
In the midst of health discussions around chronic illnesses, it’s increasingly important to bring awareness to conditions that aren’t always visible to the naked eye. Often referred to as invisible illnesses, these conditions can have a profound and often debilitating impact on the lives of millions worldwide. Understanding these complex conditions is the first step towards fostering greater support, advancing research, and improving the quality of life for those affected.
One such group of conditions falls under the umbrella term of dysautonomia. This hidden challenge affects over 70 million people globally and has seen increased prevalence following viral infections, including the recent COVID-19 pandemic. While the symptoms can vary widely and often overlap with other conditions, the core issue in dysautonomia lies within the body’s essential automatic functions.
This article aims to shed light on dysautonomia, with a particular focus on one of its most common forms, Postural Orthostatic Tachycardia Syndrome, or POTS. By exploring the intricacies of these conditions, from their definitions and symptoms to the challenges in diagnosis and potential management strategies, we hope to contribute to a clearer understanding and provide valuable information for patients and those who support them.

1. **Dysautonomia: An Invisible Global Challenge**: Dysautonomia is a term used to describe various medical conditions resulting from a malfunction of the autonomic nervous system (ANS). This vital part of your body operates automatically, controlling crucial functions that we don’t consciously think about, such as heart rate, blood pressure, digestion, temperature regulation, and respiratory rate. When the ANS is impaired, these automatic processes can become dysregulated, leading to a wide range of symptoms that are not immediately apparent to onlookers.
Dysautonomia is a term used to describe various medical conditions resulting from a malfunction of the autonomic nervous system (ANS). This vital part of your body operates automatically, controlling crucial functions that we don’t consciously think about, such as heart rate, blood pressure, digestion, temperature regulation, and respiratory rate. When the ANS is impaired, these automatic processes can become dysregulated, leading to a wide range of symptoms that are not immediately apparent to onlookers.
This makes dysautonomia an “invisible illness,” a physical, mental, or neurological condition that significantly impacts a person’s life but isn’t outwardly visible in the way a cast or a wheelchair might be. Despite their invisibility, these conditions require special accommodations and ongoing support. The global prevalence is estimated at over 70 million people, a number that has notably increased following viral infections like COVID-19.
The impact on patients can be profound, affecting multiple systems within the body. According to Lauren Stiles, founder and president of Dysautonomia International, “it’s important for doctors to look at the whole picture of the patient, not just one organ or one system. Which is unfortunately how medicine is broken up now, like the pulmonologist only wants to talk about your lung issues and the cardiologist only wants to talk about your heart issues. But people with Dysautonomia can have issues with all of these systems,” highlighting the systemic nature of the condition and the challenges within a fragmented healthcare system.
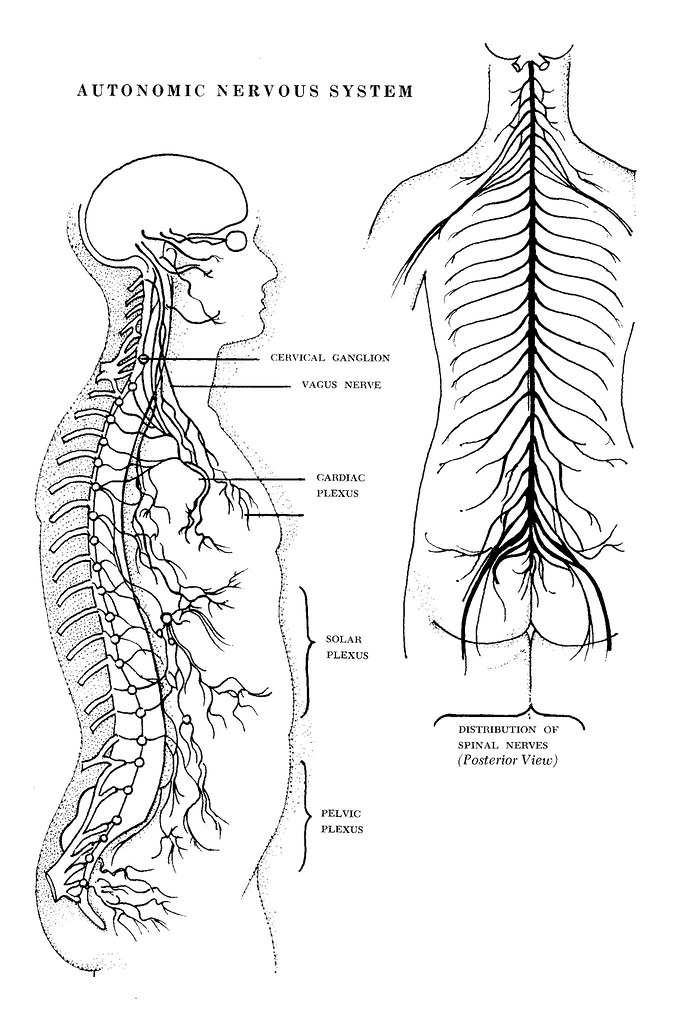
2. **The Autonomic Nervous System: The Body’s Automatic Pilot Gone Awry**: To truly understand dysautonomia, it helps to appreciate the role of the autonomic nervous system (ANS). This intricate network is responsible for regulating involuntary bodily functions, essentially acting as our body’s automatic pilot. It ensures that crucial processes like your heart beating, your lungs breathing, your digestion working, and your body temperature staying stable happen without conscious effort.
To truly understand dysautonomia, it helps to appreciate the role of the autonomic nervous system (ANS). This intricate network is responsible for regulating involuntary bodily functions, essentially acting as our body’s automatic pilot. It ensures that crucial processes like your heart beating, your lungs breathing, your digestion working, and your body temperature staying stable happen without conscious effort.
The ANS is broadly divided into two main branches that typically work in balance: the sympathetic nervous system, often called the “fight or flight” system, which activates during stress or activity, and the parasympathetic nervous system, known as “rest and digest,” which oversees basic functions during calmer periods. “And so, those 2 operate in balance, essentially,” explained Arthur L. Jenkins III, MD, FACS, CEO of Jenkins NeuroSpine.
In cases of dysautonomia, this delicate balance is disrupted, and the ANS malfunctions. As Dr. Jenkins notes regarding one common form, “Sometimes it’s more parasympathetic, like when you’re eating a meal and when you’re sleeping, but then when you’re active and doing things, you need more sympathetic. So, POTS tends to be either overactivity of the parasympathetic, but more frequently, it’s some dysfunction, some under function of the sympathetic.” This imbalance or underfunction leads to dysregulated heart rate, blood pressure, and other automatic functions, resulting in the diverse and challenging symptoms experienced by patients.

3. **Understanding Postural Orthostatic Tachycardia Syndrome (POTS)**: Postural Orthostatic Tachycardia Syndrome, or POTS, is one of the most prevalent forms of dysautonomia and has received increasing attention recently. It is primarily characterized by a significant and abnormal increase in heart rate that occurs when a person changes position, specifically transitioning from lying down to standing up.
Postural Orthostatic Tachycardia Syndrome, or POTS, is one of the most prevalent forms of dysautonomia and has received increasing attention recently. It is primarily characterized by a significant and abnormal increase in heart rate that occurs when a person changes position, specifically transitioning from lying down to standing up.
The diagnostic criterion for POTS is typically met when patients experience a heart rate increase of over 30 beats per minute upon standing within 10 minutes, or over 40 beats per minute for those aged 12 to 19. This rapid increase in heart rate is often accompanied by a collection of symptoms that can be quite debilitating.
POTS is recognized as a condition that throws the body’s natural balancing act into disarray, causing the heart to race unnecessarily upon assuming an upright posture. While it has been historically overlooked, awareness is growing, partly due to high-profile individuals sharing their stories, such as US Olympian Katie Ledecky, who revealed her experience living with the condition in her memoir. POTS may affect up to 1 million individuals in North America, making it a relevant topic as more individuals are diagnosed and seek effective management strategies.

4. **The POTS Patient Experience: A Rollercoaster of Symptoms**: For individuals living with POTS, the experience is often described as navigating a “rollercoaster of symptoms.” These symptoms can be wide-ranging and fluctuating, making daily life unpredictable and challenging. While the defining characteristic is the abnormal heart rate increase upon standing, the impact goes far beyond just a rapid pulse.
For individuals living with POTS, the experience is often described as navigating a “rollercoaster of symptoms.” These symptoms can be wide-ranging and fluctuating, making daily life unpredictable and challenging. While the defining characteristic is the abnormal heart rate increase upon standing, the impact goes far beyond just a rapid pulse.
Common symptoms include dizziness, weakness, and a feeling of being lightheaded, particularly when standing. However, the list of potential symptoms is extensive and can include palpitations, fatigue, brain fog, nausea, tremors, and even fainting. These symptoms can severely impact a patient’s ability to perform everyday tasks, leading to significant disability in some cases.
The variability and sometimes seemingly random nature of symptoms can make the condition particularly frustrating and difficult to manage. Patients often face the added burden of their symptoms being minimized or dismissed. As Dr. Jeffrey Boris, a pediatric cardiologist with extensive experience with POTS patients, points out, “In the paper we just published, anywhere from half to 2/3 of patients were told that their symptoms were in their head. Who needs a doctor to tell you this kind of garbage?” This sentiment is echoed by patients like Kaylin, who experienced a mix of scary, random symptoms for years before finally being diagnosed, finding it “hard to have these issues and be taken seriously for them.”
5. **Identifying POTS Triggers and Risk Factors**: Understanding why POTS develops can be complex, as its causes are varied and not always clear. However, several factors have been identified that can contribute to the onset of the condition. These include genetic predisposition, certain autoimmune disorders, and various viral or bacterial infections.
Understanding why POTS develops can be complex, as its causes are varied and not always clear. However, several factors have been identified that can contribute to the onset of the condition. These include genetic predisposition, certain autoimmune disorders, and various viral or bacterial infections.
Notably, there has been a significant surge in POTS diagnoses among young adults linked to the COVID-19 pandemic, with many reporting long-lasting health issues post-infection. Dr. Jeffrey Boris notes that in his patient series, “56% of patients were able to identify a trigger. That trigger could include infections, concussions, surgery or non-concussion trauma like a fracture.”
Beyond underlying causes and infections, certain demographic factors and life events also appear to play a role. Women are disproportionately affected by POTS, with estimates suggesting that 70% of patients identify as female, often presenting symptoms in their late teens or early twenties. Furthermore, triggers can include significant life stressors, prolonged bed rest, growth spurts, or menarche in younger patients—any situation that puts strain on the body either through physical injury or stress, which can potentially trigger an overactive immune response.

6. **Diagnosing POTS: Navigating a Complex Path**: The journey to receiving a POTS diagnosis is frequently described as long and complicated, presenting significant challenges for both patients and healthcare providers. Due to the wide range of symptoms that overlap with other conditions like anxiety, chronic fatigue syndrome, fibromyalgia, or even dehydration, POTS is often misdiagnosed or goes unrecognized for extended periods.
The journey to receiving a POTS diagnosis is frequently described as long and complicated, presenting significant challenges for both patients and healthcare providers. Due to the wide range of symptoms that overlap with other conditions like anxiety, chronic fatigue syndrome, fibromyalgia, or even dehydration, POTS is often misdiagnosed or goes unrecognized for extended periods.
Many patients endure months or even years of unexplained and debilitating symptoms before receiving a proper diagnosis. The average delay in diagnosis for POTS is estimated to be four years, a period often filled with frustration and doubt as patients struggle to find answers and validation for their experiences. Healthcare providers typically begin the diagnostic process with a thorough review of the patient’s symptoms, medical history, and current medications, followed by a physical examination.
The gold standard test for diagnosing POTS is the tilt table test. This specialized test monitors a patient’s heart rate and blood pressure responses while they are transitioned from a lying-down position to an upright tilt. Additional tests, such as blood and urine analyses, autonomic function tests, and imaging like echocardiograms, may also be utilized to help confirm a POTS diagnosis or rule out other conditions that might be causing the symptoms. The diagnostic process is often lengthy and complex due to a lack of widespread awareness among some medical professionals and the need for specialized testing, which can delay treatment and exacerbate patients’ physical and emotional challenges.

7. **Living with Hypermobility and Ehlers-Danlos Syndrome (EDS)**: While POTS is a common form of dysautonomia, it’s important to recognize that it frequently co-occurs with other conditions. Among these related conditions are hypermobility spectrum disorders and Ehlers-Danlos Syndromes (EDS). These are disorders that affect the body’s connective tissue, the biological glue that holds much of our body together.
While POTS is a common form of dysautonomia, it’s important to recognize that it frequently co-occurs with other conditions. Among these related conditions are hypermobility spectrum disorders and Ehlers-Danlos Syndromes (EDS). These are disorders that affect the body’s connective tissue, the biological glue that holds much of our body together.
Hypermobility is defined as having one or more joints that can naturally move past their typical end range of motion. For some individuals, this enhanced flexibility is not problematic, as seen in professions like circus arts, where it can even be beneficial. However, when hypermobility leads to chronic pain, instability, or other related issues, it is then defined as symptomatic hypermobility or hypermobility spectrum disorder (HSD).
Ehlers-Danlos Syndrome is a group of connective tissue disorders often characterized by significant hypermobility and chronic pain, among other symptoms. A key feature that often distinguishes EDS from HSD is involvement of the skin, which tends to be more elastic, soft, and sometimes more fragile in EDS patients. Physical therapists play a role in identifying hypermobility using normative range of motion values and can recommend further evaluation for EDS if systemic symptoms and skin involvement are present, typically suggesting assessment by a primary care provider or another appropriate specialist.



