exceed two months, implying that more illnesses and potentially deaths are still expected. Individuals who consumed tainted deli meat in July could develop symptoms into the fall. The CDC also stated that identifying whether a sick individual is part of an outbreak can take three to four weeks, suggesting the actual number of sick individuals is likely higher than official reports, as many mild cases may go uncounted.
Read more about: Rewind & Reflect: 14 Vintage Car Commercials That Couldn’t Air Today

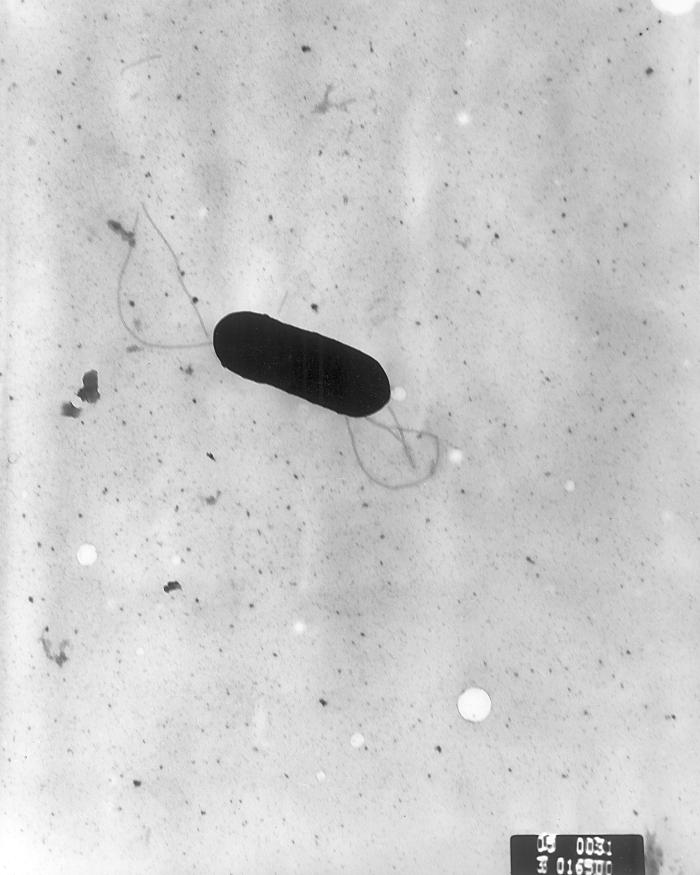
2. **Listeria: A Deadly Foodborne Threat**Listeria monocytogenes is a type of bacteria commonly found in moist environments like water and soil. A key characteristic of this bacterium is its ability to survive and even multiply under refrigeration temperatures, posing a persistent threat in food processing and storage facilities. When consumed through contaminated food, it causes listeriosis, an illness ranging from mild gastrointestinal upset to severe, life-threatening invasive disease.
While the CDC estimates approximately 1,600 Listeria infections occur annually in the United States, this relatively smaller number compared to other foodborne pathogens is misleading. Listeria infection is the third leading cause of death from foodborne illness in the U.S., responsible for about 260 fatalities each year. CDC data suggests 1,250 people are infected with Listeria annually, with 172 succumbing to the infection, underscoring its significant mortality rate.
Listeria causes severe illness when the bacteria spread beyond the gut to other body parts, termed invasive illness. Most individuals, however, recover from intestinal illness without antibiotic treatment. Deli meat is considered a high-risk food for Listeria contamination because the bacteria spreads easily on equipment and surfaces, and the product is typically consumed without further heating, which is necessary to kill Listeria. Prevention relies on proper food handling and thorough heating.

3. **Identification of the Source**The investigation into the widespread Listeria outbreak quickly focused on deli meats, specifically those sliced at deli counters, as a common exposure point. Early epidemiological data from the Centers for Disease Control and Prevention (CDC) indicated a strong link between consuming these products and illness. Of 24 individuals interviewed initially, 23 reported eating meats sliced at a deli prior to falling ill.
Further inquiries pinpointed a more specific connection: “Of the 23 people who were asked if they ate liverwurst, 13 reported deli-sliced liverwurst before getting sick, and seven reported Boar’s Head brand.” This detailed patient information provided crucial leads for investigators. The critical breakthrough in identifying the source occurred when a sample of Boar’s Head liverwurst tested positive for the outbreak strain of Listeria monocytogenes.
This contaminated sample was not a random find; Maryland health officials collected it from an unopened package of liverwurst obtained from a grocery store. Subsequent whole genome sequencing tests definitively confirmed that the Listeria strain in this liverwurst precisely matched the genetic fingerprint of the strain cultured from patients in the outbreak. This scientific validation confirmed contaminated deli meats, particularly liverwurst from a specific facility, as the likely primary source of the widespread illnesses and fatalities.
Read more about: Hyundai-Kia Crisis: Towing Hitch Fire Risk Threatens Telluride and Palisade SUVs

4. **Boar’s Head Initial Recall**Following the definitive confirmation linking its liverwurst product to the national Listeria outbreak strain, Boar’s Head Provisions Co. Inc., located in Jarratt, Virginia, initiated its first voluntary recall on July 26. This initial action targeted over 200,000 pounds of liverwurst due to potential Listeria contamination, marking the immediate corporate response to the public health threat.
The recalled product was identified as Boar’s Head Strassburger Brand Liverwurst MADE IN VIRGINIA. This specific item was sold in 3.5-pound loaves in plastic casings or in various weight packages sliced at retail delis. Consumers were advised to check for sell-by dates ranging from July 25, 2024, to August 30, 2024, on their liverwurst purchases to identify if they possessed a recalled item.
The company’s decision to enact this recall stemmed directly from learning from the U.S. Department of Agriculture (USDA) that their Strassburger Brand Liverwurst was linked to the outbreak. Boar’s Head stated on its website that “Based on this new information, we took steps to ensure we are doing everything possible to protect public health.” This initial action was a critical first step in attempting to contain the spread of the deadly bacteria.

5. **The Expanded Recall: Scope and Scale**Just five days after its initial recall, on July 30, Boar’s Head Provisions dramatically expanded its recall, adding an astounding 7 million pounds of products. This massive expansion was a broad and precautionary measure, prompted by the company’s decision to include every item produced at the same Jarratt, Virginia facility where the contaminated liverwurst originated. The expanded recall ultimately encompassed 71 products sold under both the Boar’s Head and Old Country brand names.
This recall, totaling over 7 million pounds of deli meat, was described by Boar’s Head as a necessary action because they “believed it was the right thing to do,” demonstrating their commitment to public health. The severity of the situation was further underscored by the company’s decision to immediately and voluntarily pause all ready-to-eat operations at the Jarratt facility until further notice. This move signaled a comprehensive review and rectification of their processes.
The vast array of items included in this recall primarily consisted of ready-to-eat meats and poultry products. These products were intended for slicing at retail delis, allowing for widespread distribution in grocery stores, but some pre-packaged items were also included. This wide net of recalled products reflected profound concerns about potential widespread cross-contamination within the Jarratt facility, indicating a systemic problem that necessitated drastic measures.
Read more about: Ford’s Hybrid Fire Risk: An In-Depth Consumer Report on Escape, Corsair, and Maverick Recalls

6. **Recalled Products and Identification**The comprehensive and expanded recall, implemented on July 30, encompasses a substantial list of 71 distinct products, marketed under both the prominent Boar’s Head and Old Country brands. These potentially contaminated items were produced between May 10, 2024, and July 29, 2024. Consumers are advised to check for sell-by dates ranging from July 29, 2024, to October 17, 2024. A critical identifier for consumers is the presence of “EST. 12612” or “P-12612” located inside the USDA inspection stamp on the product labels.
The list of specific recalled Boar’s Head brand meats is extensive and diverse. Examples include various hams like Virginia Ham Whole, Fiber Cappy Ham Half, Hot Butt Cappy Ham, Gourmet Pepper Ham Half, Sweet Slice Ham Whole and Half, Natural Casing Cappy Ham Half, Tavern Ham, Extra Hot Cappy Ham, and Rosemary Sundried Tomato Ham. Other recalled Boar’s Head products range from frankfurters, head cheese, and olive loaf to different varieties of bologna, salami, and sausages, including the Smoked Andouille Chicken Sausage.
In addition to Boar’s Head branded items, the recall extended to 17 kinds of Old Country brand hams. These Old Country products were primarily sold to the foodservice industry, distributed to restaurants, caterers, and cafeterias, highlighting the broad impact across various food sectors. The USDA’s Food Safety and Inspection Service (USDA FSIS) posted a full, detailed list of all 71 products, with images of their labels, to assist in accurate identification and prompt removal from sale and consumption.
Read more about: Consumer Notice: These 9 Used Bicycles Become Frame Crackers Once They Hit 10000 Kilometers

7. **Affected Retailers and Distribution**The massive recall of Boar’s Head and Old Country deli meats due to Listeria contamination has had an extraordinarily extensive reach, impacting a vast network of retailers across virtually every state in the United States and several international markets. The contaminated products were distributed nationwide, making it an urgent matter for consumers in a multitude of states to diligently check their purchases for affected items.
The sheer scale of distribution is evident from a list of stores that sold recalled Boar’s Head deli meats, published on the USDA’s Food Service and Inspection Service (USDA FSIS) website. This comprehensive document is an astounding 825 pages long, illustrating the deep penetration of these products into the U.S. food supply chain. It includes almost every state in the U.S., from Alabama to Wyoming, and extends to three U.S. territories: Puerto Rico, the Virgin Islands, and Washington, D.C.
Key states involved in the recall include Arizona, Florida, Georgia, Illinois, Indiana, Massachusetts, Maryland, Minnesota, Missouri, North Carolina, New Jersey, New Mexico, New York, Pennsylvania, South Carolina, Tennessee, Virginia, and Wisconsin. Internationally, the contaminated products were exported to the Cayman Islands, the Dominican Republic, Mexico, and Panama. Prominent retailers affected include Alberstons, Kroger, Publix, H-E-B, Target, and many others, underscoring the significant and complex challenge in removing all contaminated products from consumer hands.
Read more about: Seriously What Happened? From Classic Blends to Legal Battles: 8 Cigar Brands That Mysteriously Vanished from Local Tobacco Shops

8. **Federal Inspection Reports Reveal Unsanitary Conditions**Months prior to the catastrophic Listeria outbreak and subsequent recalls, federal inspection reports from the U.S. Department of Agriculture’s Food Safety and Inspection Service (FSIS) had documented a disturbing array of unsanitary conditions at the Boar’s Head Jarratt, Virginia plant. These reports, spanning the 12 months leading up to the voluntary shutdown, painted a grim picture of systemic failures within the facility. Food safety lawyer Bill Marler, commenting on these findings, starkly stated, “This is the worst set of inspection reports I have ever seen.”
Inspectors consistently noted concerning issues such as the presence of insects, both alive and dead, black and green mold, and mildew throughout the plant. Specific observations included a “steady line of ants” on a wall in June 2024. These findings indicated persistent sanitation challenges that posed a direct threat to food safety and the integrity of the products being manufactured.
Further reports detailed instances of “Ample amounts of blood in puddles on the floor” in the plant’s Raw Receiving cooler in February 2024, accompanied by a “rancid smell.” Such conditions point to inadequate cleaning protocols and a potential environment conducive to bacterial growth. The FSIS ultimately filed 69 reports of “noncompliances” over the past year at the Jarratt plant, reflecting a pattern of regulatory violations that preceded the widespread Listeria contamination.

9. **Calls for Congressional Investigation and Legal Challenges**The revelations of sustained unsanitary conditions have prompted strong calls for a congressional investigation into both Boar’s Head’s practices and the oversight by federal inspectors. Food safety lawyer Bill Marler, who represents families affected by the outbreak, has been a vocal proponent of such an inquiry. Marler emphasized the clear need for accountability, stating, “It’s a layup, whether you are a Republican or Democrat, to have congressional hearings on why this happened and why FSIS inspectors let this thing drag on.”
Marler did not mince words when expressing his dismay over the situation. He posed pointed questions about the plant’s operational priorities and the role of regulatory bodies. “It’s crazy. Not only was this plant better at producing listeria than it was at producing meat, but also, what were the inspectors doing?” he questioned in an interview with USA TODAY. This highlights a significant concern regarding the effectiveness of federal oversight.
Beyond calls for investigation, Boar’s Head has faced tangible legal repercussions stemming from the outbreak. The company has been confronted with multiple lawsuits filed by individuals who suffered illnesses or by the families of those who tragically died. These legal challenges seek to hold the company accountable for the devastating impact of the contaminated products.
Further adding to the pressure, Representative Rosa DeLauro characterized the situation as a “pattern of negligence.” She asserted that the company was “cutting corners to protect the company’s bottom line at the expense of consumers,” underscoring the severity of the alleged disregard for public health and safety.
Read more about: Reality TV’s Reckoning: The Legal and Financial Disasters That Threaten Dynasties

10. **Listeria Symptoms and Vulnerable Populations**Listeria infection, or listeriosis, presents a range of symptoms that can vary significantly depending on the individual infected and which part of the body is affected. The Centers for Disease Control and Prevention (CDC) distinguishes between two primary kinds of illness: invasive illness, where the bacteria spread beyond the gut, and intestinal illness, which is typically milder and confined to the gastrointestinal tract. Understanding these variations is crucial for recognizing the severity of the infection.
A Listeria infection can be particularly harmful, and even deadly, for certain high-risk populations. These vulnerable groups include pregnant women, newborns, adults aged 65 or older, and individuals with weakened immune systems. For pregnant women, Listeria can lead to severe outcomes such as pregnancy loss, premature birth, or life-threatening infections in their newborns, even if the mother experiences only mild, flu-like symptoms. Other people can contract Listeria, but they generally do not become seriously ill.
Common symptoms for non-pregnant individuals can include fever, muscle aches, and a general feeling of lethargy. More severe invasive illness may manifest with symptoms such as headache, a stiff neck, confusion, loss of balance, and even seizures. The CDC notes that symptoms can begin anywhere from the same day of consuming contaminated food to as late as 10 weeks afterward, though they often appear within two weeks. Prompt medical attention is advised if these symptoms develop after consuming potentially contaminated products.
Read more about: Unpacking Food Safety: A Comprehensive Consumer’s Guide to Preventing Illness and Protecting Your Family
11. **Diagnosis and Treatment of Listeria Infection**Accurate and timely diagnosis of Listeria infection is critical for effective management and treatment. Listeria infection is typically confirmed through laboratory testing. This involves growing Listeria bacteria from a sample of an ill person’s body fluid or tissue, such as blood or cerebrospinal fluid. This diagnostic method allows healthcare providers to definitively identify the pathogen responsible for the illness.
Once diagnosed, the course of treatment for listeriosis is tailored to the specific kind of illness experienced and its overall severity. For individuals suffering from diarrhea, a common symptom of intestinal illness, drinking plenty of fluids is a primary recommendation to prevent dehydration, which occurs when the body lacks sufficient water. Hydration is key to supporting recovery from gastrointestinal distress.
Antibiotic treatment is a crucial component for managing invasive Listeria illness, where the bacteria have spread beyond the gut to other parts of the body. In these severe cases, antibiotics are administered to combat the infection and prevent further complications. For most people with intestinal illness, however, antibiotic treatment is not necessary, as they typically recover without it. Antibiotics are reserved for those who are very ill or are at an elevated risk of becoming severely ill due to the infection.

12. **Prevention of Listeria Contamination**Preventing Listeria infection is paramount, especially for at-risk populations and those who prepare food for them. Health officials emphasize the importance of awareness regarding foods that are more likely to be contaminated with Listeria. Armed with this knowledge, individuals can make safer food choices, actively reducing their exposure to the bacteria. This proactive approach is a cornerstone of effective food safety.
For the general public, adhering to fundamental food safety guidelines is universally recommended. The “Clean, Separate, Cook, and Chill” principles, advocated by food safety authorities, serve as a comprehensive framework for preventing foodborne illnesses, including listeriosis. These guidelines promote proper hygiene, segregation of raw and cooked foods, thorough cooking to kill pathogens, and prompt refrigeration to inhibit bacterial growth. Staying informed about foodborne outbreaks and product recalls is also a critical preventative measure.
Specifically, health officials have issued targeted advice for highly vulnerable groups, including pregnant individuals, those over 65, and people with weakened immune systems, regarding deli meats. It is strongly advised that these individuals do not consume meats sliced at deli counters unless the meat is reheated to an internal temperature of 165 degrees Fahrenheit. After heating, the meat should be allowed to cool before consumption. Additionally, thorough cleaning and sanitizing of refrigerator drawers, shelves, and any surfaces that may have come into contact with potentially contaminated deli meats are essential to prevent cross-contamination.
Read more about: Unpacking Food Safety: A Comprehensive Consumer’s Guide to Preventing Illness and Protecting Your Family

13. **Boar’s Head Corporate Response and Plant Status**In response to the severe Listeria outbreak, Boar’s Head Provisions Co. Inc. took significant corporate actions, including a voluntary and widespread recall, and temporarily halted operations at its Jarratt, Virginia, facility. The company publicly acknowledged the gravity of the situation, stating, “We regret and deeply apologize for the recent Listeria monocytogenes contamination in our liverwurst product.” As a direct consequence, Boar’s Head announced its decision to permanently stop manufacturing liverwurst, which was identified as a primary source of the outbreak.
The Jarratt plant, which was at the epicenter of the contamination, was shut down in September following its suspension by U.S. Agriculture Department officials. The suspension was enacted due to the company’s “failed to maintain sanitary conditions” and the withdrawal of federal marks of inspection. The company stated its commitment to implementing “comprehensive measures… to prevent such an incident from ever happening again,” signaling an internal review and rectification of its processes and procedures.
Despite the previous shutdown and the severe findings, USDA officials announced in July that they had “thoroughly reviewed” the Jarratt plant and subsequently lifted the forced suspension. The USDA’s Food Safety and Inspection Service stated that “The facility is in full compliance of the guidelines and protocols set for the safe handling and production of food and the serious issues that led to suspension have been fully rectified.” This clearance indicates the facility is set to reopen.
In preparation for its reopening, Boar’s Head has posted job openings for two dozen positions at the Jarratt site, including a food safety quality analyst. The company also convened a panel of expert advisers last fall and hired a chief food safety officer in May, emphasizing their “unwavering commitment to food safety and quality” and efforts in developing a plan to reopen the facility “in a measured, deliberate way in the coming months.”

14. **Persistent Food Safety Concerns at Other Company Locations**Despite the significant actions taken at the Jarratt facility, recent inspections have brought to light persistent sanitation problems at other Boar’s Head plants across the country. Documents obtained by The Associated Press via a Freedom of Information Act request revealed that facilities in Forrest City, Arkansas; New Castle, Indiana; and another location in Petersburg, Virginia, were flagged for sanitation issues strikingly similar to those that precipitated the devastating Listeria outbreak.
These inspection reports, covering January through July, detailed a range of concerning findings. Inspectors documented instances of meat and fat residue on equipment, walls, and stairs, indicating insufficient cleaning. They also noted drains blocked with meat products, beaded condensation on ceilings and floors, and overflowing trash cans. Additionally, observations included staff failing to wear required protective hairnets and plastic aprons, or neglecting essential handwashing protocols, all of which are critical for preventing contamination.
Food safety advocates have expressed serious concerns over these ongoing issues. Sandra Eskin, former USDA official, stated, “If there is evidence that food safety problems are continuing, the government needs to make sure the company fixes them.” Brian Ronholm of Consumer Reports added, “You would have expected after all they went through that they would put themselves in a place where you could essentially eat deli meat off the factory floor.” These comments highlight a perceived lack of systemic improvement despite the widespread recall and public health crisis.
Barbara Kowalcyk of George Washington University pointed to a deeper issue, characterizing the findings as indicative of a “food safety culture problem” that needs to start changing at the top of the organization. She advised consumers, especially vulnerable populations, to be aware that “there are issues at this organization that still are not completely under control, apparently.” These statements collectively underscore the ongoing challenges Boar’s Head faces in fully restoring confidence in its food safety practices across all its operations.
Read more about: Understanding Water Damage: The 10 Vehicles That Survive Floods and the Ones That Fail in Light Rain, Causing Costly Electrical Gremlins
The massive Listeria recall linked to Boar’s Head and Old Country deli meats has served as a stark reminder of the critical importance of stringent food safety practices. While corporate responses, regulatory actions, and a plant reopening signal progress, the persistent reports of sanitation issues at other facilities underscore the ongoing vigilance required from both manufacturers and consumers. As the food industry continues to grapple with these challenges, informed awareness and adherence to safety guidelines remain essential for safeguarding public health against deadly foodborne pathogens like Listeria.



