The journey toward the end of life is a deeply personal and unique experience for every individual. While the exact timeline and manifestations can vary significantly depending on illness, medications, and personal circumstances, there are common signs and symptoms that often emerge as a person approaches their final days, particularly within the 24 to 48 hours before death.
Understanding these changes can be an overwhelming prospect for families and caregivers. However, being informed about what to expect can provide a measure of preparedness, allowing you to respond with wisdom, compassion, and focused comfort care. It helps to shift the focus from distress to providing the most supportive and peaceful environment possible during this sensitive time.
Healthcare professionals, especially hospice nurses with extensive experience, have identified patterns in the dying process. These observations are not meant to predict an exact moment but to offer a framework for recognizing the body’s natural progression towards its final rest. The goal is to ensure comfort, dignity, and a loving presence for the individual and their family.

1. **Decreased Communication and Activity Levels**As the body begins its final deceleration, one of the most noticeable changes is a significant reduction in a person’s level of communication and physical activity. Your loved one may start sleeping for extended periods, often becoming less responsive to their surroundings. They might resist movement of any kind, finding even small shifts in position to be an effort or a source of discomfort.
As the body begins its final deceleration, one of the most noticeable changes is a significant reduction in a person’s level of communication and physical activity. Your loved one may start sleeping for extended periods, often becoming less responsive to their surroundings. They might resist movement of any kind, finding even small shifts in position to be an effort or a source of discomfort.
This inward turning is a natural part of the dying process, often described as “detaching” from life. It’s a time when external events, conversations, and even the presence of others may become less important. While challenging for caregivers to witness, this decreased engagement doesn’t necessarily signify a lack of awareness or a rejection of your presence.
Caregivers can support their loved one by continuing to speak gently, maintaining a calm environment, and offering gentle touches. If you notice signs of discomfort with movement, such as grimacing or restlessness, it is crucial to communicate with the hospice team. They can provide guidance on safe repositioning techniques or adjust pain medication schedules to ensure comfort.
Read more about: Warren Buffett’s 14 Indispensable Financial Wisdoms for Young Actors Building Lasting Wealth

2. **Declining Appetite and Fluid Intake**
A universal sign of the body winding down is a noticeable decrease, or even a complete cessation, of interest in eating and drinking. As physical systems slow, the body no longer requires the same amount of nourishment. This is a normal and expected part of the process, not a cause for concern or a need to force food or fluids.
Beyond a lack of interest, individuals nearing the end of life may also experience difficulties with swallowing. This can lead to choking or coughing with any attempt to ingest medication, food, or fluids, posing a risk rather than providing benefit. The body’s ability to process and digest food also diminishes, making intake uncomfortable.
Providing comfort care during this phase means prioritizing oral hygiene. Keeping your loved one’s mouth and lips moist with damp sponges, often called ‘toothettes,’ and applying lip balm to prevent chapping can bring significant relief. The hospice team can also prescribe medications that can be absorbed sublingually (under the tongue), through the skin, or by injection, bypassing the need for swallowing while still providing symptom relief.
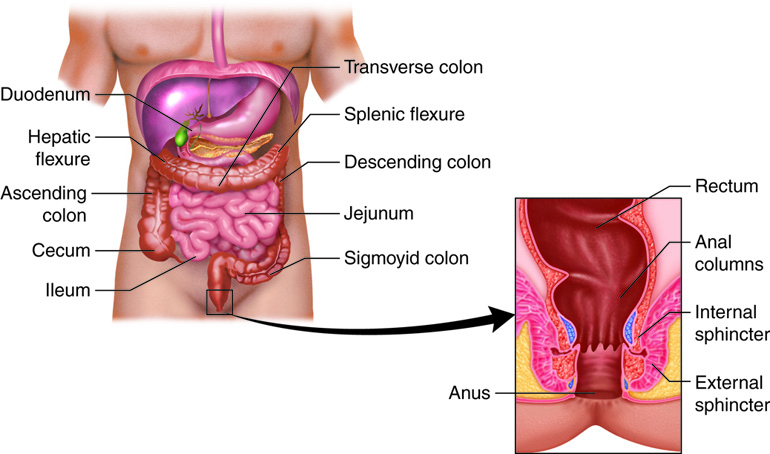
3. **Changes in Bowel and Bladder Function**
As appetite and fluid intake lessen, changes in bowel and bladder function become increasingly evident. Constipation may worsen due to reduced food intake, decreased mobility, and the effects of certain medications. Conversely, a loss of bladder control, or incontinence, may also occur as muscle tone weakens and the individual becomes less responsive to bodily cues.
Another concern can be urinary retention, where the bladder is unable to fully empty. This can lead to discomfort, restlessness, and even agitation. Caregivers should monitor for signs such as a distended or firm bladder (felt just above the pubic bone) or a lack of urination for 12 hours or more.
To maintain comfort, stool softeners or laxatives may be necessary for constipation. For bladder issues, if incontinence is causing skin irritation or if retention is suspected, a Foley catheter may be recommended by the healthcare provider. This allows for continuous urine drainage, protecting the skin, easing pressure, and reducing the need for frequent repositioning for diaper changes, which can be disruptive.
Read more about: Understanding the Journey: Common Changes Your Body Experiences When Nearing the End of Life
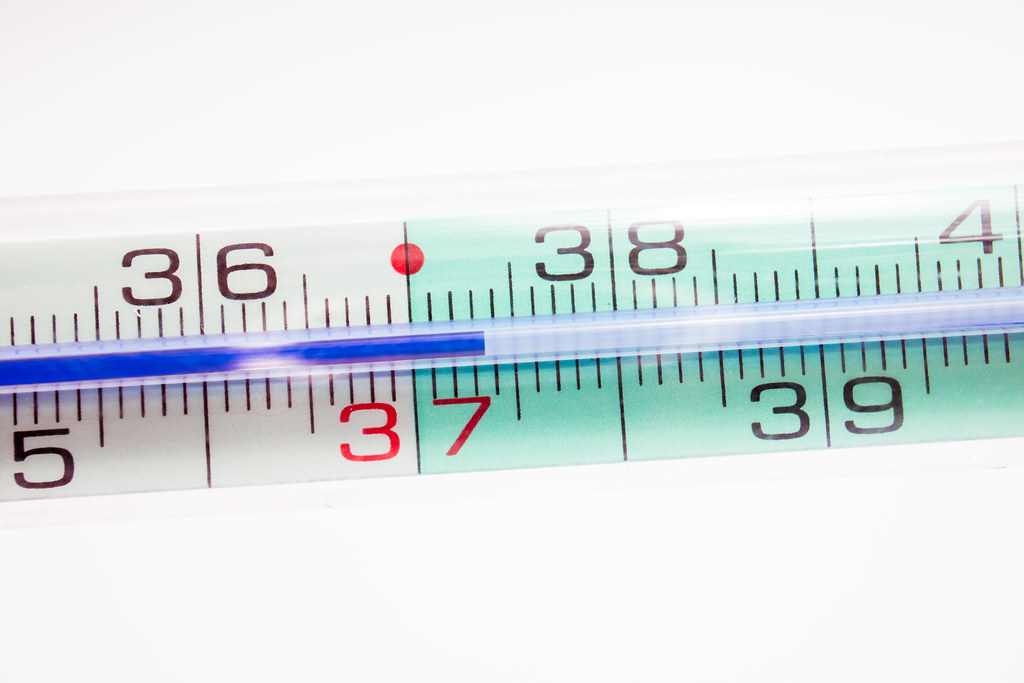
4. **Fluctuations in Body Temperature**
Changes in body temperature are common as death approaches, reflecting the body’s impaired ability to regulate its internal processes. Your loved one’s core body temperature may drop by a degree or more, causing them to feel cool. Alternatively, some individuals may develop a mild fever, with their torso and face appearing flushed and feeling warmer to the touch.
These fluctuations can occur quickly, with the person feeling hot one minute and cool the next. The extremities, particularly the knees, legs, feet, hands, and fingers, often become cool to the touch over time. This cooling is a sign of decreased circulation to the periphery of the body.
Comfort measures are key. If your loved one feels cold, a soft, warm blanket can be comforting, but avoid heating pads, as fragile skin burns easily. If they feel warm, a lukewarm washcloth placed on the forehead can provide some relief. Regularly checking their comfort level and adjusting blankets or using cool compresses can help manage these temperature swings effectively and gently.
Read more about: Decoding Your Blood Pressure Numbers: A Comprehensive Guide to Understanding and Managing Your Cardiovascular Health

5. **Irregular Vital Signs**
Near the end of life, the body’s vital signs – such as blood pressure, heart rate, and oxygen saturation – become increasingly irregular and tend to decrease. Blood pressure may drop significantly, and the pulse may become weak or thready, sometimes difficult to find. Heart rate might fluctuate, becoming either slower or irregular.
Oxygen saturation levels, which measure the amount of oxygen in the blood, will also typically decrease. While some patients with pre-existing lung conditions may tolerate lower oxygen levels for extended periods, a reading of 79% or lower is often an indicator that death may occur within the next 24 hours, though individual variations exist.
It is important for caregivers to report these changes to the hospice nurse or other healthcare providers. While taking vital signs might feel like a medical necessity, the focus at this stage is primarily on comfort. Hospice nurses often prioritize observation of comfort over precise numerical readings, but knowing the general trend of decreasing vital signs helps in understanding the progression.
Read more about: The 9 Reasons Why You Should Never Buy a Refurbished 4K Monitor (Expert Warns)
6. **Significant Skin Changes**
One of the most observable physical changes in the final hours or days of life involves the skin, particularly the development of mottling. The skin may take on a purplish, pale, gray, or blotchy appearance, especially on the knees, feet, buttocks, ears, and hands. This mottling occurs as circulation decreases and is often a strong indicator that death will occur within days or hours.
As circulation continues to diminish, the nail beds may also appear dusky. The face can become quite pale or ashen, with the area around the nose and lips becoming very pale. These changes reflect the body’s systems shutting down and are a natural part of the dying process.
Additionally, the skin, like other organs, begins to stop functioning, making it highly susceptible to breakdown. While pressure wounds can develop at any stage of a terminal illness, open wounds may appear rapidly at the end of life. Discussing care for wounds and other skin changes with the hospice team is important, with the primary goal being to ease pain with medication and maintain cleanliness, rather than aggressive, potentially painful treatments.
Navigating the final hours of a loved one’s life requires not only an understanding of the initial physical shifts but also an awareness of the intensifying symptoms that signal the body’s ultimate decline. As we move deeper into the active dying phase, several profound changes become more pronounced, impacting pain management, respiratory function, cognitive processes, and even offering moments of unexpected clarity. Being informed about these indicators empowers caregivers to provide focused, compassionate support during this most sensitive time, ensuring peace and dignity for the individual.
Read more about: Halle Berry’s Ageless Secrets: 12 Core Strategies for a Youthful Body & Unstoppable Energy

7. **Intensifying Pain**
As a person’s illness progresses towards its conclusion, pain can become more pronounced. This intensification is often due to the worsening of chronic conditions like arthritis, increased stiffness in joints, or the rapid development of pressure injuries on the skin as organ function declines. It’s important to recognize that while some individuals may verbalize their discomfort, others may be non-verbal, making it essential for caregivers to observe subtle signs.
For those who can communicate, they may directly express their pain. For non-verbal individuals, however, caregivers must be attuned to behavioral cues that signal distress. These can include agitation or restlessness, grimacing, moaning or groaning, stiffening of the body when moved, clenching fists or teeth, or even calling out. These signs serve as a crucial alert that comfort may be compromised.
When such signs are observed, the immediate step is to communicate with the hospice team. They are equipped to guide families on effective pain management strategies. Medications like Morphine or Roxanol are commonly included in a comfort kit specifically for this purpose. It is natural for families to fear that administering pain medication might make their loved one too sleepy, but healthcare professionals often encourage a shift in perspective: prioritizing comfort and peace over a distressed wakefulness is paramount in the final hours.
Read more about: America’s Grandeur and Grime: 10 Defining Epochs of Progress and 5 Persistent Shadows

8. **Profound Respiratory Changes: Slowing and Irregularity**
As the body enters the final stages of life, breathing patterns become markedly irregular, often serving as one of the cardinal signs of the actively dying state. The normal rhythm and rate of respiration may give way to periods of rapid, shallow breaths (tachypnea, over 30 breaths per minute), followed by moments where breathing slows or deepens significantly. These changes reflect the body’s systems winding down and are a natural part of the dying process.
A distinctive breathing pattern known as Cheyne-Stokes respiration frequently emerges. This involves several rapid breaths followed by a period of no breathing, or apnea, which can last from a few seconds to up to a minute. Eventually, these periods of apnea increase in length. While distressing for caregivers to witness, this specific pattern usually indicates that death is only minutes or hours away and does not typically signify pain or suffering for the individual.
Caregivers can implement several comfort measures when respiratory changes occur. Repositioning the loved one’s body, elevating the head of the bed, or using a fan nearby can sometimes ease noisy breathing or perceived discomfort. If the patient appears to be in distress, such as showing a furrowed brow, moaning, or experiencing deep, labored breathing, the hospice team should be contacted. They may recommend administering opioids like morphine, which can effectively reduce the effort of breathing and promote comfort.

9. **The Phenomenon of the Death Rattle**
The ‘death rattle’ is a recognizable sound that can occur as death approaches, typically in the final 24 hours. It is characterized by loud, gurgly breathing, often accompanied by secretions from the mouth, and results from the accumulation of respiratory secretions in the back of the throat. Because patients in a coma-like state are often unable to actively swallow, these secretions build up, causing the characteristic wheezing sound that can progress over time.
While the death rattle can be deeply unsettling and distressing for family members to hear, hospice nurses generally assure that it does not cause pain or suffering to the patient. However, there are instances where a patient may show signs of discomfort, such as trying to clear their throat, coughing, or displaying a furrowed brow. If these indications are present, it suggests the patient may indeed be bothered by the secretions.
Interventions primarily focus on comfort. Repositioning the patient, particularly elevating the head of the bed or trying a high side-lying position (sometimes referred to as the “Connecticut Drain”), can help secretions drain or settle. Medications like subcutaneous glycopyrrolate or atropine, available in the home setting, can be very effective in drying up these secretions. It’s also important to continue regular oral care, swabbing the mouth, and placing small amounts of water on the tongue for moisture.
Read more about: Hollywood’s Hidden Hazards: Unpacking the 15 Most Toxic Clauses in Multi-Picture Deals for A-List Talent
10. **Cognitive Shifts: Disengagement and Agitation**
As a person nears the end of life, significant cognitive changes are common. One profound shift is a gradual withdrawal from the external world, often described as “detaching” from life. Your loved one may become increasingly less responsive to questions, show diminished interest in favorite activities, and interact less with family members, caregivers, or friends. They may sleep for extended periods, and external events, conversations, and even your presence may become less important to them.
Another challenging but common cognitive shift is the emergence of agitation and restlessness, sometimes referred to as “terminal restlessness” or “terminal agitation.” This can manifest as unexplained periods of disquiet, constant movement in bed, attempts to get out of bed, picking at the air, or appearing confused, combative, or distressed. Delirium, which is confusion that comes and goes and gradually worsens, may also be present. These symptoms can be particularly distressing for both the patient and their family.
When agitation or restlessness appears, it is crucial to contact the hospice team immediately for guidance. They can help identify potential underlying causes, such as a full bladder (urinary retention) or wrinkled linens, and offer strategies for comfort. Medications such as Haldol or Ativan, often included in the comfort kit, are frequently used to significantly soften this process, allowing the patient to sleep and be comfortable. Throughout these shifts, caregivers should continue to speak gently and maintain a calm, peaceful environment, as hearing is often one of the last senses to lapse.

11. **Sensory Alterations and Near-Death Awareness**
Near the end of life, a dying person may experience various sensory changes that can profoundly alter their perception of the world. These alterations can include illusions, where they misinterpret real sounds or sights (e.g., the wind blowing sounds like someone crying, a lamp appears to be a person). Hallucinations are also common, where individuals report hearing, seeing, or feeling things that others cannot perceive. In some cases, delusions may occur, causing fear of harm or beliefs in impossible abilities.
A particularly unique phenomenon is “near-death awareness.” During this time, your loved one may speak about their impending death, sometimes calmly stating they will die soon. They might also express seeing or talking with God, other religious figures, or beloved family members and friends who have already passed away. These conversations can sometimes involve preparing for a “trip,” such as packing a suitcase or getting on a plane, symbolizing their transition.
It is important for caregivers to understand that these sensory changes are a normal part of the dying process and can fluctuate throughout the day, often becoming more pronounced at night. The comfort a dying person may derive from the thought of reuniting with deceased loved ones can be immense. If these sensory changes appear to cause distress, rather than comfort, the hospice team can recommend specific medications to help ease these symptoms, ensuring the patient’s final experiences are as peaceful as possible.
Read more about: Understanding the Journey: Common Changes Your Body Experiences When Nearing the End of Life

12. **The “Death Rally” and Unresponsiveness**
In the unpredictable journey toward death, some individuals may experience a phenomenon known as a “death rally.” This is a temporary, often unexpected, surge of energy that can occur in the last few days, or even up to 24 hours, before death. During this rally, a person who has been bedbound and unresponsive might suddenly display amazing mental clarity, become more communicative, and even show renewed interest in their surroundings. While not extensively researched, case studies have noted this remarkable lucidity even in patients with severe cognitive impairments.
This sudden burst of vitality can be emotionally challenging for family members, often giving them false hope that their loved one is recovering. It is crucial to understand that a death rally is typically a temporary state; most individuals will pass away within a few days or even on the same day after experiencing such a rally. It is a poignant, albeit brief, return of a person’s spirit before the final decline.
Following, or sometimes preceding, a death rally, many people will enter a state of complete unresponsiveness. This is a deeply unconscious or coma-like state where the individual cannot be roused, will not open their eyes, and is unable to communicate or respond to touch. Even in this state, it is widely believed that hearing is one of the last senses to diminish. Therefore, caregivers are encouraged to continue speaking gently, maintaining a loving presence, and tending to their loved one’s needs, as they may still be able to hear and potentially feel pain or distress.
As death becomes imminent—sometimes within minutes—the body’s final efforts are observable through distinct respiratory patterns. Breathing may become very shallow, with only the lower part of the jaw moving (mandibular breathing), or it may be characterized by significant pauses between breaths, known as apnea. The patient might appear to be opening and closing their mouth without actually breathing, or exhibit a gasping quality, called agonal breathing. Another pattern is “fish-out-of-water breathing,” where the lips puff out with barely a breath. These visual signs, while difficult to witness, are simply how the body completes its final journey.
Understanding these profound changes offers not an exact prediction, but a framework of preparedness. It allows families and caregivers to approach these final moments with wisdom, compassion, and unwavering love. Your presence, your gentle words, and your commitment to comfort are perhaps the most profound gifts you can offer, ensuring a peaceful and dignified departure for your loved one, even in the midst of the body’s final, transformative shifts.