
The hush of night often ushers in profound peace, a much-needed respite from the day’s demands. For many, the dream of a peaceful transition involves simply drifting off to sleep and never waking up, a seemingly serene end to life’s journey. Yet, beneath this comforting facade lies a complex interplay of physiological processes, where slumber can become an unexpected portal between worlds. This delicate balance, where vital systems momentarily falter, is a topic shrouded in both fascination and unsettling questions about our final moments.
The concept of dying in one’s sleep, though often romanticized, is far from a simple, uniform event. It compels us to confront the intricate dance between our waking consciousness and the profound physiological shifts that occur as we surrender to the night. While popular belief often paints a picture of a universally painless passing, the scientific reality is far more nuanced, revealing a spectrum of causes and mechanisms. Understanding these underlying factors is key to demystifying this enigmatic phenomenon and appreciating the delicate machinery of the human body, even in its most vulnerable state.
Our exploration will journey into the depths of sleep, examining the critical organs and systems that, when compromised, can lead to these nocturnal fatalities. From the rhythmic pump of the heart to the complex electrical symphony of the brain and the delicate balance of our metabolic functions, we will uncover specific medical conditions that increase susceptibility. While the overall risk remains relatively low for most, a deeper understanding can illuminate the importance of vigilance over our health, ensuring our nights remain a sanctuary of rest rather than a moment of unforeseen peril.
1. **Sudden Cardiac Arrest (SCA)**: Sudden cardiac arrest, often referred to as SCA, stands as the most frequent and abrupt cause of unexpected death during sleep. This catastrophic event occurs when the heart’s electrical system malfunctions, causing it to suddenly stop beating effectively. When the heart ceases its vital pumping action, blood flow to the brain and other essential organs is immediately cut off. This leads to rapid loss of consciousness and, without immediate intervention, death in a matter of minutes, a stark reminder of the heart’s tireless yet vulnerable role.
According to Sumeet Chugh, medical director of Cedars-Sinai’s Heart Rhythm Center, SCA is responsible for a staggering 90 percent of sudden and unexpected deaths during sleep, also known as nocturnal death. Individuals with underlying heart conditions, such as coronary artery disease, an enlarged heart, or pre-existing irregular heartbeats like ventricular fibrillation, are at a significantly heightened risk. The quietude of sleep often masks subtle warning signs, making these nocturnal events particularly insidious.
What makes SCA during sleep uniquely perilous is the reduced capacity to respond to distress signals. Cardiologist Jack Flyer notes, “If I’m standing up and I have a 10-second pause in my heart rate, I’m going to fall down and pass out and make a big thud and someone is going to hear it.” However, when a person is deeply asleep, they simply cannot respond to their own symptoms. This leaves them vulnerable to a sudden cessation of vital functions without outward indication of trouble, underscoring the critical need for managing pre-existing heart conditions.
2. **Arrhythmias and Undiagnosed Heart Conditions**: Beyond the dramatic immediacy of sudden cardiac arrest, the insidious nature of abnormal heart rhythms, or arrhythmias, constitutes a prevalent cause of unexpected death. These electrical disturbances cause the heart to beat too fast, too slow, or irregularly, disrupting its ability to pump blood efficiently. Among the deadliest are ventricular fibrillation, where the heart’s lower chambers quiver instead of pumping, and ventricular tachycardia, characterized by an abnormally fast heart rate.
In many tragic instances, individuals who succumb to a fatal arrhythmia during sleep may have harbored an undiagnosed heart condition, unknowingly increasing their susceptibility. These latent issues, such as structural abnormalities or genetic predispositions, can remain asymptomatic until a critical event occurs. The American Academy of Pediatrics highlights a concerning trend: sudden cardiac death, whether during sleep or waking hours, is a leading cause of death among young athletes, often due to such previously undetected conditions. This underscores the importance of thorough medical evaluations, even in seemingly healthy individuals.
The quiet periods of sleep can sometimes exacerbate these underlying vulnerabilities. Subtle shifts in heart rate, blood pressure, and oxygen levels naturally occur during different sleep stages. In a vulnerable heart, these can trigger an arrhythmia that becomes deadly. Without the body’s usual waking defenses or the awareness to seek help, these irregular rhythms can escalate into full cardiac arrest. This highlights why understanding family history and seeking regular preventative care are crucial steps in mitigating these silent, nocturnal risks.

3. **Heart Attack**: While closely related to sudden cardiac arrest, a heart attack, or myocardial infarction, presents a distinct mechanism through which death can occur during sleep. A heart attack happens when the heart muscle does not receive adequate oxygen, typically due to a blockage in a coronary artery. This oxygen deprivation causes parts of the heart muscle to become damaged or die, severely impairing the heart’s ability to pump blood and oxygen to the rest of the body.
The critical difference lies in the initial event: a heart attack is primarily a circulation problem to the heart muscle itself, whereas cardiac arrest is an electrical problem. However, a severe heart attack can certainly lead to cardiac arrest if the damaged heart muscle can no longer maintain a regular rhythm or pump adequately. The challenge during sleep is that classic warning signs, such as severe chest pain or shortness of breath, may not be recognized or may not even be present in their typical intensity.
This silent progression means that a person experiencing a heart attack during sleep may not awaken or seek help, allowing damage to the heart muscle to become extensive and irreversible. The body’s inability to respond to these critical internal signals, as Dr. Flyer points out, renders the individual helpless. This scenario underscores why managing risk factors like high blood pressure, high cholesterol, and coronary artery disease through lifestyle and medical intervention is paramount, not only to prevent heart attacks but also to reduce their fatal impact during vulnerable sleep hours.

4. **Stroke**: A stroke, a grave medical emergency that interferes with the oxygen supply to the brain, also poses a significant risk for nocturnal fatalities. This life-threatening event can be caused by two primary mechanisms: either a blood clot obstructing blood flow to a part of the brain (ischemic stroke) or a ruptured blood vessel causing bleeding within the brain (hemorrhagic stroke). Without a steady supply of oxygen, brain cells rapidly begin to die, leading to impaired function in the body parts controlled by the affected regions.
Remarkably, approximately 25 percent of all strokes occur during sleep, making it a critical consideration in cases of sudden nocturnal death. The danger here is that, unlike during waking hours when symptoms like sudden difficulty speaking or weakness might prompt immediate medical attention, a stroke occurring during sleep can go entirely unnoticed. This delay in recognition and treatment is incredibly perilous, as prompt medical intervention is crucial for minimizing brain damage and improving outcomes.
Conditions such as a brain aneurysm, a weakened, bulging blood vessel that can burst, or a massive stroken, can directly cause death during sleep by overwhelming the brain’s vital functions. Furthermore, underlying health issues like high blood pressure and obstructive sleep apnea can significantly heighten the risk of experiencing a stroke at night. The link between sleep apnea and stroke is well-documented, as intermittent oxygen deprivation can strain the cardiovascular system and make blood clots more likely, creating a deadly synergy under the cloak of night.
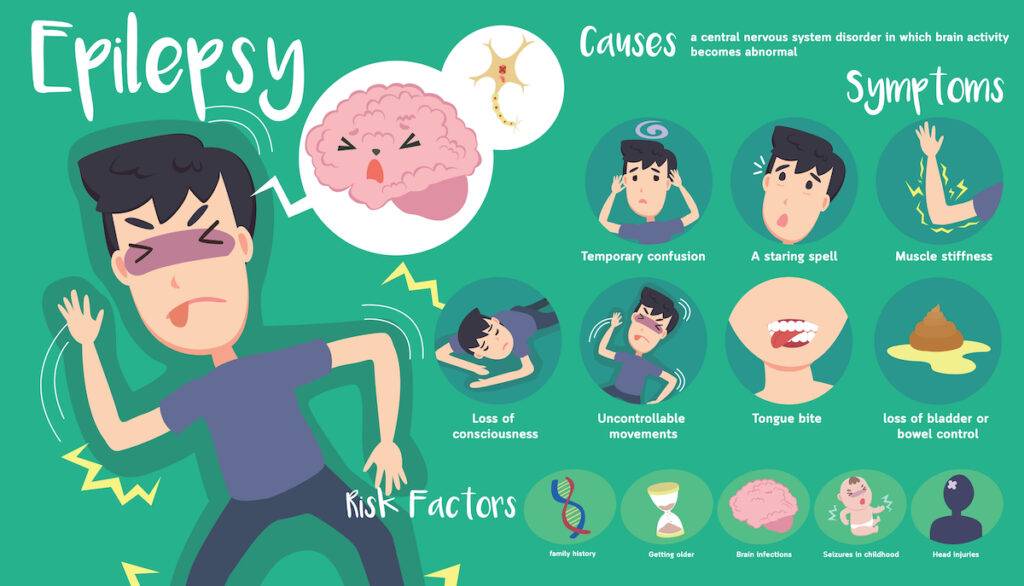
5. **Epilepsy and Sudden Unexpected Death in Epilepsy (SUDEP)**: Epilepsy, a neurological disorder characterized by recurring seizures, carries an increased and deeply concerning risk of death during sleep, specifically through Sudden Unexpected Death in Epilepsy, or SUDEP. This tragic outcome often occurs without warning, and while the exact reasons are not fully understood, research suggests that sleep itself may amplify the risk. For individuals whose seizures are not fully controlled by medication, SUDEP represents the leading cause of death.
According to the Epilepsy Foundation, more than 1 in 1,000 people with epilepsy die each year as a result of SUDEP. The mechanism is believed to involve seizures interfering with critical bodily functions, particularly breathing or heart rhythms. A seizure can cause a person to stop breathing for a period, or it can lead to dangerous cardiac arrhythmias, either of which can be fatal. The body’s state of reduced alertness during sleep means that these life-threatening disruptions may not trigger usual protective reflexes or awaken the individual.
Poorly controlled epilepsy significantly elevates the risk of SUDEP. Moreover, positional factors during sleep, such as lying face down, are thought by some researchers to exacerbate this risk. This highlights the vital importance of consistent medical management for epilepsy. Working closely with doctors and healthcare providers to find an effective treatment plan and meticulously adhering to prescribed medication regimens are crucial steps in mitigating the risk of SUDEP and ensuring safer nights for those living with this condition.

6. **Type 1 Diabetes and “Dead in Bed” Syndrome**: For individuals living with type 1 diabetes, there exists a specific and concerning risk of sudden, unexplained death, frequently occurring during the night. This tragic phenomenon has been colloquially termed “dead in bed” syndrome, a stark description of its manifestation. A 2011 study published in *Diabetic Medicine* revealed that type 1 diabetes significantly increases this risk in young, otherwise healthy individuals, accounting for approximately 6% of all deaths in people under 40 with the condition.
The precise mechanism behind these nocturnal deaths in individuals with diabetes is not yet fully understood, adding to the unsettling nature of the syndrome. However, severe hypoglycemia, or dangerously low blood sugar levels, is strongly suspected as a primary cause. When blood sugar plummets during sleep, it can trigger a cascade of physiological responses, including seizures or severe heart arrhythmias, which can ultimately prove fatal. The body’s reduced awareness during sleep makes it difficult to detect or respond to the critical drop in glucose, leading to a silent emergency.
Furthermore, diabetes is intrinsically linked to heart disease, raising the possibility that some diabetes-related deaths during sleep may be a consequence of abnormal heart rhythms exacerbated by metabolic imbalance. The interplay between glucose control and cardiovascular health is delicate, making vigilant management of type 1 diabetes paramount. Monitoring blood sugar levels before bed and utilizing continuous glucose monitors are invaluable strategies for prevention, empowering individuals to take proactive steps against this silent, nocturnal threat.

7. **Carbon Monoxide Poisoning**: The tranquility of sleep can sometimes conceal an insidious and entirely external threat: carbon monoxide poisoning. This colorless, odorless, and tasteless gas, often dubbed the ‘silent killer,’ is a tragically common cause of accidental nocturnal fatalities. It can be unknowingly released by malfunctioning furnaces, water heaters, dryers, or other common household appliances, transforming a seemingly safe sleeping environment into a dangerous one without any immediate warning.
Carbon monoxide is exceptionally dangerous because it readily binds to red blood cells, far more efficiently than oxygen. This preferential binding starves the body’s tissues and organs, including the vital heart and brain, of the oxygen they desperately need to function. As a result, individuals simply drift into unconsciousness and, eventually, death, never realizing the invisible peril surrounding them. The Centers for Disease Control and Prevention (CDC) provides crucial safety tips and preventive measures for avoiding this silent threat.
The terrifying aspect of carbon monoxide poisoning during sleep is precisely its undetectable nature without proper equipment. Unlike a fire alarm, it emits no sound, smoke, or visual cues. The most effective defense against this hidden danger is proactive prevention: installing carbon monoxide detectors in your home, particularly near sleeping areas, and regularly ensuring they are functioning properly. These devices act as a crucial early warning system, alerting residents to potentially dangerous levels of the gas and offering a vital chance to escape before its fatal effects take hold.

8. **Obstructive Sleep Apnea (OSA)**: While often perceived as a mere nuisance characterized by loud snoring, obstructive sleep apnea (OSA) represents a significant and potentially deadly respiratory obstruction during sleep. This condition involves repeated pauses in breathing as the airway muscles narrow or collapse, temporarily cutting off the oxygen supply. The body’s frantic response to this deprivation includes brief awakenings (often unnoticed by the sleeper), and critically, a dangerous escalation in heart rate and blood pressure, straining the entire cardiovascular system.
The link between OSA and nocturnal death is particularly concerning due to its cascading effects on vital organs. Dr. Sumeet Chugh of Cedars-Sinai’s Heart Rhythm Center highlights that people with OSA may be more than 2.5 times as likely to experience sudden cardiac death between 12 a.m. and 6 a.m. as those without the condition. The intermittent lack of oxygen, coupled with the heightened strain on the heart, significantly increases the risk of cardiac arrhythmias and even heart failure, transforming a sleep disorder into a life-threatening medical emergency. The Sleep Foundation further elucidates the deep connection between obstructive sleep apnea and heart-related risks.
Though OSA itself may not always be the direct cause of death, it is a powerful exacerbating factor for other pre-existing conditions. As Dr. Milind Sovani, a consultant in respiratory medicine, notes, it’s more often related to nocturnal death when it intensifies an underlying problem, such as a heart condition. Managing OSA, often through devices like a Continuous Positive Airway Pressure (CPAP) machine, is paramount. This machine delivers constant and steady air pressure to help maintain an open airway, mitigating the severe risks associated with untreated sleep apnea and helping to prevent tragic nocturnal outcomes.

9. **Other Sleep Disorders and Unforeseen Hazards**: Beyond the more direct physiological threats, certain other sleep disorders, though less commonly fatal on their own, can lead to dangerous and potentially deadly situations. Sleepwalking, for instance, a parasomnia where an individual performs complex actions while asleep, can result in physical trauma or accidental death. People might walk into hazardous environments, fall down stairs, or wander into dangerous situations, all while their consciousness is subdued by slumber.
While the context specifically mentions sleep paralysis as ‘scary but harmless,’ other conditions, though rare, underscore the unpredictable nature of nocturnal hazards. The brain’s reduced vigilance during sleep, as highlighted by cardiologist Jack Flyer, means an individual cannot respond to distress signals or dangerous circumstances as they would while awake. This vulnerability extends to instances where physical trauma might occur, whether self-inflicted during a sleepwalking episode or due to an external, unforeseen event.
The importance of addressing any unusual sleep patterns or disorders cannot be overstated. While death from sleepwalking is uncommon, the potential for serious injury or fatal accidents makes it a concern requiring medical evaluation. Such instances serve as a stark reminder that even seemingly benign sleep oddities can, in rare circumstances, transform into grave dangers when combined with an individual’s unconscious state and their inability to protect themselves from unforeseen perils.

10. **Medications and Substance Use**: The delicate balance of the body’s vital functions during sleep can be profoundly disrupted by certain medications, especially when misused or combined with other substances like alcohol. Opioids and sedatives, for example, are known to suppress the central nervous system, which controls essential processes like breathing and heart rate. Excessive doses of these substances can slow down respiratory function to a dangerously low, even fatal, level, particularly when an individual is deeply asleep and their body’s natural defenses are muted.
The risk of overdose, whether accidental or intentional, is significantly heightened during sleep because the body cannot effectively respond to the toxic load. Combining substances, such as alcohol with prescription sedatives, creates a synergistic effect that can further depress breathing and cardiac activity, leading to critical and often irreversible consequences. The unconscious state of sleep prevents the individual from recognizing the impending danger or seeking help, making it a perilous time for such interactions.
Preventing nocturnal fatalities related to medication and substance use hinges on strict adherence to medical advice and responsible consumption. Always follow your doctor’s dosage instructions meticulously, and never combine medications or mix them with alcohol without explicit medical guidance. Open communication with healthcare providers about all prescribed drugs, over-the-counter remedies, and any recreational substance use is crucial for identifying potential risks and ensuring a safe and restful night.
As we conclude our journey through the complex landscape of nocturnal fatalities, it becomes clear that while the desire for a peaceful passing in one’s sleep is deeply human, the reality is a nuanced interplay of physiology, environment, and individual health. From the silent suffocation of carbon monoxide to the insidious progression of sleep apnea, and the rare, often undiagnosed conditions that compromise vital systems, the night can indeed hold hidden perils. Yet, by understanding these underlying mechanisms, embracing preventative care, and staying attuned to our body’s signals, we empower ourselves to transform the potential for peril into a sanctuary of rest. Every dawn we witness is a testament to the resilience of life, inviting us to live each waking moment fully, reassured by knowledge and vigilance.





