
Blood clots are a very real risk that can change your life in a moment. While often associated with serious medical emergencies, the signs can sometimes be subtle or easy to dismiss, especially in active individuals or those who feel otherwise healthy. However, medical experts emphasize the critical importance of recognizing the potential indicators and understanding who might be at higher risk.
Recent high-profile cases, from a young boy’s life-threatening stroke to NBA superstars sidelined by deep vein thrombosis and a celebrity’s scare during pregnancy, have brought increased attention to the potential dangers of blood clots. These stories highlight that blood clots can affect individuals across different ages, activity levels, and life stages.
To help empower you with knowledge and encourage prompt medical attention when needed, we’ve compiled essential information from medical professionals and patient experiences shared in recent reports. Understanding the basics of blood clots, where they typically form, what symptoms to look for, and what factors increase your risk is the first step in protecting your health. Let’s explore what experts say about these potentially life-altering events.

1. **What is a Blood Clot?**
A blood clot, in simple terms, is a clump of blood that has changed from a liquid state to a gel-like or semi-solid state. While clotting is a normal process that helps stop bleeding after an injury, clots can sometimes form abnormally inside blood vessels, blocking blood flow. These internal clots are what medical professionals are concerned about.
The context provided mentions several specific types of blood clots. Deep vein thrombosis (DVT) is the most common, typically occurring in the veins of the arms or legs. Cerebral venous thrombosis (CVT) is a rare type affecting the brain, as seen in young Preston Patton. Pulmonary embolism (PE) is a dangerous condition resulting from a blood clot traveling to the lungs, often originating from a leg DVT.
Understanding these terms helps clarify the different ways blood clots can manifest and the potential severity of each. DVT is frequently discussed because it is common, but its primary danger lies in its potential to lead to PE. CVT, though rare, is a serious form affecting the brain with significant neurological consequences.

2. **Common Places Where Blood Clots Form**
Blood clots aren’t confined to just one area of the body; they can develop in various locations within the circulatory system. According to Dr. Edward Morrison, a vascular surgeon, blood clots can form in the arms or legs, as well as the heart, brain, lungs, and other organs or arteries. This widespread potential means symptoms can vary widely depending on where the clot is located.
The location of the clot significantly impacts the symptoms experienced and the potential risks involved. A clot in the legs might cause localized pain and swelling, while one in the lungs can lead to severe breathing difficulty. A clot in the brain, like Preston Patton’s CVT, can cause paralysis and vision loss.
Knowing the different places where clots can form underscores why a diverse range of symptoms can signal a potential problem. It also highlights why medical evaluation is crucial, as the same underlying issue – a blood clot – can present very differently depending on which vessel it obstructs.

3. **Crucial Symptoms You Should Never Ignore**
Recognizing the signs of a blood clot early is paramount because it allows for quicker intervention and reduces the risk of serious complications. Experts emphasize that while symptoms can sometimes be subtle, certain indicators should prompt immediate medical attention. These symptoms can include intense pain, swelling, and discoloration of the affected area, especially in the arms or legs where DVTs are common.
Beyond localized signs, clots can also affect the lungs or brain, leading to more systemic symptoms. These include shortness of breath, chest pain (particularly with activity), or a rapid heartbeat, which might indicate a pulmonary embolism. In cases of a brain clot, symptoms can be dramatic, such as limpness, complete paralysis on one side of the body, or loss of vision and eye movement, as described in Preston Patton’s case.
Dr. Cheng-Han Chen notes that these symptoms, like soreness, swelling, and heaviness, can sometimes be hard to recognize, especially for professional athletes who experience typical wear and tear. Gal Gadot initially experienced major headaches for three weeks that doctors attributed to migraines or hormones during pregnancy before a scan revealed brain clots. This reinforces the advice to “advocate for your health” and listen to your body, getting checked if anything feels persistently wrong, even if initially dismissed.
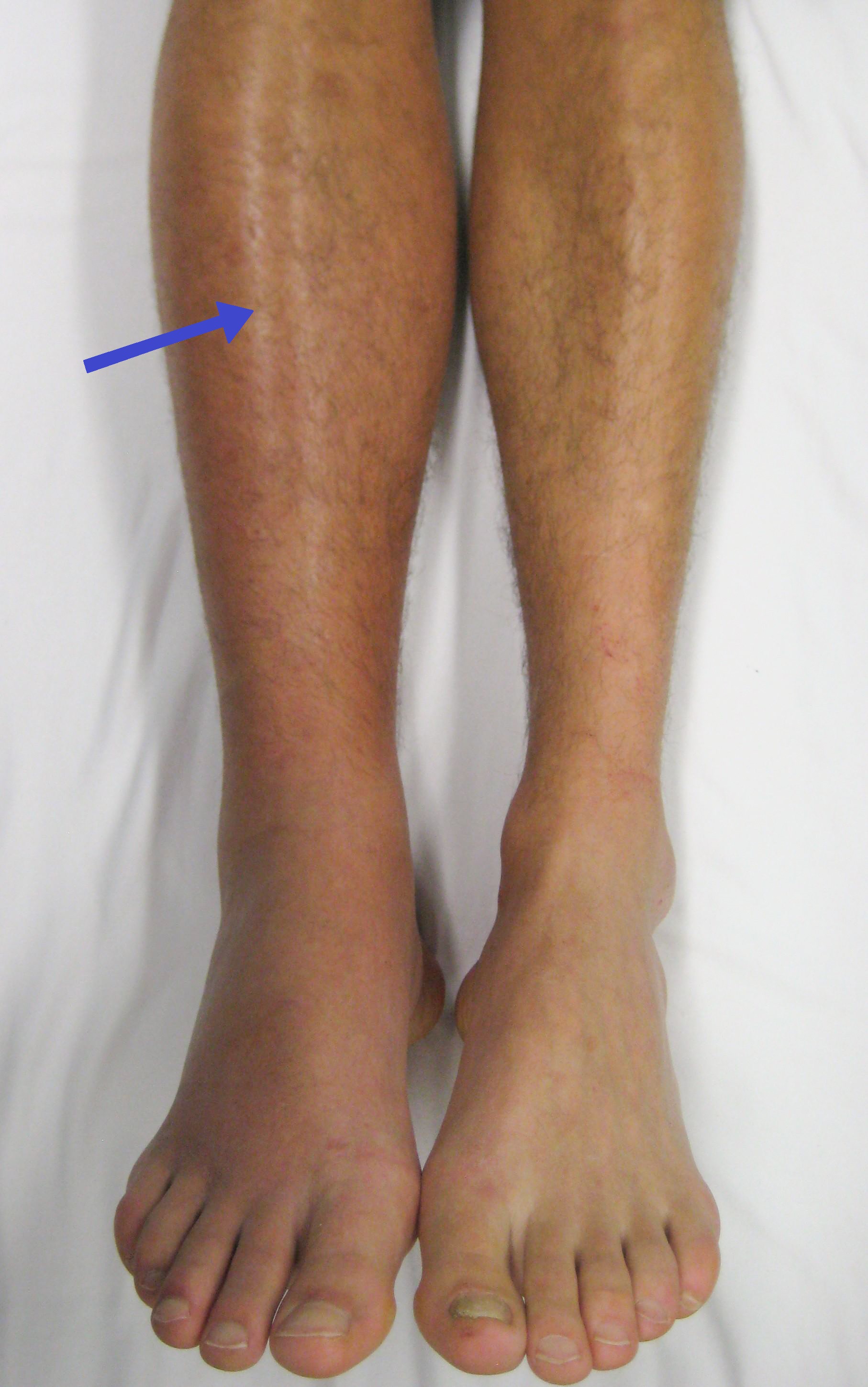
4. **Why Deep Vein Thrombosis (DVT) in Legs is Urgent**
While DVTs can occur in the arms or legs, those forming in the legs are particularly concerning due to a specific, life-threatening risk: pulmonary embolism (PE). A PE occurs when a blood clot, often originating from a deep vein in the leg, becomes dislodged and travels up to the lungs, blocking an artery there. This blockage can severely impair breathing and oxygenation, making it a medical emergency.
Dr. Vinay Badhwar, professor and chairman of the Department of Cardiovascular Thoracic Surgery, explains that lower extremity DVTs have a “predilection to migrate to the heart,” which then pumps the clot into the lungs. The earlier a DVT is caught, the lower the risk of this dangerous migration occurring and causing a PE. Dr. Cummings also highlights that clots getting larger and traveling to the lungs are a major worry, as this is what causes a majority of the fatalities associated with blood clots.
Rick Campbell’s experience after hip surgery serves as a stark reminder of this danger. He developed excruciating pain in his leg that moved up towards his groin. When he was eventually checked, doctors discovered he had suffered a pulmonary embolism. Dr. Morrison stated, “It didn’t take more than a glance for me to realize he was in trouble,” and that getting the clot out was life-threatening, reinforcing the urgency of addressing leg DVTs.

5. **Groups at Higher Risk for Blood Clots**
Certain individuals are inherently at a higher risk of developing blood clots due to various factors, ranging from medical conditions and procedures to lifestyle choices and demographics. Dr. Edward Morrison identifies several groups with increased susceptibility, including those pre- or post-surgery, older adults, individuals who smoke or are obese, postpartum mothers, and those who are immobile or on bed rest. Immobile patients face reduced blood flow, increasing clotting potential.
Statistical data also points to demographic disparities in blood clot risk. According to Erin Vandyke, Vice President of the National Blood Clot Alliance, clots impact African Americans more than Caucasians by 60%. Furthermore, with age, men become more susceptible to developing blood clots. These factors suggest that a combination of physiological, environmental, and potentially genetic elements can contribute to one’s overall risk profile.
Understanding these high-risk groups is crucial for both individuals and healthcare providers. Patients within these categories should be particularly vigilant about potential symptoms and discuss preventative measures with their doctors. Increased awareness within these populations can lead to earlier detection and better outcomes, potentially saving lives by addressing clots before they become life-threatening pulmonary embolisms or strokes.

6. **How Lifestyle and Activities Increase Risk**
Beyond inherent medical conditions, several lifestyle factors and common activities can contribute to an increased risk of blood clot formation. Prolonged periods of inactivity significantly raise the risk because blood flow slows down when you’re not moving, making it easier for clots to form. This is why frequent plane travel is cited as a risk factor, as passengers often sit for extended periods.
Other general risk factors highlighted include smoking and obesity, which negatively impact cardiovascular health and blood circulation. Dehydration can also accelerate the risk by making the blood thicker and more prone to clotting. Being immobile or on bed rest for medical reasons also falls into this category of reduced activity leading to increased risk.
Even seemingly minor choices or unavoidable situations can contribute to the overall risk picture. While professional athletes might experience this through travel or dehydration, anyone can be affected by prolonged sitting during long commutes, office work, or recovery from illness or surgery. Being mindful of these everyday factors and taking steps to mitigate them, like staying hydrated and moving periodically, can play a role in prevention.
7. **Repetitive Motion and Athlete-Specific Risks**
Professional athletes, despite their high level of fitness, face unique risk factors for blood clots, often related to the intense demands placed on their bodies. Repeated use of non-steroidal anti-inflammatory drug (NSAID) medications like Advil, commonly used for pain management in sports, has been suggested to increase the risk of DVT. This is notable given the trend away from opioids towards NSAIDs in sports medicine.
Furthermore, trauma to the extremities from repetitive motions and jumping, inherent in sports like basketball, can accelerate the risk. Dr. Christopher Yi, a vascular surgeon, notes that overuse of the arm and shoulder from repetitive arm movements, such as jump shots or even golf swings (as seen with Nelly Korda), can cause veins in the thoracic outlet to compress. This compression, part of a condition known as thoracic outlet syndrome (TOS), slows blood flow and increases the likelihood of clotting.
The cases of NBA players like Victor Wembanyama (shoulder DVT linked to Paget–Schroetter disease, a type of TOS) and Damian Lillard (calf DVT) underscore how the physical nature of their profession contributes to risk. While not genetic or familial in these specific overuse cases, the repeated stress and potential micro-trauma from athletic activity can create an environment where clots are more likely to form in specific anatomical locations subject to compression or stress.
As we’ve seen, blood clots are complex and can arise from a variety of factors, sometimes in unexpected ways. Understanding the specific causes, how doctors identify these hidden dangers, and the various ways they can be treated is just as crucial as recognizing the initial warning signs. Let’s continue our exploration into what experts and real-life experiences teach us about navigating this serious health issue.
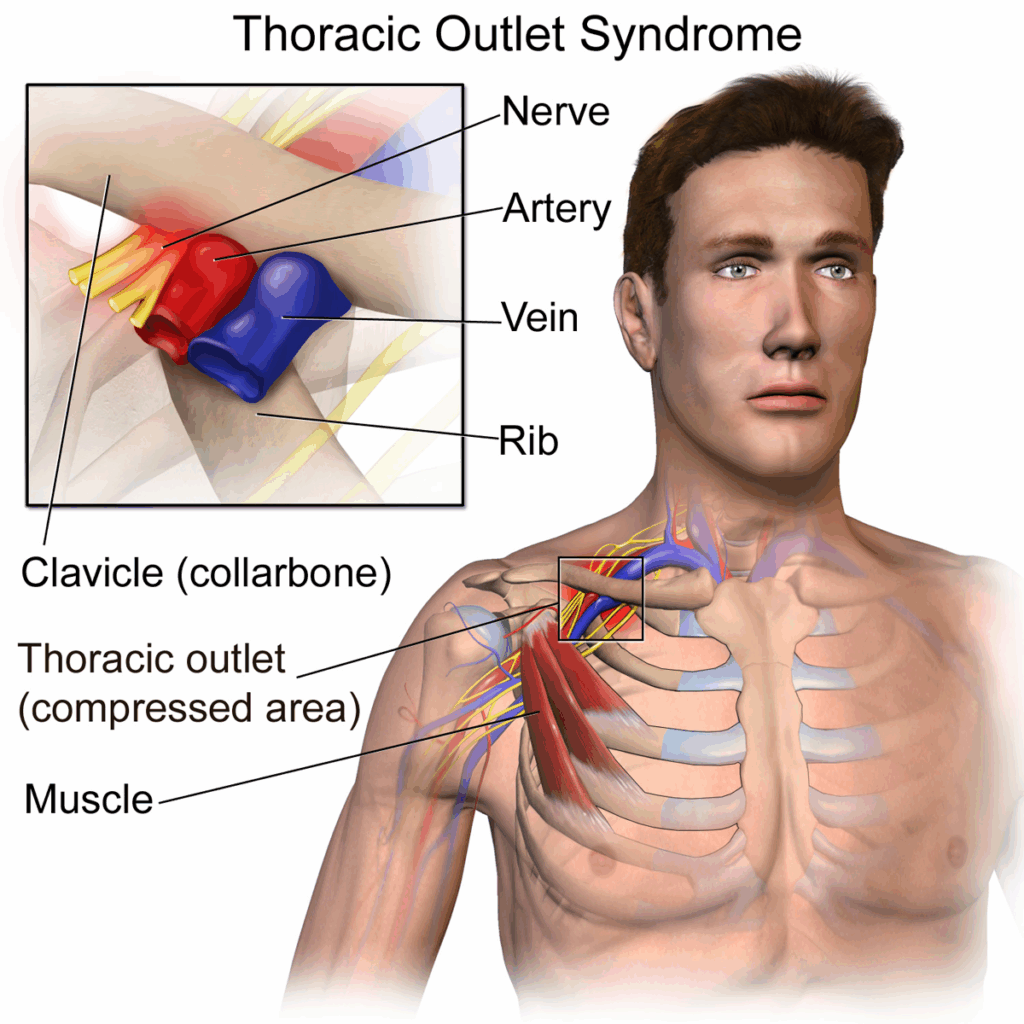
8. **Delving Deeper into Thoracic Outlet Syndrome (TOS) as a Cause**
While we touched on it briefly, Thoracic Outlet Syndrome, or TOS, warrants closer examination as a specific cause of blood clots, particularly in athletes. This condition relates to the compression of nerves, arteries, or veins in the thoracic outlet, which is the space located between the collarbone (clavicle) and the first rib. This area is also surrounded by muscles like the scalenes and is near one of the pectoral muscles.
Dr. Christopher Yi, a vascular surgeon, explains that overuse of the arm and shoulder from repetitive arm movements can cause the veins in this confined space to compress. Think about activities like jump shots in basketball, golf swings, or other actions requiring repeated overhead or strenuous arm use. This compression slows down the normal flow of blood through the vein, significantly increasing the risk of blood clotting in that specific location, often leading to upper extremity DVT.
Cases like NBA player Victor Wembanyama, diagnosed with a shoulder DVT linked to Paget–Schroetter disease (a type of TOS), and golfer Nelly Korda, highlight how this anatomical compression from athletic activity can create a predisposition for clots in the arm or shoulder. It’s not necessarily genetic or familial in these overuse cases but rather a direct result of the physical demands placed on the body, leading to a mechanically induced clotting risk in that specific anatomical region.
9. **Identifying the Hidden Danger: How Doctors Diagnose Blood Clots**
Pinpointing a blood clot isn’t always straightforward, especially when symptoms are vague or overlap with other common issues like muscle soreness or headaches. Medical professionals employ various diagnostic methods to confirm the presence of a clot and determine its location and severity. Rick Campbell’s experience highlights the process; after noticing excruciating pain and movement limitations, he was referred to the emergency room where tests were run, leading to his diagnosis of a pulmonary embolism.
In cases of suspected brain clots, like Preston Patton’s and Gal Gadot’s, brain scans, such as an MRI, are crucial diagnostic tools. These scans provide detailed images that can reveal blockages in blood vessels. Gal Gadot shared that despite suffering major headaches for three weeks and seeing multiple doctors who initially thought it was a migraine or hormone-related issue during pregnancy, an MRI finally revealed the terrifying truth of her three brain clots.
For Deep Vein Thrombosis (DVT), particularly in the limbs, imaging techniques like ultrasound are commonly used to visualize blood flow and detect clots within the veins. Dr. Cheng-Han Chen noted that part of the follow-up process after blood thinners might involve ultrasounds and other imaging to check for further clotting once a patient is off medication. The ability of medical staff to recognize potential signs and order appropriate testing is paramount, as highlighted by Dr. Edward Morrison’s immediate recognition of Rick Campbell’s life-threatening situation just from a glance and understanding his symptoms.

10. **The Primary Defense: Understanding Blood Thinners**
One of the most common and crucial treatment approaches for blood clots, particularly DVT, involves the use of blood thinners. These medications are a group of anticoagulant drugs that don’t technically “thin” the blood but rather make it more difficult for the blood to clot. Their primary function is to stop the existing clot from growing larger and to prevent new clots from forming, allowing the body’s natural processes to potentially dissolve the clot over time.
For a leg DVT, like the one Damian Lillard experienced, patients typically begin a blood thinner regimen as soon as possible. This is a standard initial step in treatment. While effective at mitigating the risk of the clot traveling or growing, being on blood thinners comes with a significant caveat, especially for athletes: it makes the body more prone to excessive bleeding.
This increased bleeding risk is why professional athletes cannot typically play their sport while on blood thinners. Any contact, falls, or even minor injuries could lead to dangerous internal or external bleeding. As Dr. Chen explained regarding Lillard’s situation, the goal is to stay on blood thinners until the clot resolves, but the recovery timeline for this process is highly unpredictable, potentially taking anywhere from three months to a year depending on the individual and the clot.

11. **Targeted Intervention: Mechanical Thrombectomy**
Beyond medication, interventional procedures are often employed, especially for larger or more dangerous clots. Mechanical Thrombectomy is a prominent example. Dr. Trevor Cummings described this procedure as a way to mechanically remove the clot from the blood vessel. It involves advancing a catheter up into the clot itself.
Once the catheter reaches the clot, medical professionals can use mechanical suction to pull the clot out. Additionally, metal coils can be advanced to further clean out the blood vessel, ensuring the blockage is removed. This procedure is described as most common for higher-risk patients dealing with conditions like Pulmonary Embolism (PE) and Deep Vein Thrombosis (DVT), offering a more immediate way to restore blood flow.
Preston Patton’s case of cerebral venous thrombosis (CVT) in his brain illustrates the critical nature of this procedure. Dr. Sourabh Lahoti performed a thrombectomy to remove the clot blocking blood flow to the right side of Preston’s brain. Despite the clot having traveled to a smaller, riskier vessel, the decision was made to proceed to prevent potentially lifelong paralysis or death. The “complete reversal” of Preston’s symptoms soon after the clot was removed demonstrates the life-saving potential of this intervention, which doctors noted was not available as a common option in the past, often leaving patients with permanent disability.

12. **Additional Treatment Avenues: Lytics, Surgery, and Support**
The spectrum of blood clot treatment includes other options beyond standard blood thinners and mechanical thrombectomy, tailored to the specific situation and severity. For some patients, Lytic Therapy may be appropriate. Dr. Cummings explained that this involves giving medications specifically designed to break up the clot, rather than just preventing it from growing or new ones from forming.
In severe, life-threatening cases, more invasive interventions might be necessary. Dr. Cummings mentioned the possibility of an open Embolectomy, which involves open heart surgery to remove a clot, particularly relevant if a large clot has impacted the heart or lungs severely. Another advanced technique is the use of ECMO (Extracorporeal Membrane Oxygenation), a mechanical device that takes over the function of oxygenating the blood, used to support patients whose lungs are compromised by a large pulmonary embolism.
Ferris State professor Sandy Alspach’s experience underscores that sometimes surgery is a necessary step. After two blood clot scares, including shortness of breath that hindered her ability to walk across campus, surgery was deemed essential. Just two weeks after her procedure, she reported being able to walk the distances needed without shortness of breath, highlighting how these various treatments, whether medical or surgical, aim to restore function and alleviate life-threatening symptoms.

13. **Location Matters: How Treatment Varies by Where the Clot Is**
A critical aspect of blood clot treatment is recognizing that the approach often differs significantly based on where the clot is located. As Dr. Christopher Yi explained, treatment strategies for lower-extremity DVT (in the legs) can be quite different from those for upper-extremity DVT (in the arms), particularly when linked to structural issues like TOS.
For DVT in the legs, like Damian Lillard’s calf clot, the standard consensus treatment typically starts with a blood thinner regimen. These are generally managed with medication, and monitoring is done as the body works to dissolve the clot. Dr. Yi noted that lower-body DVTs appear to be more random and are usually not caused by the kind of anatomical compression from bone seen in some upper-body cases, making blood thinners the primary approach.
Conversely, for arm DVT, especially if linked to Thoracic Outlet Syndrome as seen in Victor Wembanyama or previously with Brandon Ingram, there are often surgical options to address the underlying cause of compression. Ingram underwent surgery where part of his first rib was removed to relieve pressure on the vein. This surgical decompression is combined with blood thinners to dissolve the existing clot, followed by physical therapy. Dr. Yi emphasized that addressing the compression source is key in these cases to prevent recurrence, a step often not necessary for lower-extremity clots.

14. **The Road Ahead: Recovery and the Risk of Recurrence**
Recovering from a blood clot is often a process with an unpredictable timeline, and importantly, having experienced one clot increases the risk of developing another in the future. As Dr. Chen put it, “Once someone has one, then you are a little more worried that it’s going to happen again, because something in their body is prone to cause that blood clot.” This means that patients, and athletes, must be continually checked for future instances.
The duration of recovery varies greatly. For individuals on blood thinners, the time it takes for the clot to dissolve can range from a few months to a year, as Dr. Chen noted. For those undergoing surgery to address an underlying cause like TOS and remove a rib, combined with physical therapy, the full process to return to competitive form can take up to a year, according to Dr. Yi, though usually results in a full recovery in terms of function.
The long-term impact also depends on the severity and location of the clot. A Pulmonary Embolism (PE), especially a severe one originating from a leg DVT, can leave lasting effects on leg swelling and lung function. In such cases, patients may need to be on long-term blood thinners, and as tragically seen with Chris Bosh, a recurrence can unfortunately lead to retirement from high-impact activities. However, increased awareness among athletes, trainers, and the public is a silver lining, leading to earlier diagnosis and potentially better outcomes by catching clots before they cause severe complications or permanent damage.
Understanding blood clots, from recognizing subtle signs to knowing the complex diagnostic and treatment pathways, empowers us to take proactive steps for our health and advocate for appropriate care. While scary, stories of recovery like Preston Patton’s, Rick Campbell’s, and Sandy Alspach’s offer hope and underscore the critical importance of listening to our bodies and seeking medical help when something feels persistently wrong. Stay informed, stay vigilant, and prioritize your health, because knowing the signs and risks can truly be life-altering.



